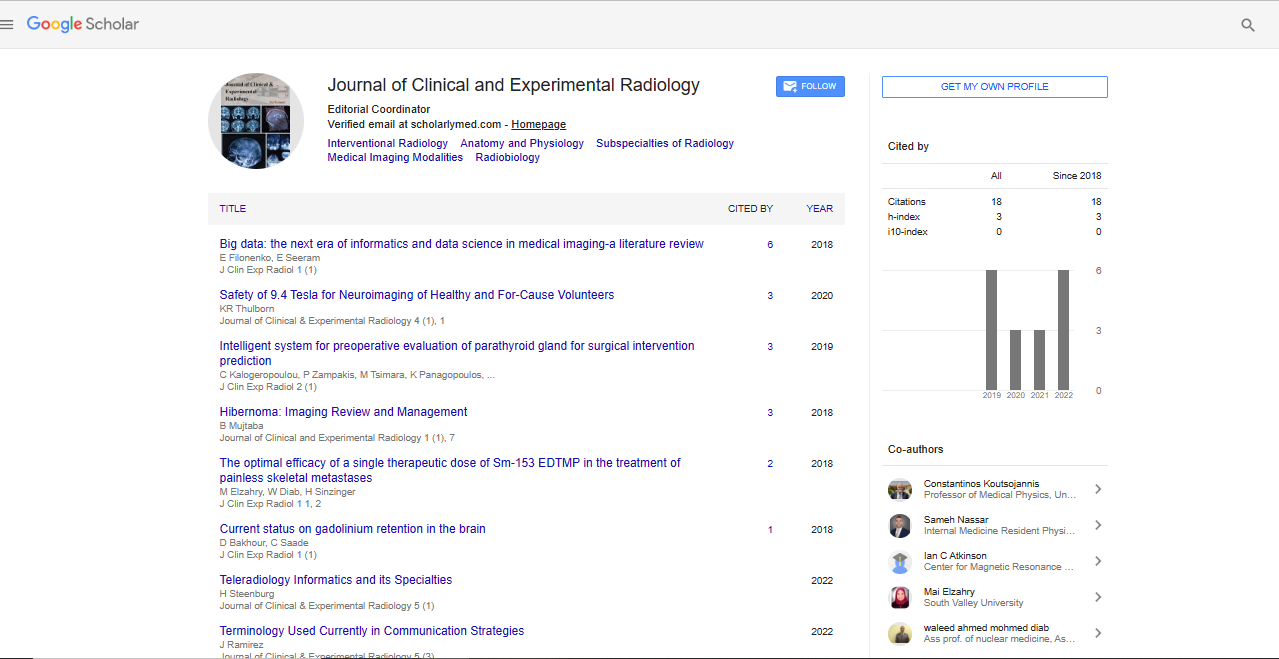
Research Article, J Clin Exp Radiol Vol: 2 Issue: 1
Intelligent System forPreoperative Evaluation of Parathyroid Gland for surgical intervention Prediction
Kalogeropoulou Christina1*, Zampakis Petros1, Tsimara Maria1, Panagopoulos Konstantinos2, Hatzilygeroudis Ioannis3 and Koutsojannis Constantinos4
1Department of Radiology, University of Patras
2Department of Surgery, University of Patras
3Computer Engineering & Informatics Department, University of Patras
4Health Physics and Computational Intelligence Lab, TEI of Western Greece
*Corresponding Author : Kalogeropoulou Christina
Department of Radiology, University of Patras, Greece
Tel: 2691022058
E-mail: ckrat@upatras.gr
Received: January 28, 2019 Accepted: February 12, 2019 Published: February 19, 2019
Citation: Christina K, Petros Z, Maria T, Konstantinos P, Ioannis H, et al. (2019) Intelligent System for Preoperative Evaluation of Parathyroid Gland for Surgical Intervention Prediction. J Clin Exp Radiol 2:1.
Abstract
Background: According to previous studies, CT scan exhibits the highest sensitivity and specificity rates among the imaging methods for parathyroid glands. The purpose of this work is the development and evaluation of an intelligent decision support system for the appropriate surgical intervention of parathyroid gland based on the evaluation of CT images for preoperative mapping. additionally to the traditional technique in distinguishing mono/multiglandular parathyroid pathology assisting precise preoperative localization of adenomas or hyperplasia and offering the best choice for minimal or extensive surgical exploration. Methods: Based on simple clinical and CT imaging information and criteria such as CT diagnosis, location of enlarged parathyroid gland, density in ΗU before IV contrast enhancement, increase of enhancement, volume of pathological parathyroid and final surgical results, data mining algorithms were used to develop the knowledge base for decision making. As training data the records from 118 histologically proven PHPT patients referred to our Hospital University Department of Radiology-Computer Tomography were used on a retrospective chart analysis. As test database the records from histologically proven PHPT patients were used. Results: The final developed intelligent system produced succeeded to predict an acceptable outcome for all participants who emerged surgical therapy and compared to the surgical results revealed minimal false positive rate and excellent positive and negative likelihood ratios. Conclusion: The final intelligent system has provided better performance than the commonly used imaging criteria in predicting the surgical of multi- or single-glandular disease.
Keywords: Parathyroid; Multi- or single-glandular; Preoperative CT imaging; minimal invasive parathyreoidectomy; Machine learning
Keywords
Parathyroid; Multi- or single-glandular; Preoperative CT imaging; minimal invasive parathyreoidectomy; Machine learning
Introduction
Hyperparathyroidism is a condition in which one or more of the parathyroid glands become overactive elevating the levels of calcium in the blood, and causing hypercalcemia. In many instances, a person who has hyperparathyroidism doesn’t have any symptoms. A person who has mild hyperparathyroidism may have joint pain, muscle weakness, fatigue, depression, etc. More severe cases of hyperparathyroidism may produce confusion, nausea and vomiting, etc. Finally high blood pressure occurs more commonly in people with hyperparathyroidism and may need to be treated whether or not specific treatment is recommended for the hyperparathyroidism. For primary hyperparathyroidism, diagnosis MDCT is clinically used that is a multiphase (4D or 2D) imaging technique, for accurate localization of parathyroid pathologic tissue finally providing the introduction of minimally invasive techniques in most of the cases [1].
Today and according to the existed literature approximately 90% of the patients with primary hyperparathyroidism have a single parathyroid adenoma, 10% have multiglandular adenomatous disease, and very rarely a number of them have parathyroid carcinoma [2]. Available imaging techniques consist of Computed Tomography (CT), ultrasound, radionuclide scanning and Magnetic Resonance Imaging (MRI) and “4D” or “2D” [3,4]. Imaging is performed in order to identify: a) the site of enlarged parathyroid gland and b) the type of the pathology. This requirement for increasingly more accurate preoperative localization of adenomatous parathyroid tissue has been driven by the recent evolving surgical approach to this disease [5]. Using improved preoperative imaging and having available the intraoperative parathyroid hormone (IOPTH) monitoring, standard cervical (or “4-gland”) exploration has given way to “minimally invasive” parathyroidectomy (DIP) for the treatment of single-gland disease and not only. Otherwise DIP is more invasive or without any results. The previously presented imaging techniques that are used nowadays offered a great help in preoperative mapping although each one has its own limitations. Ultrasonography presents excellent evaluation of superficial lesions but the small lesions, the ectopic site or postoperative necks are the main limiting factors [6]. Addition of Contrast-Enhanced Ultrasonography (CEUS) presented controversial results and still remains to be evaluated [7,8]. A number of studies revealed 99mTc-MIBI-SPECT/CT (MIBI-SPECT/CT) in correctly localizing single parathyroid.
Adenomas in patients with negative US, although without the appropriate anatomic information plus that sensitivity of method is still low in case of the multiglandular type of the disease, concurrent thyroid disease or reduced radiotracer retention. C-methionine Positron Emission tomography/computed tomography (Met-PET/ CT) is a very promising method in patients with negative US and MIBI-SPECT/CT [9]. Additionally MRI diagnosis depends on the knowledge of the typical morphology and location of the parathyroid glands and common sites of ectopic glands. It seems to be effective in locating remaining abnormal parathyroid tissue [10]. The multipara metric MR perfusion can distinguish parathyroid adenomas from the subjacent thyroid tissue or lymph nodes with very high diagnostic accuracy [11]. Finally, CT scan has shown in several studies, superior accuracy and better effectiveness as ultrasonography, scintigraphy or MR imaging being a valuable tool for preoperative planning though the radiation dose remains high, 5.2 mSv in case of 2D CT and 27 mSv of 4D CT [12,13]. CT examination consists of axial acquisitions, sagittal and coronal reformatted images and the enhancement modification comparing non-contrast images to after contrast enhancement imaging and today demonstrates a high diagnostic accuracy for single gland disease and high specificity in multigland disease. Some of the limitations of the method are the radiation exposure, the necessity of iodinated contrast media, the technical challenges and the expertise in anatomic knowledge.
To expose the patient to less radiation, in our institution we performed and studied 2D-CT in a cohort of 81 patients with established primary hyperparathyroidism, to demonstrate the pathology and site of enlarged parathyroid gland. We concluded that 2D-CT scan offers a same sensitivity, specificity and accuracy to 4DCT. A novel positioning mapping was included in our study combined with the parathyroid classification system as follows: a type A gland is a “normal” superior gland in proximity to the posterior surface of the thyroid or even compressed within the capsule of the thyroid. A type B gland is a superior parathyroid gland fallen posteriorly into the trachea-esophageal groove, in the plane of the superior pole of the thyroid. There is minimal or no contact between the gland and the posterior surface of the thyroid. Αs B+ glands are referred those near the carotid bifurcation or mandible. A type C gland is a superior gland that has fallen posteriorly into the tracheoesophageal groove and lies at the level of or below the inferior pole of the thyroid, posterior to the RLN. The type D gland lies in the mid region of the posterior surface of the thyroid parenchyma, near the junction of the RLN and the inferior thyroid artery. The type D gland may be either asuperior or inferior gland, depending on its exact relationship to the nerve. The type E gland is an inferior gland in close proximity to the inferior pole of the thyroid gland, anterior to the trachea. The type of gland is an inferior gland descended into the thyrothymic ligament, superior thymus, “ectopic” or within the mediastinum. Finally, the type G gland is a rare intrathyroidal parathyroid gland [14,15]. As a result, based on several studies, CT scan exhibits the highest sensitivity and specificity rates among the imaging methods for parathyroid glands. However, assisting an automated diagnosis system was thought to increase the likelihood of pathology and the distinction between hyperplasia and simple adenoma.
The purpose of this article is to describe the role of Artificial Intelligence techniques additionally to the traditional MDCT technique in distinguishing mono/multiglandular parathyroid pathology assisting precise preoperative localization of adenomas or hyperplasia and offering the best choice for minimal or extensive surgical exploration.
A.I. is approved as a forceful computational method that may better than statistics describe non deterministic associations between different parameters in the plethora of medical databases [16,17]. AI has found medical applications as in cancer survival prediction and in some studies has demonstrated greater accuracy over traditional approaches [18,19]. Machine Learning includes a number of Artificial Intelligence approaches, mainly consisted of Data Mining tools, aiming Knowledge extraction from data concerning well defined instances of a situation. In medicine medical knowledge extraction is presented as a type of decision tree or production rules [20,21].
The purpose of this article is to use for the first time, the appropriate approaches of Artificial Intelligence based on the traditional MDCT technique in distinguishing mono from multiglandular parathyroid pathology assisting precise preoperative localization of adenomas or hyperplasia offering the choice for precise minimal or extensive surgical exploration [22-24].
Patient and Methods
At the beginning a retrospective study of 230 patients with biochemically confirmed PHPT, was performed at our university hospital. Each patient has undergone 2D-CT with pre- and postcontrast images preoperatively. The results of the computed tomography imaging were compared with operative and histological data, calculating the sensitivity and specificity of our method. Based on the final results, we developed a novel assistant intelligent automated method to discriminate adenomas and hyperplasia, as additional tool to preoperative evaluation and planning a minimally directed parathyroidectomy.Patient population and data collection.
A group of population consisted of 31 men and 199 women referred to our University department of Radiology, section of Computed Tomography in the period 2010-16, for neck CT scanning to reveal parathyroid pathology and guiding preoperative mapping. The inclusion criteria for pre-operative diagnosis of PHPT based on elevated serum calcium>10,2 mg/dl and serum PHT >30 pg/mL. All the patients that have included in our retrospective analysis have finally undergone surgical exploration submitting tissues for final histological report offering available comparison of results (Table 1). The final cohort consisted of 118 patients with 18 men and 100 women (Figure 1).
Figure 1: Categorization of the location of parathyroid glands. A: normal superior gland in proximity of posterior surface the thyroid. B: superior gland posterior in the tracheoesophageal groove. C: superior gland fallen posteriorly and inferior in the tracheoesophageal groove. D: superior or inferior gland in mid region of posterior surface of thyroid near the junction of the recurrent laryngeal nerve and inferior thyroid artery. E: normal inferior gland in proximity of the thyroid. F: inferior gland in the thyrothymic ligament or superior thymus or in mediastinum. G: intrathyroidal gland.
| 18 Men | Median age 50 y.o | Older 86 y.o youngest 21 y.o |
| 100 Women | Median age 57 y.o | Older 73 y.o youngest 26 y.o |
| Initial MDCT diagnosis | 102 patients with | 16 patients with multi- |
| single-glandular | glandular | |
| Final surgery type | 103 patients with | 15 patients with multi- |
| single-glandular | glandular |
Table 1: Patient database.
CT imaging was performed with a 16-slice multidetector CT system (GE Lightspeed 16x) and 64-slice multidetector CT system Toshiba-Aquilion Prime). Patients were on supine position with arms parallel to their body. The scanning protocol consisted of two helical scanning: first from the mandible up to inferior limit of thyroid gland and the second scan form the mandible up to the superior border of mediastinum. The parameters for each phase for GE Lightspeed were as follows: detector configuration 16 x 1.25 mm; tube rotation time 0.6s; pitch 0.938;120 kVp; and automatic tube current modulation. For Toshiba were as follows: detector configurations 80 × 0.5mm; tube rotation time 0.5 s; pitch 0.813; 100 kVp; and automatic tube current modulation. The first scanning phase is performed without iv contrast while the second one is carried out, 40 sec after the intravenous contrast injection. For contrast enhancement was injected 100 ml iodinated contrast material (Ultravist 300, Visipaque 320 mgI/ml) at the rate of 3.5 mL/s followed by saline flush. Data were stored to PACS. Detailed study included axial plan analysis and multiplanar reconstructions (Table 2).

Table 2: Patient database parameters.
In the report was noted mono- or multi-glandular pathology defining location of pathology using referred classification system [5,15].
Preoperative approach and final surgical procedure
Historically the only potential cure for PHPT is parathyreoidectomy. The 2013 guidelines for parathyroid surgery recommend that patients with biochemically confirmed PHPT who manifest overt symptoms and signs, should undergo surgery [14].
Preoperative preparation consists of physical examination (palpation of thyroid nodulesor even parathyroid carcinoma) and biochemical confirmation of PHPT (measurements of the serum calcium, intact PTH, creatinine and 25-hydroxy-vitaminD). After decision for surgery, parathyroid localization studies allow the surgeon to attach the lesion by a focused parathyreoidectomy for mono-glandular disease orbilateral neck exploration in case of multi-glandular disease (4-gland hyperplasia ordouble adenoma). If preoperative imaging studies identify a target enlarged gland, surgeon resects it with minimal invasive parathyreoidectomy (MIP) using intraoperative PTH measurement to confirm adequate resection (biochemical cure is suggested by a drop in PTH >50% of baseline 10 to 15 minutes after target gland resection). If imaging studies are suggestive for multiglandular disease, is indicated a bilateral neck exploration. IntraoperativPTHmeasurement is useful for confirming the adequate resection by a PTH drop into 20-30 pg/ml range [14,15]. Parathyreoidectomies are routinely performed through a 2.5 cm to 3.5 cm abbreviated Kocher incision placed along existing skin creases. Surgical cure after parathyreoidectomy is defined as normoacalcemia 6 months after surgery [25].
Results
Data mining techniques were performed using WEKA 3.7.8, an open source code platform including different AI and statistical approaches [26]. In order to analyse the large amount of the available health records and extract medical knowledge information, a data mining approach is implemented. Data mining techniques were performed using the WEKA 3.7.8 that is an open software source code tool [27]. WEKA is a collection of machine learning algorithms which can either be applied for data set pre-processing, classification, regression, clustering, association rules and visualization or to develop new machine learning schemes (Figure 2).
The WEKA software uses well established mathematical algorithms with a number of them resulting decision trees for data classification [28]. Decision trees can be used either for identifying interesting information or building predictive models as in the present application. A decision tree is a classification tree which functions as a guide to make a prediction on the basis of a series of decisions based on the input data. Specifically a decision tree is a flowchart that divides up the data on each branch without losing any of the data (the number of the given total health records remains constant throughout the study) for making a series of decisions. Every time each tree is created as follows: each branch of the graphical representation displays a step where a decision must be made based on the data of an input parameter in order to proceed to the next branch of the tree. This process is repeated until a leaf provides the predicted output (the type of surgery outcome). As the final step, for each patient microscopically is expected to see a proliferation of a single cell type (chief or oxyphilic cells). Occasionally a mixture of both types of cells can be seen, raising the question of parathyroid hyperplasia. These microscopic features of parathyroid adenoma are challenges for the pathologist to judge each case of being a true adenoma or part of parathyroid hyperplasia [22-24]. The most important step in this procedure is the choice of the appropriate surgery invasion. Building a decision tree and when it has been grown up to a size, an immediate step is required to test the accuracy of the model. From the beginning, the available data were randomly divided into two subsets, a training set which was used to build the decision tree and a test set that was used to evaluate the accuracy of the model. The training set at the present work included 66 percent of the data (78 patients) whereas the remaining randomly divided data were placed in the test set (40 patients). This check is also important since machine learning algorithms present the issue of so-called over fitting that is the situation in which the induction algorithm generates a classification tree that perfectly fits the training data but is not generalizing to other instances not present. If we enter in the system new data the chosen algorithm continues to develop hypotheses reducing error while the prediction of future unknown values usually becomes worse due to increase the final test set error [29]. The available methods to avoid over fitting are the pre-pruning and the post-pruning that involves reduction size by removing branches with less power to classify the training set. Pre-pruning stops growing the tree before it perfectly classifies the training set, while post-pruning allows the expanding of the tree to perfectly classify the input set and after cutting branches. The second approach is more effective since it is not easy to precisely estimate at what size will stop evolving the decision tree. The dual goal of pruning is to reduce tree complexity and improve prediction by reduction of overfitting and removal of sections that are based on output error. To create a balance, for one tree to be as simple as possible with as few “branches” and “leaves of decision” while at the same time we will be as accurate as possible ensuring that the produced model will accurately predict future unknown set of patient data [21].
Decision trees are supervised learning algorithms. The main concept, behind decision tree learning, is: starting from the training data, we build a predictive model which is mapped to a tree structure [30]. The target is to achieve perfect classification with minimal number of decision, although not always possible due to the inconsistencies in training data (Table 3). From the table we need a decision tree which can be used to predict the type of surgery. A decision tree learning algorithm will return a prediction model (Figure 3). At the start each level splits the data according to different attributes, the non-leaf nodes are represented by attributes/parameters, and the leaf nodes represent the predicted variable or output. The algorithm for learning decision trees follows the steps:
| SEX, AGE,ADENOMA,HYPERPLASIA, TYPE, DHU, DESCRIPTION, SURGERY_TYPE |
| Woman, 63,yes,no,E2,68,medium,2 |
| Woman, 53,no,yes,E2,103,large,1 |
| Woman, 53,no,yes,F2,68,small,0 |
| Woman, 53,no,yes,E1,75,medium,0 |
| Woman, 48,yes,no,E2,110,medium,1 |
| Woman, 67,yes,no,C2,135,large,1 |
| Woman, 67,yes,no,C1,110,small,2 |
| Man, 55,yes,no,B2,175,medium,1 |
| Woman, 72,yes,no,C1,157,medium,1 |
| Woman, 59,yes,no,A1,184,medium,1 |
| Woman, 58,yes,no,C1,202,small,1 |
| Woman, 65,yes,no,B1,125,small,1 |
| Woman, 58,no,yes,A2,167,small,1 |
Table 3: Part of training data set.
Starting with the sum of training data.
Select an attribute or a value that gives “best” split create child nodes.
Recurse on each child using child data until: all examples have same class or the amount of data is too small or the tree is too large.
The main challenge while building the tree is to decide on which attribute to split the data at a certain step in order to have the “best” split (Figure 4). “Entropy” is a measure of the uncertainty contained in a piece of information and is calculated before and after each split. In the training patient dataset, must be selected the parameter that lowers the entropy:
Entropy=-pP * log2(pP) -pN * log2(pN)
pP – the proportion of positive (training) examples
pN – the proportion of negative (training) examples
For users that are not familiar with the tool in order to build the decision tree using the WEKA Explorer one can go from the “Preprocess” tab to “Open file” button and load the “database3. arrf” file. Then to the “Classify” tab, from the “Classifier” section choose “trees” > “RANDOMFOREST” and pressing Start. For the moment, the platform does not allow the visualization of the RANDOMFOREST generated trees. The J48 decision tree is the Weka implementation of the standard C4.5 algorithm which is the successor of ID3. Weka allows the generation of the visual version of the decision tree for the J48 algorithm (Figure 5). So, from the “Classifier” section select “trees” > “RANDOMTREE”. Also the “-C 0.25 -M 1” options are selected for the algorithm with:
ConfidenceFactor — The confidence factor used for pruning (smaller values incur more pruning).
Finally pressing “Start” the calculation select the result in the left pane, right-click and selecting the “Visualize tree” the final decision tree is created (Figure 6).
The random forest algorithm
The final algorithm Random Forest (RF) that has been selected here is a collection or ensemble of Classification and Regression Trees (CART) trained on datasets of the same size as training set, called bootstraps, created from a random resampling on the training patient data set itself. When the tree is constructed, a set of bootstraps, which do not include any particular record from the original dataset, is used as test set while the error rate of the resulted classification of all the test sets is the estimate of the generalization error. Breiman has proved that, for the bagged classifiers, the error is accurate as using a test set of the same size as the training set [30,31]. Consequently, using this estimate removes the need for a separate patient data test set. To classify new input data, each individual CART tree “votes” for one class of output and the “forest” predicts the class that obtains the plurality of all the “votes” [32]. RF has specific rules and is proved robust to over fitting considering more stable in the presence of outliers and in very high dimensional parameter spaces than other similar algorithms [30]. The concept of variable importance is an implicit feature selection performed by the RF, and assessed by the Gini impurity criterion index [31]. The Gini is a measure of prediction power of all variables in classification, based on the principle of impurity reduction it is non-parametric and therefore does not rely on data belonging to a particular type of distribution [33]. For a split, the Gini index of a node n is:
Gini(n)=1−Σ2j=1(pj)2
Where pj is the relative frequency of class j in the node n.
For dividing a node in the best way, the improvement in the Gini index should be maximized. In other words, a low Gini means that a specific predictor feature plays a greater role in classifying the patient data into the two classes. Thus, the Gini index can be used to rank the importance of variables for the best classification [21,33].
We also tested the dataset with alternative knowledge extraction algorithms (as J48, REPTree, Random Tree, RF, LMT) in the form of knowledge decision trees (Figure 7). The following were calculated: sensitivity (the probability that a test will indicate ‘surgery_type’ among those with the surgery), specificity (the fraction of those without disease who will have a negative test result), positive prognostic value and negative prognostic value. Finally we used the best model according to metrics as sensitivity, specificity and prognostic value [20, 21]. The best results from our experiments were succeeded with Random forest algorithm for all different patient groups of SUREGRY_TYPE are presented in the table.
According to our results we can see that the trained intelligent system based on training data of patients included in this study has high performance providing no false positive (FP or LR+) results (Figure 8). This means that for every new patient it can be proposed the proper surgery intervention very accurately with LR+=104.0 compared with 25.5 that resulted the traditional approach and perfect sensitivity.
After the final construction of the decision tree the final model was build up as a computer application with ACRES v3.0.1 platform that is an ES developing tool (Figure 9). This tool constructs ESs form data and has been developed from AI Group of Computer Engineering Department of University of Patras [23]. At the end of this procedure the user can interact with a form that asking for the input parameters of a new patient and giving as an output, using internally the ES, the possible depression type, combined with the appropriate possibility as percentage. The final tool can be easily downloaded on a mobile system for fast and on-site use by the health professional. At present is used on line from mobile phones [23]. In the future and after the collection of a new group of patient records the system can update the internal reasoning model, recalculate its’ new performance and give even more accurate results. The internal model could change both with future changes in general knowledge that will be absorbed in new established questionnaires, or in experts’ final approach according to their experience [33].
Discussion
AI has proven superiority over linear statistical models in previous reports from the medical field [25,26]. Experience from the use of A.I. such as its prognostic and diagnostic value in acute pancreatitis and pancreatic cancer showed that the management of these kinds of disorders could be greatly improved from these
Predictive systems [27,28]. To elaborate there are many medical applications of for example of Artificial Neural Networks in bibliography including cancer survival prediction, outcome prediction in patients suffering from colorectal, staging and image analysis in non-small lung cell carcinoma and breast cancer [27,28].
A.I. has been also widely used in the prediction of mortality and treatment outcomes in elderly population undergoing surgery for hip fractures and age associated neurological diseases such as Alzheimer disease and other cognitive impairments. With respect to our research, and according to our knowledge this is the first study that evaluates the prognostic value of AI techniques based on CT images for preoperative mapping and offering clinicians useful information to apply minimal invasive excision of parathyroid adenomas.
In our work we used five data mining algorithms available at the WEKA software tool. Nevertheless the results of all algorithms were satisfactory, but RandomForest algorithm yielded the best results. According to their mathematical approach it can be explained only from the type and structure of our data [20]. More patient data could result better or even different algorithm performances among data mining techniques. Finally, according to our results, we could predict the completion with sensitivity: 100.00%, specificity: 99.04%, LR+: 104.00 and no LR- with the overall accuracy was at 99.15% (Table 4).
| Input | True | True | False | False | Sensitivity | Specificit | LR - | LR + | |
|---|---|---|---|---|---|---|---|---|---|
| parameters | positive | negative | Positive | Negative | % | y % | Accuracy | ||
| Computer | |||||||||
| System | 14 | 1 | 0 | 103 | 100.00 | 99.04 | 0.00 | 104.00 | 99.15 |
| Traditional | |||||||||
| Approach | 12 | 3 | 4 | 99 | 75.00 | 97.06 | 0.26 | 25.50 | 94.07 |
Table 4: Classification results for both predictions.
Despite the effectiveness of the above models, there are some limitations that need to be improved in order to be more accurate as it seems that sometimes the model incorrectly classifies some of the data. This may be attributed to the fact that the choice of an acceptable percentage of errors as the choice between false positive or false negative option depends on the model creator that sometimes cannot distinguish them.
This study reveals that the most important application of AI is in extremely complex medical situations where the prognostic factors and their relationships, which might influence the treatment decision, are not detectable in most common statistic algorithms [23,28]. Software tools as WEKA usually include A.I. as well as statistical approaches that the user could compare in order to have the best output [27,33]. According to our study the surgeon can predict the number of pathologic adenomas using a simple and fast AI system stored in a mobile platform as an IPhone with very good results even if is controversial to radiologist’s results.
Conclusion
Decision of minimal invasive parathyreoidectomy or extensive bilateral neck exploration depends on preoperative imaging studies. Adjusting αν application of A.I. in clinical practice can be demonstrated beneficial as it could facilitate health professionals in taking critical and evidence based medical decisions provided through fast and simply used as mobile applications. At present the prototype system is used on-line from mobile phones. In the future and after the collection of a new group of patient records the system can update the internal reasoning model, recalculate its’ new performance and give even more accurate results.
References
- Douglas PC, Deborah RS (2012) Imaging of the Parathyroid Glands. Semin Ultrasound CT MRI 33: 123-129.
- Geneva JR, Philip BZ, James IC, Bronwyn EH (2009) Contrast-enhanced MDCT characteristics of parathyroid adenomas. AJR 193.
- Chazen JL, Gupta A, Dunning A, Phillips CD (2012) Diagnostic accuracy of 4D-CT for parathyroid adenomas and hyperplasia. AJNR Am J Neuroradiol 33: 429 –433.
- Jenny KH, Won-kyung S, Manisha B, Douglas PC (2014) How to perform parathyroid. 4D CT: tips and traps for technique and interpretation. Radiology 270: 1.
- Steven ER, George JH, Leena MH, Dawid S, David BD, et al. (2006) Improved preoperative planning for directed parathyroidectomy with4-dimensional computed tomography. Surgery 140: 932-941.
- Kelly HR, Hamberg LM, Hunter GJ (2014) 4D-CT for preoperative localization of abnormal parathyroid glands in patients with hyperparathyroidism: accuracy and ability to stratify patients by unilateral versus bilateral disease in surgery-naive and re-exploration patients. AJNR Am J Neuroradiol 35: 176–181.
- Timothy AP, Moshim K, Rania E, William C, Ahmed A (2014) Low dose four-dimensional computerized tomography with volume rendering reconstruction for primary hyperparathyroidism: How I do it? World J Radiol 6: 726-729.
- David F, Jose VT, Beatriz D, Oriol S, Gloria M, et al. (2009) Dual-phase 99 mTc-MIBI scintigraphy to assess calcimimetic effect in patients on haemodialysis with secondary hyperparathyroidism . Nucl Med Commun 30: 890-894.
- Nathan AJ, Mitchell ET, Jennifer BO (2007) Parathyroid Imaging: technique and role in the preoperative evaluation of primary hyperparathyroidism. AJR 88: 1706– 1715.
- Michael D, Beland WW, Mayo-Smith DJ, Grand JT, Machan JM, et al. (2011) Dynamic MDCT for localization of occult parathyroid adenomas in 26 patients with primary hyperparathyroidism. AJR 196: 61–65.
- Nancy D, Perrier Ζ, Beth EΖ, Rodolfo NΖ, Isis GΖ et al. (2009) A novel nomenclature to classify parathyroid adenomas. World J Surg 33: 412–416.
- George JH, Daniel TG, Hillary RK, Elkan FH, Leena MH (2014) Discriminating parathyroid adenoma from local mimics by using inherent tissue attenuation and vascular information obtained with four-dimensional CT: Formulation of a multinomial logistic regression model. Radiology 270: 1.
- Jacqueline A, Wieneke Ζ, Alice S (2008) Parathyroid Adenoma .Head Neck Pathol 2: 305–308.
- Glenda GC, Robert U (2014) Surgery for Primary Hyperparathyroidism Cancer December.
- Elizabeth GG, Beth SE, Maria KG, Brett JM, Edmund K, et al. (2009) Chapter 2 Preoperative Parathyroid Imaging for the Endocrine Surgeon. Handbook of Parathyroid Diseases: 19 A Case-Based Practical Guide.
- Manisha B, Sepahdari AR, Julie AS, Jenny KH (2015) Parathyroid adenomas and hyperplasia on four-dimensional CT scans: three patterns of enhancement relative to the thyroid gland justify a three-phase protocol. Radiology 000: 1–9.
- Michael JC, Paul S, Adnan A, Blackmore CC, John AR (2015) Two-phase (low-dose) computed tomography is as effective as 4D-CT for identifying enlarged parathyroid glands. Int J Surg 14: 80-84.
- Ayman A, Matthias H, Christian S, Hans JS , Ernst MJ (2013) Highly efficient localization of pathological glands in primary hyperparathyroidism using contrast-enhanced ultrasonography (CEUS) in comparison with conventional ultrasonography. J Clin Endocrinol Metab 98: 2019–2025.
- Manjunath G, Anurag RL, Swati SJ, Sushil S, Priya H (2017) Percentage arterial enhancement: An objective index for accurate identification of parathyroid adenoma/hyperplasiain primary hyperparathyroidism. Clin Endocrinol 87: 791–798.
- Baxt WG (1995) Application of artificial neural networks to clinical medicine. Lancet 346: 1135-1138.
- Eibe F (2009) Machine Learning Group at the University of Waikato. WEKA.
- Elias K, Susanne K, Helmut H, Detlef KB, Ilhan C (2012) Does contrast-enhanced cervical ultrasonography improve preoperative localization results in patients with sporadic primary hyperparathyroidism? J Clin Imag Sci 2: 4.
- Christina L, Peter G, Christian W, Norbert S (2015) MarioColombo-Benkmann Preoperative 11C-Methionine PET/CT Enables Focused Parathyroidectomy in MIBI-SPECT Negative Parathyroid Adenoma. World J Surg 39: 1750–1757.
- Nael K, Hur J, Bauer A, Khan R, Sepahdari A (2015) Guerrero Dynamic 4D MRI for Characterization of Parathyroid Adenomas: Multiparametric Analysis
- Marchevsky AM, Patel S, Wiley KJ (1998) Artificial neural networks and logistic regression as tools for prediction of survival in patients with stages I and II non-small cell lung cancer. Mod Pathol 11: 618-625.
- Koutsojannis C, Lithari C, Hatzilygeroudis I (2010) Managing urinary incontinence through hand-held real-time decision support aid. MEDICON 2010, IFMBE Proceedings 29: 913–919.
- Burke HB, Goodman PH, Rosen DB, Henson DE, Weinstein JN (1997) Artificial neural networks improve the accuracy of cancer survival prediction. Cancer 79: 857-862.
- Baxt WG (1995) Application of artificial neural networks to clinical medicine. Lancet 346: 1135-1138.
- Breiman L, Friedman J, Stone CJ, Olshen RA (1984) Classification and Regression Trees. Boca Raton FL: CRC press.
- Breiman L (1996) Bagging predictors. Mach Learn 24: 123–140.
- Ceriani L, Verme P (2012) The origins of the gini index: extracts from variabilità e mutabilità (1912) by corrado gini. J Econ Inequal 10: 421–443.
- Strobl C, Boulesteix AL, Augustin T (2007) Unbiased split selection for classification trees based on the gini index. Comput Stat Data Anal 52: 483–501.
- Sarica A, Cerasa A, Quattrone A (2017) Random forest algorithm for theclassification of neuroimaging data in Alzheimer’s Disease: A systematic review. Frontiers in Aging Neuroscience 9: 329.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi