Case Report, J Clin Image Case Rep Vol: 7 Issue: 3
Highly Numerous Post-Traumatic Splenic Pseudoaneurysms
Andrew Samoyedny*
Department of Pediatric Radiology, Hospital of the University of Pennsylvania, Philadelphia, United States
*Corresponding Author:
Andrew Samoyedny
Department of Pediatric Radiology,
Hospital of the University of Pennsylvania,
Philadelphia,
United States,
Tel: 5709569342;
E-mail: as4336@drexel.edu
Received date: 17 January, 2020, Manuscript No. CICR-23-6445;
Editor assigned date: 21 January, 2020, PreQC No. CICR-23-6445 (PQ);
Reviewed date: 04 February, 2020, QC No. CICR-23-6445;
Revised date: 14 June, 2023, Manuscript No. CICR-23-6445 (R);
Published date: 12 July, 2023, DOI: 10.4172/CICR.1000248
Citation:Samoyedny A (2023) Highly Numerous Post-Traumatic Splenic Pseudoaneurysms. J Clin Image Case Rep 7:3.
Abstract
Splenic Pseudoaneurysms (SPA) are a dangerous complication of splenic trauma. Pancreatitis, peptic ulcer disease and iatrogenic reasons are additional possible causes of SPA. They are extremely rare, with only about 200 cases published in the English literature in 2006, and their prevalence is essentially unknown. SPA have a significant risk of rupture and have been documented to be deadly in adulthood if left untreated. SPA can form 1 to 8 days following a traumatic splenic lesion in the setting of trauma and may be undetected on initial imaging.
Keywords: Splenic pseudoaneurysm, Ulcer disease, Pancreatitis
Introduction
The treatment of adult blunt splenic trauma is thoroughly researched. However, management in paediatric patients is ambiguous. In terms of SPA, only eleven paediatric case studies are available in English [1]. Although uncommon, traumatic Splenic Artery Pseudoaneurysm (SAP) can be fatal. The diagnostic approaches and therapy methods for SAP have yet to be determined. A 10-year-old child was treated conservatively for a grade III Blunt Splenic Injury (BSI). After a 5-day uneventful hospitalisation, the child was returned home, but a routine follow-up CT scan revealed a big SAP. The pseudoaneurysm was successfully angiographically embolised and a later abdominal CT revealed that the pseudoaneurysm had been successfully resolved, with just a minor remnant splenic cyst [2].
Management of adult blunt splenic trauma is well-studied. However, the management in pediatric patients is poorly defined. With regards to SPA, only eleven pediatric case reports are found in the English literature. Although the American pediatric surgical association does not recommend routine follow-up imaging in pediatric trauma patients regardless of grade of injury, several reviews have described the potential benefits of follow-up CT imaging for detection of pseudoaneurysm [3].
Pseudoaneurysm (PA) formation after blunt and penetrating abdominal trauma is a well-known consequence of solid organ injury that is usually detected via Contrast-Enhanced CT (CECT) imaging. Delayed rupture is a potentially fatal event in paediatric trauma, but its prevalence is unknown. Contrast Enhanced Ultrasound (CEUS) is a unique radiation-free alternative to CECT that may be used to detect PA.
Treatment
Pseudoaneurysms can be treated with embolization using liquid embolic agents to thrombose the inflow and outflow arteries or filling the sac itself. Distal splenic embolization should be avoided.
Case Presentation
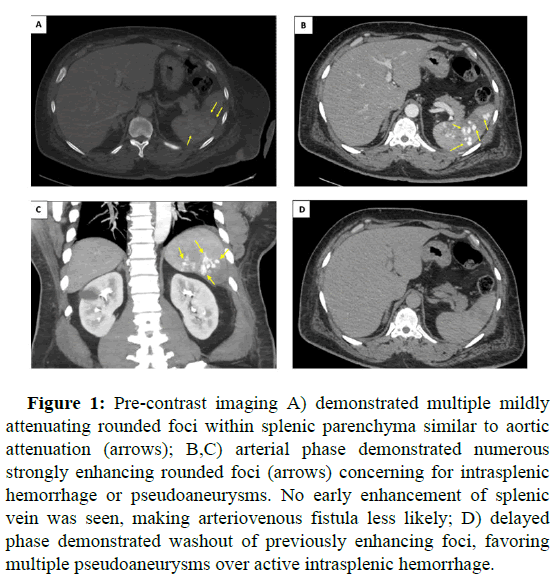
A 55-year-old male presented to the emergency department with worsening left abdominal pain one week after an assault with a wooden board to the left abdomen. Contrast-enhanced CT was obtained with pre-contrast, arterial, venous, and delayed phases [4]. Pre-contrast imaging (A) demonstrated multiple mildly attenuating rounded foci within splenic parenchyma similar to aortic attenuation (arrows). Arterial phase (B, C) demonstrated numerous strongly enhancing rounded foci (arrows) concerning for intrasplenic hemorrhage or pseudoaneurysms [5]. No early enhancement of splenic vein was seen, making arteriovenous fistula less likely. Delayed phase (D) demonstrated washout of previously enhancing foci, favoring multiple pseudoaneurysms over active intrasplenic hemorrhage. The patient recovered with supportive care only; pseudoaneurysms later resolved on follow-up imaging (Figure 1).
Figure 1: Pre-contrast imaging A) demonstrated multiple mildly attenuating rounded foci within splenic parenchyma similar to aortic attenuation (arrows); B,C) arterial phase demonstrated numerous strongly enhancing rounded foci (arrows) concerning for intrasplenic hemorrhage or pseudoaneurysms. No early enhancement of splenic vein was seen, making arteriovenous fistula less likely; D) delayed phase demonstrated washout of previously enhancing foci, favoring multiple pseudoaneurysms over active intrasplenic hemorrhage.
Splenic pseudoaneurysms are rare post-traumatic sequelae with a high risk of rupture and mortality. Their perceived rarity may be due to poor documentation of cases in the English medical literature, as only 200 cases had been reported as of 2007. They are far less common than their nontraumatic cousin, splenic aneurysm [6]. As a posttraumatic sequela as in the presented case, splenic pseudoaneurysm is typically a delayed phenomenon occurring within 1 to 3 weeks posttrauma. The primary symptom is acute-onset severe left upper quadrant abdominal pain. Due to the rarity of splenic pseudoaneurysm, data on outcomes is sparse. Rupture may occur in up to 37% of cases, and data suggest a mortality rate of 90% for untreated rupture. Given the high risk of rupture and the corresponding high risk of mortality, the consensus in the literature is urgent management either through splenectomy or endovascular embolization [7,8].
This case is notable for the exceptional number of pseudoaneurysms present as well as their spontaneous resolution in the absence of intervention.
Results and Discussion
Splenic Artery Pseudoaneurysms (SPA) remain a rare but potentially fatal pathology following blunt trauma which is managed non-operatively. Delayed splenic rupture is observed in approximately 6% of cases of adult splenic trauma. Most of these cases are caused by traumatic SPA. Studies have demonstrated the benefits of repeated follow-up imaging and early intervention upon diagnosis of SPA. Management of SPA can be operative entailing splenectomy with or without pancreatectomy or non-operative, using endovascular techniques. In recent studies, utilization of angioembolization has been demonstrated to decrease non-operative management failure rate in adults with blunt splenic injuries. However in children, there are no strong evidence-based guidelines that exist to help guide management of SPA.
Studies have revealed that radiation from a single CT scan increases the risk of cancer. The amount of the risk, however, remains unknown. According to Brenner et al. of Columbia university, the lifetime risk of deadly malignancy from both abdomen and head CT examination is approximately 500 out of 600,000. Although the danger exists, the benefits of a CT scan may outweigh the little increase in cancer risk in emergency scenarios. Given that several of the above-mentioned sample populations had CT scans more than a decade ago, advances in CT technology may have greatly reduced the radiation burden on children.
Our proposed protocol is based on more conservative approach than Mayglothling et al. (Figure 1). Even though there may be an association between incidence of SPA and high grade splenic lacerations (i.e., grade III and IV splenic laceration), there is no strong clinical evidence to show benefits of aggressive angiography of these patients. We concur with Safavi et al. in the necessity of follow-up imaging before planned discharge because there is a potential risk of delayed splenic rupture in this population. The natural course of SPA in children needs to be further studied and defined.
Conclusion
Splenic artery pseudoaneurysm is an uncommon vascular lesion. Most are caused by pancreatic disease; however, trauma is also a common cause. Endovascular therapy of PAs in trauma patients can be efficiently integrated into the trauma process. Endovascular therapy of traumatic visceral and extremities PAs is effective, with low complication rates and no need for reintervention.
References
- Agrawal GA, Johnson PT, Fishman EK (2007) Splenic artery aneurysms and pseudoaneurysms: Clinical distinctions and CT appearances. Am J Roentgenol 188: 992-999.
[Crossref] [Google Scholar] [PubMed]
- Jesinger RA, Thoreson AA, Lamba R (2013) Abdominal and pelvic aneurysms and pseudoaneurysms: Imaging review with clinical, radiologic, and treatment correlation. Radiographics 33: E71-E96.
[Crossref] [Google Scholar] [PubMed]
- Lopez-Tomassetti Fernandez E, Delgado-Plasencia L, Arteaga-Gonzalez I, Carrillo-Pallares A, Diaz-Romero F (2008) Posttraumatic intrasplenic pseudoaneurysm with high-flow arteriovenous fistula: New lessons to learn. Eur J Trauma Emerg Surg 34: 305-308.
[Crossref] [Google Scholar] [PubMed]
- Fitoz S, Atasoy C, Dusunceli E, Yagmurlu A, Erden A, et al. (2001) Post‐traumatic intrasplenic pseudoaneurysms with delayed rupture: Color Doppler sonographic and CT findings. J Clin Ultrasound 29: 102-104.
[Crossref] [Google Scholar] [PubMed]
- Yardeni D, Polley Jr TZ, Coran AG (2004) Splenic artery embolization for post-traumatic splenic artery pseudoaneurysm in children. J Trauma 57: 404-407.
[Crossref] [Google Scholar] [PubMed]
- Foo ET, Kumar V, Nanavati SM, Huo E, Wilson MW, et al. (2018) Percutaneous embolization of post traumatic splenic pseudoaneurysm. Emerg Radiol 25: 719-722.
[Crossref] [Google Scholar] [PubMed]
- Raghavan A, Wong CKF, Lam A, Stockton V (2004) Spontaneous occlusion of post-traumatic splenic pseudoaneurysm: Report of two cases in children. Pediatr Radiol 34: 355-357.
[Crossref] [Google Scholar] [PubMed]
- Yamanaka Y, Ishida H, Naganuma H, Komatsuda T, Miyazawa H, et al. (2018) Superb Microvascular Imaging (SMI) findings of splenic artery pseudoaneurysm: A report of two cases. J Med Ultrason 45: 515-523.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi