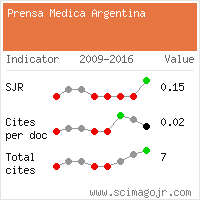
Short Communication, La Prensa Medica Vol: 107 Issue: 7
CHONDROBLASTOMA MIMICKING INFECTIVE ARTHRITIS: A DIAGNOSTIC DILEMMA
Saba Feraz
Department of Radiology, Discovery Diagnostics, Jamshedpur, Jharkhand, India.
*Corresponding author:
Saba Feraz , Department of Radiology, Discovery
Diagnostics, Jamshedpur, Jharkhand, India
E-mail: drsabaferaz@gmail.com
Abstract
Chondroblastoma is a rare chondroid tumor, accounting for 1-2% of all primary bone tumors(1,2). It primarily affects adolescents and the young population, between 10-25 years of age with the male-to-female predominance of 2:1(2,5,7). It involves the epiphysis or epiphysis equivalent (apophysis) of bones, most commonly femur, tibia, and humerus (1,3). Other rare sites of occurrence are ilium, acetabulum, patella, small bones of hand and foot, most commonly talus and calcaneum, and temporal bone(1). Rarely, it has been reported in metaphysis and diaphysis of long bones (1,3). It is associated with marked inflammatory reaction in the form of thick periosteal reaction, marrow edema, erosion of cartilage, and joint effusion which are better seen on MR imaging, mimicking the imaging findings of other benign bony entities like osteoid osteoma and eosinophilic granuloma in children and stress fracture in adults and infection in both(3,4,6,9,14). We hereby present a case of chondroblastoma of the distal femur presenting with synovitis of the knee joint.
Keywords: Chondroblastoma, DIAGNOSTIC DILEMMA
Introduction
Chondroblastoma is a rare chondroid tumor, accounting for 1-2% of all primary bone tumors(1,2). It primarily affects adolescents and the young population, between 10-25 years of age with the male-to-female predominance of 2:1(2,5,7). It involves the epiphysis or epiphysis equivalent (apophysis) of bones, most commonly femur, tibia, and humerus (1,3). Other rare sites of occurrence are ilium, acetabulum, patella, small bones of hand and foot, most commonly talus and calcaneum, and temporal bone(1). Rarely, it has been reported in metaphysis and diaphysis of long bones (1,3). It is associated with marked inflammatory reaction in the form of thick periosteal reaction, marrow edema, erosion of cartilage, and joint effusion which are better seen on MR imaging, mimicking the imaging findings of other benign bony entities like osteoid osteoma and eosinophilic granuloma in children and stress fracture in adults and infection in both(3,4,6,9,14). We hereby present a case of chondroblastoma of the distal femur presenting with synovitis of the knee joint.
Case report
A 10year-old male child presented to our hospital with complaints of pain, swelling, and restriction of left knee movements for 3 months. There was no history of trauma and fever and past medical history was also insignificant. The Vitals of the patient was within normal limits. Physical examination revealed swelling over the left knee joint and painful terminal restriction of knee movements. There were no local signs of inflammation. Laboratory investigations were all within normal limits.
AP(Fig.1) & lateral(Fig.2) radiographs of the left knee showed an expansile geographic lytic lesion involving the medial distal epiphyseal-metaphysis of the left femur with extension across the growth plate and a focal cortical breach was noted in the proximal part. The lesion showed internal matrix calcification with sclerotic margins. No adjoining or distant periosteal reaction was present. Soft tissue around the knee joint appeared prominent with fullness in the popliteal fossa and suprapatellar pouch. The age of the patient and a well-defined lytic lesion involving the distal epiphyseal-metaphyseal region of the femur with a narrow zone of transition suggested the diagnosis of benign bone tumor most likely chondroblastoma.
Magnetic resonance (MR) images showed a well defined altered signal intensity lesion of size~ 2.2 x 1.5 x 2.7 cm (APxTRxCC) in medial distal epiphysis and metaphyses of the left femur with thin peripheral hypointense rim and cortical breach at proximal aspect. The lesion was hypointense on T1W sequence and heterogeneously hyperintense on T2W and short-tau inversion recovery (STIR) sequences. There is evidence of marked edema in the rest of the distal femoral epiphysis and metaphysis. The lesion showed inhomogeneous internal enhancement with areas of peripheral enhancement within the lesion. Enhancement was also noted in the rest of the epiphysis and metaphysis. There are thickening and enhancement of synovium of the knee joint with evidence of moderate joint effusion. No extension of the bony lesion into adjoining soft tissue or knee joint was seen. No skip lesion was seen.
Knee joint aspiration cytology showed inflammatory cells and no neoplastic cells were found. Fine Needle Aspiration Cytology from the lytic lesion showed neoplastic chondroblasts and multinucleated osteoclast-like giant cells and tumor cells surrounded by dark blue “chicken wire” calcifications. After clinico-radio-pathological correlation, the diagnosis of chondroblastoma with reactive knee joint effusion was made. The patient was treated with extended curettage and bone grafting. Tissue was sent for histopathology which confirmed the diagnosis of chondroblastoma. The post-operative period was uneventful and the patient was discharged on the 7th day. The patient was followed for 1 year which did not any evidence of recurrence of the tumor.
Discussion
Distal femur is a common site of occurrence of chondroblastoma. It commonly presents with localized pain and swelling, limitation of movements, and muscle atrophy(7). It presents as a well-defined lytic epiphyseal lesion with sclerotic margins and a narrow zone of transition(1,10). Chondroid matrix calcification and extension into metaphysis are commonly seen.
Marked local inflammatory reaction in the form of soft tissue and bone marrow edema, periosteal reaction, synovial thickening, and enhancement with joint effusion is seen in association(2,6,7,8). The presence of solid or layered periosteal reaction distant to the lesion (involving the meta-diaphysis) is characteristic of chondroblastoma(11). Joint involvement can be due to direct extension of tumor or as reactive synovitis(3,6). The two can be differentiated by the presence of neoplastic cells in the joint aspirate. Marrow edema and reactive synovitis completely regresses post-treatment and thus is an important sign of eradication or recurrence of the tumor(3,7). The inflammatory reaction in chondroblastoma is due to the secretion of prostaglandin (PGE2) and cytokines like interleukin 1β, 5,6, and 8 and TNF-α by the neoplastic cells(8). Other benign bone tumors associated with inflammatory response include osteoid osteoma, eosinophilic granuloma, and osteoblastoma(2,6).
Plain radiography is the first investigation of choice for any bony complaints and clinical history and radiographic appearance help in reaching a probable diagnosis in the majority of the cases(9). MR imaging is performed to assess the extent of soft tissue and marrow involvement and presence of any skip lesions(5,9) MRI properly depicts the extent of bone marrow edema, overlying periosteal reaction, and soft-tissue extension of tumor. Benign bony entities like chondroblastoma, osteoid osteoma, eosinophilic granuloma, or stress fracture mimic the appearance of extensive infection or an aggressive bony tumor on MRI(9).
In our case the plain radiography classically suggested a benign epiphyseal tumor, however, MRI findings of synovial thickening, enhancement, and knee joint effusion, greatly confounded the diagnosis and presented an infective picture.
Chondroblastoma should be treated surgically as it can show locally aggressive behavior (2,12). It has a high recurrence rate ranging between 8-38% with most of the cases of recurrence associated with non-aggressive surgical curettage due to concern of damage to the growth plate or difficult accessibility of lesion like in femoral neck(12,13). Secondary aneurysmal bone cyst formation is noted in around 10-15% of cases(5,12). It mainly presents as a benign tumor, however, primary malignant and metastatic forms and malignant degeneration into chondrosarcoma have also been reported(1,15).
Conclusion
Clinicians and radiologists should keep in mind that chondroblastoma sometimes is associated with an intense inflammatory reaction which could lead to an erroneous diagnosis of a benign condition to a malignant one or overestimation of the aggressiveness of the lesion. Many times, because of the presence of findings of synovitis and joint effusion, the condition could also be labelled as infective.
References
- Jilong Yang, Wei Tian, Xiongzeng Zhu, Jian Wang Chondroblastoma in the long bone diaphysis: a report of two cases with literature review. Chin J Cancer. 2012, 31(5): 257â??264. doi: 10.5732/cjc.011.10402
- Y Karkhur, A Tiwari, T Verma, and L Maini. Unusual presentation of chondroblastoma mimicking Trevor's disease J Postgrad Med. 2017 Jul-Sep; 63(3): 197â??199. doi:4103/0022-3859. 201414
- Wang F, Li J, Yu D, Wang Q. Chondroblastoma of the distal femoral metaphysis: A case report with emphasis on imaging findings and differential diagnosis. Medicine (Baltimore). 2018;97(17):e0336. doi:10.1097/MD.0000000000010336
- Kaneko H, Kitoh H, Wasa J, Nishida Y, Ishiguro N. Chondroblastoma of the femoral neck as a cause of hip synovitis. J Pediatr Orthop.B 2012 Mar;21(2):17982. doi:10.1097/BPB.0b013e3283484c31. PMID:21685802
- Justin Q. Ly, Lorine M. LaGatta, and Douglas P. Beall. Calcaneal Chondroblastoma with Secondary Aneurysmal Bone Cyst.AJR. 2004;182: 130-130. 10.2214/ajr.182.1.1820130.
- Yamamoto T, Hashimoto J, Mizuno K. Hip Synovitis Associated with Chondroblastoma; Japanese Journal of Rheumatism and Joint Surgery. 1993 :12, 404-408; doi:10.11551/jsjd1982.12.403.
- Yamamura S, Sato K, Sugiura H. et al. Inflammatory reaction in chondroblastoma. Skeletal Radiol. May 1996:25, 371-376 (1996). Doi:10.1007/s002560050097
- Uchikawa C, Shinozaki T, Nakajima T, Takagishi K. Cytokine synthesis by Chondroblastoma: Relation to local inflammation. Journal of Orthopaedic Surgery. April 2009:56-61. Doi:10. 1177/230949900901700113
- Hayes CW, Conway WF, Sundaram M. Misleading Aggressive MR imaging Appearance of Some Benign Musculoskeletal Lesions. Radiographics Nov 1992; 12:1119-1134; org/10.1148/radiographics.12.6.14390151992.
- Li X, Peng Z, Zhao J, Zhang Z. Chondroblastoma of the Navicular Bone, Iran J Radiol. 2014; 11(4):e10848.doi: 10.5812/iranjradiol.10848.
- Brower AC, Moser RP, Kransdorf MJ. The frequency and diagnostic significance of periostitis in chondroblastoma. AJR Am J Roentgenol. 1990;154 (2): 309-14.AJR
- Suneja R, Grimer RJ, Belthur M, Jeys L, Carter SR, Tillman RM, Davies AM. Chondroblastoma of bone: long-term results and functional outcome after intralesional curettage. J Bone Joint Surg Br. 2005 Jul;87(7):974-8. Doi: 10.1302/0301-620X.87B7.16009.PMID:15972914.
- Sailhan F, Chotel F, Parot R; SOFOP. Chondroblastoma of bone in a pediatric population. J Bone Joint Surg Am. 2009 Sep;91(9):2159-68. Doi: 10.2106/JBJS.H.00657. PMID: 19723993.
- Ishida T, Goto T, Motoi N, Mukai K. Intracortical chondroblastoma mimicking intra-articular osteoid osteoma. Skeletal Radiol.2002 Oct;31(10):603-7.doi: 10.1007/s00256-002-0565-1.
- VukasinoviÄ? Z, Spasovski D, SlavkoviÄ? N, SlavkoviÄ? S, ZivkoviÄ? Z. [Chondroblastoma--current opinion]. Srp Arh Celok Lek. 2006 Nov-Dec;134(11-12):567-70. Serbian. PMID: 17304775.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi