Research Article, J Obes Ther Vol: 1 Issue: 1
The Long Term Efficacy of an Intensive Lifestyle Intervention versus Bariatric Surgery to Treat Morbid Obesity in Women
Papalazarou A1, Yannakoulia M1, Gavrieli A1, Kavouras SA2, Komesidou V3, Dimitriadis G4, Papakonstantinou A5 and Sidossis LS1,6*
1Department of Nutrition and Dietetics, Harokopio University, Greece
2Hydration Science Lab, University of Arkansas, USA
3Nutrition Department, Evangelismos General Hospital, Greece
4Department of Internal Medicine, Research Institute and Diabetes Center, “Attikon” University Hospital, Greece
5Department of Surgery, Evangelismos General Hospital, Greece
6Department of Kinesiology and Health, Rutgers University, USA
*Corresponding Author : Labros S. Sidossis
Department of Kinesiology and Health, Department of Medicine, Robert Wood Johnson Medical School, Rutgers University, New Jersey, 70 Lipman Drive, New Brunswick, NJ 08901-8525, USA
Tel: 848-932-9512
E-mail: lss133@rci.rutgers.edu
Received: April 20, 2017 Accepted: May 04, 2017 Published: May 11, 2017
Citation: Papalazarou A, Yannakoulia M, Gavrieli A, Kavouras SA, Komesidou V, et al. (2017) The Long Term Efficacy of an Intensive Lifestyle Intervention versus Bariatric Surgery to Treat Morbid Obesity in Women. J Obes Ther 1:1.
Abstract
Objective: The effectiveness of behavioral/lifestyle interventions in treating morbidly obese individuals is questionable. Aim of the present study was to compare the long-term efficiency of an intensive lifestyle intervention to bariatric surgery in morbidly obese women.
Methods: Twenty-nine morbidly obese females participated in this study. Fifteen subjects were assigned to the Lifestyle Group and 14 underwent vertical banded gastroplasty. Participants in the Lifestyle Group attended 30 behavioral modification sessions over three years, whereas the Surgery Group received the standard of care nutrition after bariatric surgery. Body weight, resting metabolic rate, physical activity, body composition measurements and dietary intake data were assessed repeatedly during the first 3 years postintervention. Body weight and physical activity information were also collected 9 years later.
Results: The Surgery Group lost significantly more weight in the first 3 months, and at 1, 2 and 3 years after surgery compared to the Lifestyle Group (P=0.004). However, at 9 years weight loss was similar between groups. Furthermore, at 9 years, the same percentage (61.5%) of participants in both groups lost and maintained at least 5% of their initial body weight. Physical activity level was more elevated in the Lifestyle Group compared to the Surgery Group throughout the study.
Conclusion: Surgery led to significantly more weight loss than the lifestyle intervention in the first post-intervention years. However, 9 years later both groups ended with similar weight loss, indicating that an intensive lifestyle intervention should not be ignored for treating morbid obesity, as it represent a safe, efficacious and costeffective
approach.
Keywords: Obesity; Lifestyle intervention; Bariatric surgery; Weight loss; Weight maintenance; Diet; Exercise
Introduction
The association of morbid obesity, defined as body mass index (BMI) ≥40 kg/m2, with comorbidities, such as cardiovascular disease, diabetes and cancer, is well established [1]. Bariatric surgery, defined as surgical treatment strategies either to limit energy intake (e.g. adjustable gastric banding sleeve gastrctomy, vertical banded gastroplasty) or to decrease nutrient absorption (e.g. gastric bypass, biliopancreatic diversion), has become very popular the past decades and is currently considered the most effective method to treat morbid obesity [2-4]. However, non-surgical interventions such as diet, exercise, pharmacotherapy and behavioral therapy also report some success in treating moderate to morbid obese individuals [5-10]. Although bariatric surgery offers impressive weight loss when compared to non-surgical approaches [11], especially in the shortterm [12,13], non-surgical approaches may lead to weight loss of clinical significance as well [14,15]. The combination of bariatric surgery and a non-surgical approach may further improve the outcome [16]. In a previous study of our group we showed that the combination of a lifestyle intervention program with vertical banded gastroplasty confers a greater weight loss and maintenance than bariatric surgery alone [17].
Since lifestyle interventions are safer and potentially more cost effective than surgical treatment, our research question was whether an intensive lifestyle intervention was as effective as surgery to treat morbid obesity in the long run. This was achieved by recruiting and following up for 9 years two groups of female volunteers: one that underwent surgery and another one that followed an intensive lifestyle program targeting on the improvement of nutrition and exercise habits, applied through behavior modification techniques such as self-monitoring, self-evaluation, goal setting, reinforcement, stimulus control and relapse prevention. Part of the results of the first three years is presented in a paper published in 2010 [17]. For the purposes of the current paper, some data previously published [17] have been used along with unpublished new and follow-up information on the study participants.
Methods
Subjects and assessment protocol
Twenty-nine morbidly obese females (mean BMI: 47.4 ± 5.4 kg/ m2; age range 21-51 years) who came to the “Evangelismos” General Hospital of Athens, Greece seeking obesity treatment consented to participate in this non-randomized study. Participants’ recruitment took place between 2003 and 2005. Fourteen subjects scheduled to undergo vertical banded gastroplasty were assigned to the Surgery Group and 15 who refused surgery were assigned to the lifestyle intervention. For ethical reasons, the assignment to the two groups was not random. Inclusion criteria for both groups were female sex, age ≥ 18 years, BMI ≥ 40 kg/m2 and absence of mental illness as determined by evaluation by an experienced psychiatrist. Additional inclusion criteria for vertical banded gastroplasty were history of multiple, non-successful, previous attempts for weight loss. The study protocol was approved by the Harokopio University Ethics Committee. All subjects were informed about the purpose of the study and signed written consent prior participation.
Participants of the Surgery Group underwent vertical banded gastroplasty in the “Evangelismos” General Hospital of Athens. They followed a standard dietary treatment, subscribed for the first post-operation months, while no further treatment was provided thereafter. Subjects in the Lifestyle Group visited the Nutrition Department of the hospital for 30 intervention sessions conducted over 3 years: weekly for the first 3 months, every other week for the next 3 months, monthly for the following 6 months, every 3 months for the second year and every 6 months during the third year. Nine years (104-117 months) later (in 2013) follow-up data for specific variables (body weight and physical activity) were obtained from both groups through a telephone interview.
Components of the interventions
The main purpose of the lifestyle intervention was to educate participants to achieve weight management by adopting healthier eating habits and increasing physical activity. Individually tailored treatment was used by a trained dietician, incorporating behavior modification techniques such as self-monitoring, self-evaluation, goal setting, reinforcement, stimulus control and relapse prevention. Each session lasted 40 minutes and consisted of three parts: nutrition education, eating behavior changes and physical activity changes. Information was provided on fat and fiber sources, nutritional value of foods and the health benefits of adopting a balanced dietary pattern and increasing physical activity. Participants were encouraged to eat breakfast, increase consumption of fruits and vegetables, reduce intake of high energy density foods including fast food, sweets and sauces. They were advised to adopt a more physically active lifestyle, identify external and internal stimuli related to eating and were offered manageable short-term goals. The content of each session was individualized according to each patient’s needs in order to increase participants’ adherence. Furthermore, the Lifestyle Group participants were instructed to follow a 5.0 MJ/day diet for 1 year. Targeted macronutrient composition was 55% carbohydrates, 30% fat and 15% protein.
Subjects in the Surgery group underwent surgery and then were instructed to follow a liquid diet of very low calorie content (2.8 MJ, 66 g protein/day, 100% RDA for vitamins and minerals) for four weeks post-operatively. This was followed by gradual introduction of soft and solid foods to their diet. By the end of the sixth month, most subjects had adopted conventional dietary habits.
Anthropometric assessment
Body weight and height were measured at baseline and at each assessment visit, using a calibrated scale and a stadiometer, to the nearest 0.5 kg and 0.5 cm respectively, with the subject lightly dressed and barefoot. Nine years later, self-reported information on weight and height was obtained. BMI was calculated as weight divided by height squared (kg/m2). Percent excess weight loss was computed as: [weight loss (kg) /excess weight (kg)] x100, where excess weight (kg) = weight pre-operatively (kg) – 25 x height (m) x height (m). Monthly weight loss rate was calculated as: [weight pre (kg) -weight post (kg)]/n months, where n the number of months of the particular period.
Resting metabolic rate
Resting metabolic rate was estimated by indirect calorimetry (Vmax229D; Sensormedics, Yorba Linda, CA) after an overnight fast at baseline, 3 months, 1 and 3 years post-intervention. Subjects were instructed to drink only water for 12 hours before testing and were requested to avoid physical exertion on the day before measurement. Subjects rested for 20 minutes before calorimetry. Gas concentrations were measured using the ventilated hood technique during a 40-minute period. The first 10 minutes were considered an acclimatization period.
Body composition
Body composition was determined by bioelectrical impedance analysis at baseline, 3 months, 1 and 3 years. Resistance (R) and reactance (Xc) were measured by a single investigator with a singlefrequency 50 kHz bioelectrical impedance analyzer (bioelectrical impedance analysis 101 RJL, Akern Bioresearch, Firenze, Italy). Body composition was measured by using validated equations for total body water, fat mass and fat free mass [18,19]. The ratio of fat free mass loss to weight loss was also calculated [(fat free mass pre – fat free mass post) x 100 / (weight pre – weight post)].
Physical activity
Assessment of physical activity was performed at baseline, 3 months, 1, 3 and 9 years post-intervention, using a brief, self-reported questionnaire validated for Greek population (Harokopio Physical Activity Questionnaire) [20]. The questionnaire examines the time spent over a week in light-, moderate-, and high-intensity activities. It is based on the metabolic equivalents of all activities of the week, including activities at work, leisure time, and rest or sleep. The questionnaire allows the prediction of a mean physical activity level by dividing total energy expenditure to resting metabolic rate. The higher the physical activity level the more active the lifestyle.
Statistical analysis
Data are presented as mean ± standard deviation (SD) or as percentages. Baseline characteristics were compared either through t-test for independent samples in case of continuous variables or through chi square test in case of qualitative characteristics. Body weight, BMI, weight loss, monthly weight loss rate, % excess weight loss, resting metabolic rate, physical activity level, fat free mass, fat mass, fat free mass loss/weight loss, fruit, vegetable and sweet consumption, energy and macronutrient intake over time were analyzed through repeated measures analysis of variance. Adjustment for both baseline weight and age was made in the analysis of weight loss. The percentage of participants who lost above 5 or 10 % of their initial body weight was analyzed through the chi square test (yes/no). Significance was set at P≤0.05. Data analysis was performed using standard software (Statistical Package for the Social Sciences, version 18.0 for Windows, SPSS, Inc., Chicago, IL).
Results
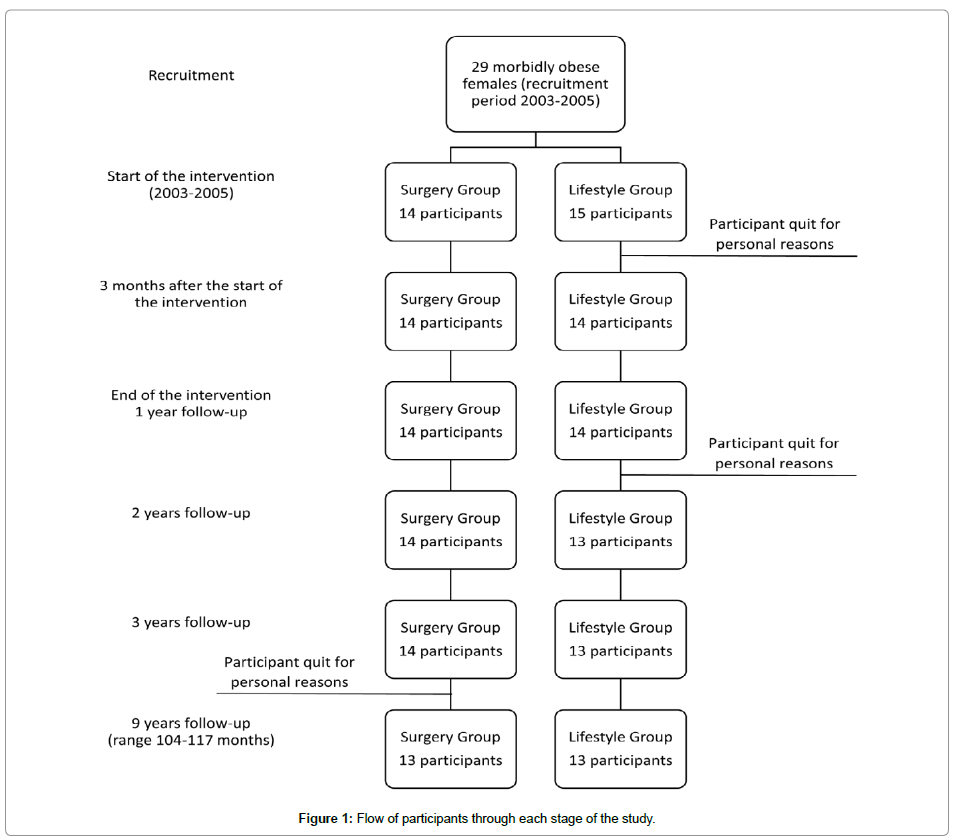
Twenty nine females were found eligible and were enrolled in the study (participants’ recruitment took place between 2003 and 2005). Fourteen individuals were allocated in the Surgery Group and 15 to the Lifestyle Group. Thirteen individuals from each group completed the 9-year follow-up (range: 104-117 months) in 2013 (Figure 1). All participants who left the study quit for personal reasons and no difference was observed between the participants who completed the study and those stopped at all baseline characteristics. No deviation from the study protocol occurred.
Baseline characteristics did not differ between groups, although the Surgery Group had slightly higher BMI than the Lifestyle Group (Table 1). The Surgery Group lost significantly more weight after 3 months (P<0.001), 1 (P=0.001), 2 (P=0.003) and 3 years (P=0.03) post-intervention compared to the Lifestyle Group (Figure 2). However, 9 years later weight loss was similar between groups. The greater weight loss the Surgery Group presented during the first 3 years, can be mostly attributed to the higher weight loss rate this group achieved during the first 3 months (p<0.001) (Table 2). While both groups continued to lose weight for the remainder of the first year, subsequent weight loss rates did not differ significantly between the two groups [3 months to 6 months: 1.56 ± 0.97 kg/mo (Surgery Group) vs. 2.72 ± 2.25 kg/mo (Lifestyle Group), P=0.10 and 6 months to 1 year: 1.02 ± 0.76 kg/mo (Surgery Group) vs. 0.57 ± 0.83 kg/mo (Lifestyle Group), P=0.17]. On the other hand, the greater 3-9 year weight gain rate the Surgery Group presented (P=0.01) substantiates the finding of the similar weight loss observed at 9 years between the two groups. Accordingly, % excess weight loss was significantly higher for the Surgery Group compared to the Lifestyle Group during the first 3 years (P<0.05), but did not differ between groups 9 years postintervention (Table 2). Furthermore, at 9 years a similar percentage of participants (61.5%) of both groups lost and maintained above 5% of their initial body weight, while 53.8% and 38.5% of the participants of the Surgery Group and the Lifestyle Group, respectively, lost and maintained over 10% of their initial body weight.
| Characteristic | Surgery Group | Lifestyle Group | P-value |
|---|---|---|---|
| Age (y) | 33.4 ± 8.1 | 33.5 ± 11.2 | 0.99 |
| Weight (kg) | 132.5 ± 16.7 | 122.6 ± 15.5 | 0.11 |
| BMI (kg/m2) | 49.4 ± 5.6 | 45.5 ± 4.8 | 0.06 |
| Being married (%) | 35.7 | 33.3 | 0.76 |
| Education level ≥12 years (%) | 71.4 | 73.3 | 0.91 |
| Parental obesity | |||
| One parent obese/overweight (%) | 71.4 | 86.7 | 0.31 |
| Both parents obese/overweight (%) | 28.6 | 13.3 | 0.31 |
Abbreviations: Body mass index (ΒΜΙ)
Table 1: Baseline characteristics of the Surgery and Lifestyle Groups.
| Baseline | 3 months | 1 year | 2 years | 3 years | 9 years# | P-trend | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | ||
| d_Weight (kg) | n/a | n/a | -26.5 ± 3.1 | -14.3 ± 25.9 | -36.9 ± 6.9 | -25.1 ± 24.6 | -34.5 ± 10.2 | -31.2 ± 36.0 | -31.9 ± 11.0 | -30.6 ± 36.3 | -24.1 ± 31.4 | -25.5 ± 38.5 | 0.63 |
| d_BMI (kg/m2) | n/a | n/a | -9.9 ± 1.0 | -5.5 ± 10.4 | -13.7 ± 2.1 | -9.5 ± 10.1 | -12.8 ± 3.4 | -11.7 ± 13.5 | -11.9 ± 3.9 | -11.4 ± 13.6 | -9.4 ± 13.4 | -9.5 ± 14.5 | 0.52 |
| Weight loss rate (kg/mo)‡ | n/a | n/a | 8.92 ± 1.02 | 2.61 ± 3.17* | 1.20 ± 0.61 | 1.29 ± 0.95 | -0.16 ± 0.40 | -0.08 ± 1.13 | -0.32 ± 0.52 | -0.06 ± 0.12 | -0.18 ± 0.14 | -0.07 ± 0.07* | <0.001 |
| Excess weight loss (%) | n/a | n/a | 42.8 ± 9.4 | 14.8 ± 20.5* | 59.9 ± 15.9 | 33.9 ± 23.1* | 56.1 ± 16.6 | 32.2 ± 23.5* | 49.1 ± 15.1 | 31.0 ± 23.7* | 25.6 ± 19.5 | 19.6 ± 24.5 | 0.008 |
| Participants lost ≥ 5% initial weight (%) | n/a | n/a | 100.0 | 28.6* | 100.0 | 92.9 | 100.0 | 92.3 | 100.0 | 84.6 | 61.5 | 61.5 | - |
| Participants lost ≥ 10% initial weight (%) | n/a | n/a | 100.0 | 21.4 | 100.0 | 64.3 | 100.0 | 46.2 | 92.9 | 53.8 | 53.8 | 38.5 | - |
Abbreviations: Body mass index (ΒΜΙ); not applicable (n/a)
#9 years: 107.9 ± 3.9 months, range 104-117 months
*significantly different from the Surgery Group, P ≤ 0.05
‡monthly weight loss rate for each two-time-point period
Table 2: Changes in body weight parameters between the Surgery and Lifestyle Groups.
Post-intervention physical activity was increased and maintained at a significantly higher rate in the Lifestyle Group compared to the Surgery Group, even 9 years later (P<0.001) (Table 3). Resting metabolic rate was significantly reduced in the Surgery Group compared to the Lifestyle Group at 1 (P=0.009) and 3 years (P=0.001), whereas body composition, as determined by fat mass and fat free mass did not differ between the groups at any of the available time-points (Table 3).
| Baseline | 3 months | 1 year | 3 years | 9 years# | P-trend | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | Surgery Group | Lifestyle Group | ||
| d_Resting metabolic rate (MJ/d) | n/a | n/a | -1.7 ± 1.2 | -0.9 ± 1.1 | -2.1 ± 1.2 | -0.8 ± 0.9* | -2.2 ± 1.1 | -0.7 ± 0.9* | n/a | n/a | 0.17 |
| d_Physical activity level | n/a | n/a | 0.11 ± 0.08 | 0.20 ± 0.38* | 0.16 ± 0.13 | 0.40 ± 0.70* | 0.06 ± 0.10 | 0.40 ± 0.86* | -0.04 ± 0.38 | 0.35 ± 0.56* | <0.001 |
| d_Fat free mass (kg) | n/a | n/a | -5.8 ± 2.5 | -1.0 ± 0.6 | -9.5 ± 6.1 | -6.5 ± 6.2 | -9.6 ± 7.2 | -3.3 ± 3.9 | n/a | n/a | 0.70 |
| d_Fat mass (kg) | n/a | n/a | -20.8 ± 3.5 | -13.0 ± 8.7 | -27.4 ± 5.3 | -14.8 ± 9.4 | -22.2 ± 7.3 | -12.7 ± 5.7 | n/a | n/a | 0.56 |
| Fat free mass loss/weight loss (%) | n/a | n/a | 21.8 ± 10.1 | 13.6 ± 6.3* | 23.9 ± 12.2 | 19.1 ± 7.1 | 22.6 ± 7.0 | 18.2 ± 8.6 | n/a | n/a | 0.06 |
Data are presented as mean ± SD, n/a: not applicable or not available
#9 years: 107.9 ± 3.9 months, range 104-117 months
*significantly different from the Surgery Group, P ≤ 0.05
Table 3: Resting metabolic rate, physical activity level and body composition changes between the Surgery and Lifestyle Groups.
Discussion
To the best of our knowledge, this is one of the few studies to compare the effects of a lifestyle intervention and a restrictive type of bariatric surgery on weight loss and maintenance in a group of morbidly obese women over a long-term period i.e. 9 years. Surgery resulted in greater weight loss during the first post-intervention years compared to the lifestyle intervention, although the weight loss achieved in the Lifestyle Group was of clinical significance (≥ 5% initial weight loss). Despite the superiority of bariatric surgery in the first post-operative years we found that in the long-term, both approaches lead to comparable results. Furthermore, females in the Lifestyle Group engaged in higher physical activity throughout the 9 years. Overall, our data suggests that a well-designed, intense lifestyle intervention program can result in clinically significant weight loss and predictable long-term weight maintenance.
Both groups lost a significant amount of weight during the first year post-intervention, which was maintained over the next 2 years. However, surgery demonstrated far greater weight reduction. Previous studies confirm the short-term effectiveness of bariatric surgery over conservative therapies [21,22] as well as the fact that the weight loss achieved through non-surgical approaches can be of clinical significance [23,24]. This was also the case in the present study: 84.6% and 53.8% of the Lifestyle Group participants lost and maintained ≥5% and ≥10% of their initial body weight, respectively, 3 year post-operatively.
The greater effectiveness of surgical treatments over lifestyle interventions for the management of morbid obesity has not yet been firmly established in the long term, although some publications are suggestive of this [25,26]. Other studies, however, indicate that behavioral modification techniques can result in sustainable longterm weight loss for 8 [15] or 10 years [27]. Our study shows that 9 years post-intervention, the weight loss in the Surgery Group was only 4.5 kg more than in the Lifestyle Group suggesting that both approaches may lead to comparable results in the long-term. Contrary to the findings of this study, the SOS study presented a greater effectiveness for bariatric surgery over non-surgical interventions 20 years later [28]. However, in the SOS study, the control group received either sophisticated lifestyle interventions and behavior modification or no treatment at all, rendering difficult the direct comparison with our study. Furthermore, another research group showed that the effectiveness of bariatric surgery over the long-term relies mostly on significant lifestyle modification and particularly on the improvement of nutrition and exercise habits [29]. This is also supported by the systematic review and meta-analysis carried out by Rudolph and Hilbert [30].
Evidence show that it is more difficult to lose and maintain weight loss following a lifestyle intervention program compared to surgical intervention [23]. However, Bond et al. [31] reported no difference between morbidly obese subjects who lost weight with either surgery or other conventional approaches at 1 year. In our study, the two groups were equally able to maintain their weight loss for up to 3 years while the Lifestyle Group was proven more resistant to gain weight 9 years post intervention. This may be explained, at least partly, by the fact that the Surgery Group had lower resting metabolic rate at the 3 years compared to the Lifestyle Group. We did not collect resting metabolic rate data at the 9 year follow-up but if it was maintained lower during the next 6 years, this could indicate a greater difficulty of the Surgery Group to maintain weight loss in the long-term. This is further supported by the fact that at 9 years the participants underwent surgery reported less physical activity than the participants underwent lifestyle modification.
This is one of the few studies comparing bariatric surgery to lifestyle intervention outcomes over a prolonged period of time. Furthermore, this study was carried out in a real world setting, adopting real life clinical practices. However, since the 9 year followup was performed through a telephone interview, we were not able to gather all the data collected during the first 3 years of the study. Another study limitation is the self-reported body weight and height at the 9 year follow-up as well as the non-randomized design of the trial. However, research designs of this type could not easily use randomization procedures..
Conclusion
Our data suggests that although bariatric surgery (vertical banded gastroplasty) results in better weight loss over the first post-operation years compared to an intensive lifestyle intervention, the superiority of bariatric surgery in weight maintenance fades away in the long run. An intensive lifestyle intervention could be more efficient in weight loss maintenance after 9 years compared to bariatric surgery when no further intervention is being made. This could potentially occur through improved physical activity levels and possibly through improvements in other factors like metabolic parameters or dietary habits not evaluated herein. Therefore, intensive lifestyle interventions should not be ignored as a potential modality for treating morbid obesity, as they can represent a safe, efficacious and cost-effective approach.
Acknowledgements
We would like to thank the volunteers for their participation and the staff at the Laboratory of Nutrition and Clinical Dietetics, for expert support.
References
- Noria SF, Grantcharov T (2013) Biological effects of bariatric surgery on obesity-related comorbidities. Can J Surg 56: 47-57.
- Albaugh VL, Flynn CR, Tamboli RA, Abumrad NN (2016) Recent advances in metabolic and bariatric surgery. F1000Res 5: 978.
- Hankey CR (2010) Session 3 (Joint with the British Dietetic Association): Management of obesity: Weight-loss interventions in the treatment of obesity. Proc Nutr Soc 69: 34-38.
- Dixon JB, Straznicky NE, Lambert EA, Schlaich MP, Lambert GW (2012) Laparoscopic adjustable gastric banding and other devices for the management of obesity. Circulation 126: 774-785.
- Danielsen KK, Svendsen M, Maehlum S, Sundgot-Borgen J (2013) Changes in body composition, cardiovascular disease risk factors, and eating behavior after an intensive lifestyle intervention with high volume of physical activity in severely obese subjects: a prospective clinical controlled trial. J Obes 2013: 325464.
- Ryan DH, Johnson WD, Myers VH, Prather TL, McGlone MM, et al. (2010) Nonsurgical weight loss for extreme obesity in primary care settings: results of the Louisiana Obese Subjects Study. Arch Intern Med 170: 146-154.
- Ling H, Lenz TL, Burns TL, Hilleman DE (2013) Reducing the risk of obesity: defining the role of weight loss drugs. Pharmacotherapy 33: 1308-1321.
- Anderson JW, Grant L, Gotthelf L, Stifler LT (2007) Weight loss and long-term follow-up of severely obese individuals treated with an intense behavioral program. Int J Obes (Lond) 31: 488-493.
- Igel LI, Kumar RB, Saunders KH, Aronne LJ (2017) Practical Use of Pharmacotherapy for Obesity. Gastroenterology 152: 1765-1779.
- Telles S, Gangadhar BN, Chandwani KD (2016) Lifestyle Modification in the Prevention and Management of Obesity. Journal of obesity 2016: 5818601.
- Picot J, Jones J, Colquitt JL, Gospodarevskaya E, Loveman E, et al. (2009) The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess 13: 1-190.
- Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, et al. (2013) Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 347: 5934.
- Cunneen SA (2008) Review of meta-analytic comparisons of bariatric surgery with a focus on laparoscopic adjustable gastric banding. Surg Obes Relat Dis 4: 47-55.
- Wadden TA, Butryn ML, Wilson C (2007) Lifestyle modification for the management of obesity. Gastroenterology 132: 2226-2238.
- Look AHEAD Research Group (2014) Eight-year weight losses with an intensive lifestyle intervention: The look AHEAD study. Obesity (Silver Spring) 22: 5-13.
- Kalarchian MA, Marcus MD, Courcoulas AP, Lutz C, Cheng Y, et al. (2016) Structured dietary intervention to facilitate weight loss after bariatric surgery: A randomized, controlled pilot study. Obesity 24: 1906-12.
- Papalazarou A, Yannakoulia M, Kavouras SA, Komesidou V, Dimitriadis G, et al. (2010) Lifestyle intervention favorably affects weight loss and maintenance following obesity surgery. Obesity (Silver Spring) 18: 1348-1353.
- Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI (1985) Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 41: 810-817.
- Kotler DP, Burastero S, Wang J, Pierson RN Jr. (1996) Prediction of body cell mass, fat-free mass, and total body water with bioelectrical impedance analysis: effects of race, sex, and disease. Am J Clin Nutr 64: 489-497.
- Kollia M, Gioxari A, Maraki M, Kavouras SA (2006) Development, validity and reliability of the Harokopio Physical Activity Questionnaire in Greek adults. Proceedings of the 8th Panhellenic Congress on Nutrition and Dietetics.
- Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev 8: 003641.
- Sundstrom J, Bruze G, Ottosson J, Marcus C, Naslund I, et al. (2017) Weight Loss and Heart Failure: A Nationwide Study of Gastric Bypass Surgery Versus Intensive Lifestyle Treatment. Circulation.
- Hofso D, Nordstrand N, Johnson LK, Karlsen TI, Hager H, et al. (2010) Obesity-related cardiovascular risk factors after weight loss: a clinical trial comparing gastric bypass surgery and intensive lifestyle intervention. Eur J Endocrinol 163: 735-745.
- Martins C, Strommen M, Stavne OA, Nossum R, Marvik R, et al. (2011) Bariatric surgery versus lifestyle interventions for morbid obesity--changes in body weight, risk factors and comorbidities at 1 year. Obes Surg 21: 841-849.
- O'Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257: 87-94.
- Hsieh T, Zurita L, Grover H, Bennett A, Farrokhyar F, et al. (2013) 10-Year Outcomes of the Vertical Transected Gastric Bypass for Obesity: a Systematic Review. Obes Surg 24: 456-461.
- Bjorvell H, Rossner S (1992) A ten-year follow-up of weight change in severely obese subjects treated in a combined behavioural modification programme. Int J Obes Relat Metab Disord 16: 623-625.
- Sjostrom L (2013) Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med 273: 219-234.
- Keren D, Matter I, Lavy A (2013) Lifestyle Modification Parallels to Sleeve Success. Obes Surg 24: 735-740.
- Rudolph A, Hilbert A (2013) Post-operative behavioural management in bariatric surgery: a systematic review and meta-analysis of randomized controlled trials. Obes Rev 14: 292-302.
- Bond DS, Phelan S, Leahey TM, Hill JO, Wing RR (2009) Weight-loss maintenance in successful weight losers: surgical vs non-surgical methods. Int J Obes (Lond) 33: 173-180.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi