Research Article, J Clin Exp Radiol Vol: 6 Issue: 4
Added Value of Low-Dose CT by using SPECT V/Q Scan in the Diagnosis of Pulmonary Embolism
Tawakol A1, Yahya Ali Mohamed1*, Yasser Mohamed Ahmed El- Sayed1, Takeya Ahmed Taymour2 and Ahmed Badawy1
1Department of Oncology and Nuclear Medicine, Cairo University, Cario, Egypt
2Department of Radiodiagnosis, Cairo University, Cario, Egypt
- *Corresponding Author:
- Yahya Mohamed
Department of Oncology and Nuclear Medicine,
Cairo University,
Cario,
Egypt;
E-mail: mostafabakry9090@gmail.com
Received date: 05 December, 2023, Manuscript No. JCER-23-123535;
Editor assigned date: 08 December, 2020, PreQC No. JCER-23-123535 (PQ);
Reviewed date: 22 December, 2020, QC No. JCER-23-123535;
Revised date: 26 December, 2023, Manuscript No. JCER-23-123535 (R);
Published date: 02 January, 2023, DOI: 07.4172/jcer.1000149
Citation: Tawakol A, Mohamed YA, El-Sayed YAM, Taymour TA, Badawy A (2023) Added Value of Low-Dose CT by using SPECT V/Q Scan in the Diagnosis . of Pulmonary Embolism. J Clin Exp Radiol 6:4.
Abstract
Untreated Pulmonary Embolism (PE) can be lethal, with fatality rates ranging from 10% to 30%. Although a variety of symptoms, signs, laboratory tests and/or predisposing patient characteristics can be utilized to develop a clinical probability of PE, these criteria are frequently vague making PE diagnosis difficult even in a strongly suspected case. PE is diagnosed based on clinical symptoms, D-dimer test findings and imaging investigations such as Multi Detector CT (MDCT) and Ventilation/perfusion (V/Q) scintigraphy. So far, radionuclide imaging has only used planar and Single Photon Emission CT (SPECT) methods. Although both methods provide information on radioisotope distribution, neither provides anatomical detail. Furthermore, perfusion and breathing investigations are necessary to confirm or rule out the diagnosis of PE.
Keywords: Nuclear medicine, Emphysema, Malignancy, Pulmonary embolism
Introduction
In daily practice, Pulmonary Embolism (PE) remains a diagnostic difficulty. In those who have PE suspicion, V/Q Single Photon Emission Computed Tomography (SPECT) has emerged as an alternative to CTPA. For more than 20 years, the V/Q scan was the gold standard, but CTPA is now the first-line imaging modality in most institutions for PE diagnosis, especially because CTPA allows for alternate diagnoses [1-5].
In clinical nuclear medicine, hybrid imaging employing SPECT/CT methods is becoming more common, with many institutions now outfitted with SPECT/CT cameras. These systems can do SPECT and CT scans in the same session. The combination of functional data from SPECT capture with anatomic characterization on CT images has been found to increase scintigraphic sensitivity and specificity.
Moreover, not all cases with PE exhibit the characteristic V/Q mismatch pattern since some suffer from pulmonary infarction, leading to matched deficits. For these reasons, many regard chest radiograph appearances to be critical in assisting in the interpretation of the V/Q scan and the results are frequently employed to enhance the accuracy and specificity of V/Q reporting.
The advantages of each modality can be gained by combining a V/Q SPECT examination with a CT study, even one employing "lowdose" settings to limit patient radiation dosage. SPECT/CT imaging can identify V/Q mismatch owing to disorders other than PE (such as radiation therapy-induced alterations, emphysema and extrinsic vascular compression from conditions such as malignancy or mediastinal adenopathy) [6-10].
Materials and Methods
Study population
The study included 81 individuals with probable PE (18 males and 63 women, with a mean age of 43.36 14.32 years). Since October 2019, V/Q SPECT/CT has been used as a standard diagnostic technique in our department for PE suspicion. From December 2019 to September 2021, patients aged 18 and up were sent to the nuclear medicine department at Cairo university hospital (NEMROCK) with symptoms indicative of acute PE. The clinical likelihood of PE was classified as low, middle or high by the physicians in charge using the modified wells criteria. All patients were considered for inclusion if they had either a high clinical probability of PE or a low clinical probability but had symptoms suggestive of PE, such as SOB (63 patients), chest pain (22 patients), cough (24 patients), hemoptysis (2 patients) and (59 patients) with abnormal enzyme linked immunosorbent assay D-dimer concentration (>500 g/ml). Patients under the age of 18 or pregnant women were excluded from the study.
The most important risk factor for suspected pulmonary embolism is DVT which was reported in (10 patients). Risk factors for formation of venous thromboembolic as immobility for more than 7 days, major surgery were also reported in (6 patients). (62 patients) had pulmonary hypertension by echocardiography and (18 patients) gave history of pulmonary embolism or DVT treated medically with good clinical outcome [11,12].
Imaging protocols
Q acquisition technique: 5 mCi of 99m Tc MAA (about 450-500 thousand of particles in normal adult patients) always injected slowly (over 15 seconds) during 3-5 respiratory cycles. SPECT cameras (Symbia T2 system; siemens or discovery 630 system; GE), collimators: LEHR, energy windows: 140 KeV, 20% for GE and 15% Siemens, energy correction: Tc99m (Tc_INTR), patient position: Supine. Area of interest (i.e., lung fields) in FOV, matrix: 256 × 256 × 16, zoom: 1.46 × 40.9 cm, total counts: 500-800-kC/view/head, correct orientation is default (180 degrees) and view sequence detector1-detector2: Anterior-posterior, LAO-RPO, LL-RL, LPORAO.
V acquisition technique: Because it is more challenging to provide a bigger dosage of 99m Tc DTPA than it is to administer a larger dose of 99m Tc MAA, aerosol imaging is often done before perfusion imaging. It is crucial that the count rate of the second trial be at least four times that of the first study because both agents were labeled with 99m Tc. The nebulizer was loaded with the required dose of 99m Tc DTPA (20 mCi in 1.5 ml), until sufficient radiotracer delivered to the lung and the count rate in the posterior view was 1,000 counts/s. Image acquisition parameters: Similar to perfusion parameters.
SPECT/CT acquisition technique
SPECT acquisition: The same cameras (Siemens' Symbia T2 System) were used to record the SPECT imaging data. The chest's SPECT images were acquired for 20 s/step with 3° increments in a 128 × 128 matrix after the perfusion planner projections. Iterative ordered subset expectation maximization was used to recreate SPECT imaging data. Trans axial, coronal and sagittal planes of the resultant pictures were shown and they were combined with the appropriate CT image slices.
Low-dose CT acquisition: On a hybrid SPECT/CT system (Symbia T2 System; Siemens), low dose-CT was done concurrently with Q SPECT on all patients. Following the Q SPECT, the patient underwent a Low Dose CT scan (130 kV, 60 mAs, pitch: 0.85), without contrast enhancement, while holding their breath or inhaling shallowly, depending on the severity of their dyspnea. The cephalocaudal direction and 512 × 512 matrix were used to acquire the pictures. Sections that were 5 mm thick were used to recreate axial, coronal and sagittal slices.
Image interpretation
On the Intellispace portal system (Philips), images were interpreted two nuclear medicine doctors with expertise in reading V/Q scans. To prevent recollection bias, the planar and SPECT/CT scan datasets were read separately. The ultimate arbitrator of the imaging investigations was a third reader with additional knowledge.
Planscans were examined using modified PIOPED II standards. PE present (high-probability V/Q scan), PE absent (normal or lowprobability V/Q scans) and nondiagnostic (all other results) were the PIOPED II classifications [13-15].
The planar images were not used in the binary interpretation of the Q-SPECT/CT scans. PE was evident, indicating at least one wedgeshaped peripheral defect that was clearly visible in all three orthogonal planes and was assessed to be less than 50% of a lung segment. In addition, we needed the absorption of macro aggregated albumin to be visibly decreased by 70% relative to regularly perfused lung in order to account for often seen in homogeneities dis intensity. Any perfusion defect that had a matching abnormality on the CT scan (such as a mass, consolidation, effusion, emphysema or fibrosis) or any perfusion defect that involved less than 50% of a segment without an associated abnormality. On Q-SPECT images, the outer lung contours typically exhibit slight abnormalities that may be related to breathing during image capture. The low-dose CT images were separately evaluated by a chest radiologist, who noted all pulmonary and pleural abnormalities.
Unfortunately, since beginning of 2020, COVID-19 had handicapped ventilation part of V/Q study as stopping all masks of ventilation methods. Adding to that, preference of physicians to send patients for CT directly as apart of CT era for chest infection evaluation, together with D-dimer level, then anti-coagulant became a part of management protocol for all D-dimer level above normal value. That had an advantage for our study to use SPECT imaging combined with low dose CT as a diagnostic modality without ventilation in meanwhile era time of COVID-19, in addition to clinical probability and D-dimer level.
Statistical analysis
Data were gathered, edited, coded and put into IBM SPSS version 23 of the statistical package for social science. The mean, standard deviations and ranges were used to portray the quantitative data with a parametric distribution. Qualitative factors were also shown as percentages and numbers. Then, the comparison between groups was done with the proper statistical analyses. The confidence interval was set to 95% and the margin of error accepted was set to 5%.
Results
81 patients with suspected pulmonary embolism (18 male and 63 female with a mean age of 43.36 ± 14.32 years), 77.8% of those patients were complaining of SOB either as the only presenting symptom or associated with other complaint, such as chest pain, cough etc. The classic triad (Chest pain+cough+hemoptysis) was reported in 2 patients. The less frequent presenting symptoms were hemoptysis with frequency 2.5% (Table 1).
| No=81 | ||
|---|---|---|
| Age | Mean ± SD | 43.36 ± 14.32 |
| Range | 19-72 | |
| Sex | Females | 63 (77.8%) |
| Males | 18 (22.2%) | |
Table 1: Age and sex of the cases.
Patients were categorized according to modified well’s criteria by the doctor in charge into high (33.3%), moderate (29.6%) and low (37.0%) pretest probability presented in Table 2. 59 patients (72.8%) above normal D-dimer test, while the below normal value were 22 patients (27.2%). Pulmonary Hypertension (PTH) that detected by echocardiography were 62 patients (76.5%) with level range between 40 mm/Hg-90 mm/Hg (55.53 mm/Hg ± 13.24 mm/Hg), 22 of high PHT patients (35.5%) their main indication of V/Q study was suspected CTEPH. 57 patients (70.4%) were known to have chronic illness varies between DM, HTN, IHD bronchial asthma, COPD and ILD [16-20].
| Clinical probability | No=81 |
|---|---|
| Low | 30 (37.0%) |
| Moderate | 24 (29.6%) |
| High | 27 (33.3%) |
Table 2: Pre-test clinical probability according to well’s criteria.
The distribution of the perfusion tracer showed no defects in 52 patients (64.2%), while 29 patients showed pleural based segmental defects, ranging between 1-12 defects (4.26 ± 3.69), 14.8 % were single defect and 21.0% were multiple defects. The trans-axial, coronal or sagittal SPECT images showed new defects in 16 patients (19.8 %), 12 patients of them revealed single more defect, while 4 patients showed 2 pleural based segmental defects. Due to COVID-19 pandemic, only 27 patients of our study population have been performed the ventilation imaging on the other day and according to modified PIOPED II criteria: 13 patients (48.1%) with high probability, 10 patients (37.0%) with low probability and 4 patients (14.8%) classified as normal (no patient categorized as nondiagnostic) [21-25].
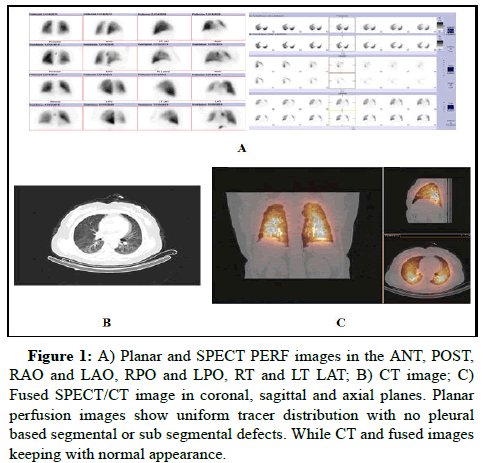
According to 2009 EANM VQ guidelines for PE diagnosis, we diagnosed the 81 patients with perfusion SPECT/CT to either, there is PE: 25 patients (30.9%) or No PE: 56 patients (69.1%) shown in Table 3 and Figure 1.
| SPECT/CT | No=81 |
|---|---|
| No | 56 (69.1%) |
| Yes | 25 (30.9%) |
Table 3: Number and percentage of patients with or without PE by SPECT/CT.
A 45-year-old woman with SOB arrived at the emergency room; her D-dimer test result was 741 ng/ml. According to well’s criteria she had low pre-test clinical probability and no pulmonary hypertension and she has not known to have chronic illness. A 58-year-old female,
Figure 1: A) Planar and SPECT PERF images in the ANT, POST, RAO and LAO, RPO and LPO, RT and LT LAT; B) CT image; C) Fused SPECT/CT image in coronal, sagittal and axial planes. Planar perfusion images show uniform tracer distribution with no pleural based segmental or sub segmental defects. While CT and fused images keeping with normal appearance.
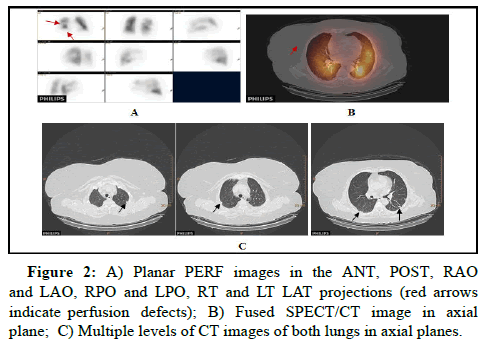
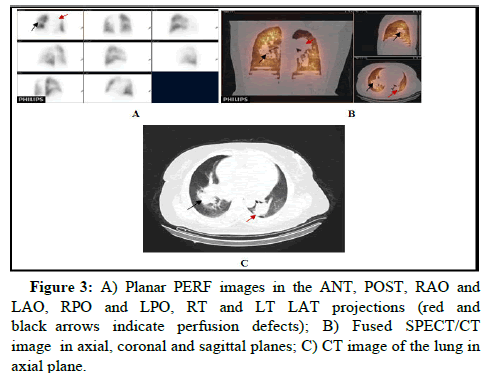
In addition to other diagnostic findings by low dose CT: GGO (10 patients), atelectasis and fibrotic bands (14 patients), pleural effusion (8 patients), lung mass and sub-pleural nodules (6 patients) as shown in Figure 2, while the enlarged cardiac size and prominent vessels detected in 28 patients represented in Figure 3. The diagnosis of 6 patients were changed after low dose CT, by confirmed that the defects were not corresponded to segmental or sub-segmental pleural based parenchymal lung lesion.
A 58-year-old female, presented with SOB and the D-dimer was above the normal value, who’s a known case of Wegner granulomatosis on Xalerto anti-coagulant. She has suffered from DVT a year ago, which raised the pre-clinical probability to be high.
Planar perfusion pictures of the right lung demonstrate many wedge shaped pleural based abnormalities, whereas SPECT/CT is compatible with the pattern of a pulmonary embolism (2009 EANM recommendation for PE diagnosis). On the co-registered CT scan, there are no related parenchymal abnormalities, although wedge shaped perfusion deficiencies on the pleura are visible on Q-SPECT pictures (mismatched). Small, many, bilateral sub-pleural pulmonary nodules are seen (black arrows).
A 48-year-old female, presented with SOB. She has past history of PE and and the pre-clinical probability is high. Echocardiography of the patient revealed 50 mm/Hg and the D-dimer is below the average.
Planar perfusion images show medium size pleural based defects at the upper lobe of the left lung and middle lobe of the right lung. QSPECT/ CT confirmed its prominent dilated mediastinal vessel (red arrow) on the left side as well as parenchymal lung mass on the right lung (black arrow), which rule out the presence of PE (2009 EANM guideline for PE diagnosis).
There was statistically highly significant relation between presence or absence of PE by SPECT/CT imaging and clinical probability (pvalue= 0.000). All 25 patients diagnosed with PE had high D-dimer, while 22 patients had low D-dimer diagnosed with no PE, then there was statistically highly significant relation (p-value=0.000). There was also statistically significant relation also with PHT (p-value=0.028) and chronic illness (p-value=0.004). There was highly significant relation between SPECT/CT results and modified PIOPED probability in diagnosis of PE (p-value=0.004) shown in Tables 4 and 5.
| SPECT/CT | Test value* | P-value | Sig. | |||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| No=56 | No=25 | |||||
| Clinical probability | Low | 30 (53.6%) | 0 (0.0%) | 26.499 | 0 | HS |
| Moderate | 16 (28.6%) | 8 (32.0%) | ||||
| High | 10 (17.9%) | 17 (68.0%) | ||||
| D-dimer | Below average | 22 (39.3%) | 0 (0.0%) | 13.484 | 0 | HS |
| Above average | 34 (60.7%) | 25 (100.0%) | ||||
| Pulmonary hypertension | Negative | 17 (30.4%) | 2 (8.0%) | 4.812 | 0.028 | S |
| Positive | 39 (69.6%) | 23 (92.0%) | ||||
| Chronic illness | Negative | 22 (39.3%) | 2 (8.0%) | 8.114 | 0.004 | HS |
| Positive | 34 (60.7%) | 23 (92.0%) | ||||
Note: P-value>0.05: Non-significant; P-value<0.05: Significant; P-value<0.01: Highly significant; *Chi-square test
Table 4: Relations of presence or absence of PE by SPECT/CT and clinical probability, D-dimer, PHT and chronic illness.
| SPECT/CT | Modified PIOPED probability | Test value | P-value | Sig. | |||
|---|---|---|---|---|---|---|---|
| Normal+low | High | ||||||
| No. | % | No. | % | ||||
| No | 12 | 85.70% | 0 | 0.00% | 20.057 | 0 | HS |
| Yes | 2 | 14.30% | 13 | 100.00% | |||
Note: P-value>0.05: Non-significant; P-value<0.05: Significant; P-value<0.01: Highly significant
Table 5: Relation between modified PIOPED and SPECT/CT in PE diagnosis.
13 patients out of 27 patients who had been identified positive for PE by SPECT/CT modality, showed concordance (positive) on planar V/Q scan (high modified PIOPED probability) considered as true positive and two more patients showed discordance (positive by SPECT/CT and negative or low/normal by modified PIOPED) considered as false positive on the SPECT/CT [26].
12 patients out of 27 patients who had been identified as negative for PE by SPECT/CT, showed concordance (negative) on planar V/Q scan (low/normal modified PIOPED probability) considered as true negative, with no false negative considered.
Discussion
A frequent and potentially deadly condition, pulmonary embolism can be treated successfully to increase survival chances. After myocardial infarction and stroke, pulmonary embolism is the third most prevalent acute cardiovascular illness and it frequently remains undiagnosed, which results in thousands of fatalities every year. According to post mortem research, pulmonary embolism affects 65% of hospitalized patients. According to estimates, PE is the only reason that accounts for 7% of hospital deaths. Clinical suspicion is necessary to make the diagnosis of pulmonary embolism. Although in practical practice, this is not always possible. Due to the non-specific character of its signs and symptoms, which are commonly found in various cardiac and pulmonary diseases, pulmonary embolism is usually underdiagnosed.
From patient to patient, pulmonary embolism can appear in a variety of clinical ways. The most prevalent presenting symptom is dyspnea. A secure, noninvasive method to assess local pulmonary perfusion and ventilation has been the V/Q lung scan. The method has been extensively used to assess individuals with suspected PE. The perfusion scan may underestimate perfusion problems despite imaging in many projections. Modern nuclear medicine diagnostics frequently employ the widely utilized imaging technique known as SPECT. Planar acquisitions have almost entirely been superseded by tomographic scans, particularly in the departments of cardiology and neurology. Several studies have evaluated the efficiency of SPECT in the diagnosis of pulmonary embolism in relation to V/Q lung scintigraphy.
In the present study, among the 52 normal patients by planar perfusion scan, 48 patients still entirely normal on SPECT with no evidence of abnormal segmental or subsegmental perfusion defects detected. SPECT add small segmental defect in 16 patients, 2 of them (7.4%) were converted from entirely normal or low probability to high probability for PE and another 2 patients confirmed with ventilation and later by low dose CT that their perfusion defects detected were from dilated vessel. While rest of the new defects in the remaining 12 patients just added to already known defects, although didn’t change the probability of PE present.
At the segmental level, the rise was still sizable (12.8%), but Reinartz, et al., demonstrated that it was not statistically significant (Pvalue= 0.401). The significantly higher sensitivity, specificity and accuracy of SPECT in compared to planar scintigraphy reflect its greater detection rate. Additionally, Collart, et al., demonstrated that the number of observable defects by SPECT may be greatly enhanced by 82.6% when compared to that of planar scintigraphy (P=0.01). In comparison between SPECT scans and planar images at the segmental level by Reinartz, et al., showed no significant difference in categorization with our study results.
To rule out other potential causes of aberrant perfusion (such as pneumonia, bullous emphysema or malignancy), ventilation scintigraphy is used as part of the V/Q-SPECT. In theory, a thoracic noncontract-enhanced CT may likewise do this. Additionally, a straightforward non-contrast-enhanced CT scan may offer important details on related thoracic diseases. Gradinscak, et al., investigated the possibility of replacing breathing scans with a combination of CT and SPECT perfusion. The research comprised 30 individuals who completed SPECT (V/Q) and CT-MDCT exams and were thought to have PE. Embolic deficiencies were defined as perfusion deficits without pulmonary parenchymal abnormalities. 96 embolic flaws were visible on the SPECT (V/Q) pictures and 87% of them were also identified as embolic defects by the MDCT data. According to the authors, false-negative defects based on MDCT images were seen for atelectatic foci, which were less severe than perfusion defects, while false-positive defects were seen in two patients with bronchial asthma because of air trapping. Gradinscak, et al., came to the conclusion that SPECT (Q)+MDCT scanning may be thought of as a backup strategy in the absence of ventilation scanning [27].
With a much lower proportion of false-negative and nondiagnostic images, this study shows that perfusion SPECT/CT imaging has a greater diagnostic accuracy than traditional V/Q planar imaging when interpreted using modified PIOPED II criteria. We further demonstrate that perfusion SPECT/CT interpretation is more consistently read by readers than planar imaging. We follow a trend in the literature that seeks to simplify the interpretation of lung scintigraphy by mandating a binary interpretation of PE present or PE missing. In addition to replacing the chest radiograph, the low dosage CT scan may potentially discover significant structural anomalies that would otherwise go unreported. According to Yang Lu, et al., study, the lowdose CT scan revealed new diagnostic findings in around 72% of patients, often offering a suitable alternative explanation for the presenting symptoms (such as an infectious disease or significant effusions). Despite this, pulmonary infarction-related CT scan anomalies may cause perfusion SPECT/CT scans to be interpreted as falsely negative.
When V/Q SPECT datasets alone were evaluated in a study by Gutte, et al., 6 patients had false-positive PE diagnoses, 3 patients had mismatched defects on the V/Q SPECT scans due to interlobar fissures and 3 patients with chronic obstructive pulmonary disease had mismatched defects due to paraseptal emphysema, pneumonic infiltration, atelectasis and pleural fluid. Low-dose CT revealed all of these lesions.
46.9% of the patients in the current research had additional diagnostic findings, including GGO (10 patients), atelectatic and fibrotic bands (14 patients), pleural effusion (8 patients), lung mass and sub-pleural nodules (6 patients). Our study's objective is to evaluate the possible advantages and diagnostic potency of combining Low Dose-CT with perfusion SPECT without the use of contrast agents for the diagnosis of pulmonary embolism. PE, 81 individuals had planar perfusion, in addition to SPECT study combined with low dose CT, however regrettably only 27 patients finished the ventilation planar study the other day due to the COVID-19 epidemic. The prevalence of PE was 48.1% when utilizing the modified PIOPED II criteria for diagnosis; however it was only 30.86% when using SPECT/CT. By taking the PIOPED as a gold standard and using ROC curve, the SPECT/CT was found a sensitivity of 100.0%, specificity of 85.7% and accuracy of 92.6%.
Only a small number of studies have been published in the literature that discusses the use of the hybrid SPECT/low-dose CT technology in the diagnosis of PE. In the research by Palmowski, et al., which assessed the usefulness of perfusion SPECT/CT in the diagnosis of PE, 93 patients with a suspicion of PE underwent V/Q planar scanning (a reference test) and low-dose CT. The SPECT/CT (Q) scans revealed that PE was identified when scintigraphy revealed perfusion abnormalities while lung CT was unremarkable. However, the authors didn't go into great detail about the diagnostic standards they used. Perfusion SPECT/CT's sensitivity and specificity were 95.8% and 82.6%, respectively which is lower than the values found in the current investigation.
In comparison to multidetector CT angiography, Gutte, et al., recently reported the identification of PE using combined V/Q SPECT and low-dose CT. They demonstrated that low-dose CT and Q-SPECT had a sensitivity of 93%, but only a poor specificity of 51%. The specificity in our sample was too high at 85.7%, while the sensitivity was lower than our finding of 100%.
On the other hand, Le Roux, et al., study, which included 393 patients overall, evaluated the potential value of combining a concurrent low dose CT with a V/Q SPECT procedure carried out on a hybrid SPECT/CT camera for the diagnosis of PE. The important takeaway is that there is a substantial danger of over diagnosis when low dose CT is used in place of ventilation SPECT. They draw the conclusion that low dose CT cannot substitute ventilation SPECT for PE diagnosis without producing a significant amount of false-positive outcomes since the diagnostic impact of integrating a low dose CT to V/Q SPECT is yet unknown.
PE was subsequently verified in 22 individuals and eliminated in 84, with an incidence of 20% in the study group, according to Yang Lu, et al., study, which examined 106 patients at a cancer center from 2006 to 2010. With a much lower incidence of false-negative and nondiagnostic images, perfusion SPECT/CT imaging provides a greater diagnostic accuracy than traditional V/Q planar imaging when evaluated using PIOPED II criteria (P=0.001). However, the study contends that perfusion SPECT/CT scanning is capable of replacing conventional planar V/Q scintigraphy since it has a high diagnostic accuracy for identifying PE in a cancer population. In most situations, the concomitant low dose CT scan provides clinically useful information [28].
We discovered that the findings of our investigation were substantially identical to those of the study by Mazurek, et al., which included 109 consecutive patients suspected of having PE between 2010 and 2011. Out of 109 patients, 84 were included for further analysis. The sensitivity and specificity of the planar (Q) scans were 73% and 43%, respectively. The sensitivity and specificity of the SPECT (Q) scans were 88% and 47%, respectively. The sensitivity increased to 100% and the specificity to 83% when CT was added SPECT/CT (Q). In comparison to our present study the sensitivity in detecting PE is similar, while the specificity by detecting a false positive is lower than our result.
Seventy five patients with probable PE underwent SPECT (V/Q) and CT procedures, according to Viau, et al. The PE diagnostic criteria from EANM were used. SPECT (V/Q) had a sensitivity and specificity of 88 and 93%, whereas SPECT/CT (Q) had a sensitivity and specificity of 100 and 82%, respectively (p value not significant). The findings indicate that SPECT/CT perfusion may be successfully used in place of V/Q scintigraphy, provided that the findings be validated in a broader patient population [29].
We are conscious that one of the research group's drawbacks is its relatively small size, which has an impact on the test's relevance. We experienced a protracted pandemic that significantly decreased the number of nuclear medicine tests, particularly ventilation of the lung scintigraphy. Our study's inability to document comorbidities and the doctor's final clinical diagnosis is another drawback. But it was not the purpose of our inquiry. We set out to demonstrate both the benefits and drawbacks of using Q-SPECT in a contemporary hybrid SPECT/CT system alongside a non-contrast enhanced CT scan.
Conclusion
The addition of low dose CT to the lung perfusion SPECT boosts the test's diagnostic yield by revealing other diseases that might be responsible for the symptoms being observed. By increasing specificity, it becomes possible for one imaging scan to accurately diagnose PE while simultaneously ruling out a number of other explanations of SOB and chest discomfort.
References
- Bajc M, Neilly JB, Miniati M, Schuemichen C, Meignan M, et al. (2009) EANM guidelines for ventilation/perfusion scintigraphy: Part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging 36: 1356-1370.
- Mortensen J, Gutte H (2014) SPECT/CT and pulmonary embolism. Eur J Nucl Med Mol Imaging 41: 81-90.
[Crossref] [Google Scholar] [PubMed]
- Begic A, Opankovic E, Cukic V, Rustempasic M, Basic A, et al. (2015) Impact of ventilation/perfusion single photon emission computed tomography on treatment duration of pulmonary embolism. Nucl Med Commun 36: 162-167.
[Crossref] [Google Scholar] [PubMed]
- Kan Y, Yuan L, Meeks JK, Li C, Liu W, et al. (2015) The accuracy of V/Q SPECT in the diagnosis of pulmonary embolism: A meta-analysis. Acta Radiol 56: 565-572.
[Crossref] [Google Scholar] [PubMed]
- Le Roux PY, Pelletier-Galarneau M, de Laroche R, Hofman MS, Zuckier LS, et al. (2015) Pulmonary scintigraphy for the diagnosis of acute pulmonary embolism: A survey of current practices in Australia, Canada and France. J Nucl Med 56: 1212-1217.
[Crossref] [Google Scholar] [PubMed]
- Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, et al. (2014) 2014 ESC Guidelines on the diagnosis and management of acute pulmonary embolism: The task force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC) endorsed by the European Respiratory Society (ERS). Eur Heart J 35: 3033-3073.
[Crossref] [Google Scholar] [PubMed]
- Mariani G, Bruselli L, Kuwert T, Kim EE, Flotats A, et al. (2010) A review on the clinical uses of SPECT/CT. Eur J Nucl Med Mol Imaging 37: 1959-1985.
[Crossref] [Google Scholar] [PubMed]
- Buck AK, Nekolla S, Ziegler S, Beer A, Krause BJ, et al. (2008) SPECT/CT. J Nucl Med 49: 1305-1319.
[Crossref] [Google Scholar] [PubMed]
- Bybel B, Brunken RC, DiFilippo FP, Neumann DR, Wu G, et al. (2008) SPECT/CT Imaging: Clinical Utility of an emerging technology. Radiographics 28: 1097-1113.
[Crossref] [Google Scholar] [PubMed]
- Patel CN, Chowdhury FU, Scarsbrook AF (2009) Hybrid SPECT/CT: The end of “unclear” medicine. Postgrad Med J 85: 606-613.
[Crossref] [Google Scholar] [PubMed]
- Sostman HD, Stein PD, Gottschalk A, Matta F, Hull R, et al. (2008) Acute pulmonary embolism: Sensitivity and specificity of ventilation perfusion scintigraphy in PIOPED II study. Radiology 246: 941-946.
- Miniati M, Pistolesi M, Marini C, Di Ricco G, Formichi B, et al. (1996) Value of perfusion lung scan in the diagnosis of pulmonary embolism: Results of the Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis (PISA-PED). Am J Respir Crit 154: 1387-1393.
[Crossref] [Google Scholar] [PubMed]
- Amin A, Hamid M, Moustafa H, Sami H. The diagnostic dilemma of pulmonary embolism: Is it a clinico investigatory portrayal or only an investigatory portrayal? Nuclear Med 35: 17-25.
- Roy PM, Colombet I, Durieux P, Chatellier G, Sors H, Meyer G (2005) Systematic review and meta-analysis of strategies for the diagnosis of suspected pulmonary embolism. BMJ 331: 259.
[Crossref] [Google Scholar] [PubMed]
- Piazza G, Goldhaber SZ (2006) Acute pulmonary embolism: Part I: Epidemiology and diagnosis. Circulation 114: 28-32.
[Crossref] [Google Scholar] [PubMed]
- Worsley DF, Alavi A (2003) Radionuclide imaging of acute pulmonary embolism. Semin Nucl Med 33: 259-278.
- Reinartz P, Schirp U, Zimny M, Sabri O, Nowak B, et al. (2001) Optimizing ventilation-perfusion lung scintigraphy: Parting with planar imaging. Nuklearmed Nucl Med 40: 38-43.
[Google Scholar] [PubMed]
- Bajc M, Bitzen U, Olsson B, Perez de Sa V, Palmer J, et al. (2002) Lung ventilation/perfusion SPECT in the artificially embolized pig. J Nucl Med 43: 640-647.
[Google Scholar] [PubMed]
- Collart JP, Roelants V, Vanpee D, Lacrosse M, Trigaux JP, et al. (2002) Is a lung perfusion scan obtained by using single photon emission computed tomography able to improve the radionuclide diagnosis of pulmonary embolism? Nucl Med Commun 23: 1107-1113.
[Crossref] [Google Scholar] [PubMed]
- HF C (1997) Diagnostic usefulness of lung SPET in pulmonary thromboembolism: An outcome study. Nucl Med Commun 18: 897-906.
- Biersack HJ, Altland H, Knopp R, Winkler C (1982) Single photon emission computed tomography of the lung: Preliminary results. Eur J Nucl Med 7: 166-1670.
[Crossref] [Google Scholar] [PubMed]
- Reinartz P, Wildberger JE, Schaefer W, Nowak B, Mahnken AH, et al. (2004) Tomographic imaging in the diagnosis of pulmonary embolism: A comparison between V/Q lung scintigraphy in SPECT technique and multislice spiral CT. J Nucl Med 45: 1501-1518.
[Google Scholar] [PubMed]
- Palmowski K, Oltmanns U, Kreuter M, Mottaghy FM, Palmowski M, et al. (2014) Diagnosis of pulmonary embolism: Conventional ventilation/perfusion SPECT is superior to the combination of perfusion SPECT and nonenhanced CT. Respiration 88: 291-297.
[Crossref] [Google Scholar] [PubMed]
- Gutte H, Mortensen J, Jensen CV, Johnbeck CB, von der Recke P, et al. (2009) Detection of pulmonary embolism with combined ventilation–perfusion SPECT and low-dose CT: Head-to-head comparison with multidetector CT angiography. J Nucl Med 50: 1987-1992.
[Crossref] [Google Scholar] [PubMed]
- Gradinscak D, Roach PJ, Schembri G, Bailey D (2009) Lung SPECT perfusion scintigraphy: Can CT substitute for ventilation imaging? Eur J Nucl Med Mol Imaging 36: 300-400).
- Mazurek A, Dziuk M, Witkowska-Patena E, Piszczek S, Gizewska A (2015) The utility of hybrid SPECT/CT lung perfusion scintigraphy in pulmonary embolism diagnosis. Respiration 90: 393-401.
[Crossref] [Google Scholar] [PubMed]
- Lu Y, Lorenzoni A, Fox JJ, Rademaker J, Vander Els N, et al. (2014) Noncontrast perfusion single-photon emission CT/CT scanning: A new test for the expedited, high-accuracy diagnosis of acute pulmonary embolism. Chest 145: 1079-1088.
[Crossref] [Google Scholar] [PubMed]
- Le Roux PY, Robin P, Delluc A, Abgral R, Palard X, et al. (2015) Additional value of combining low dose computed tomography to V/Q SPECT on a hybrid SPECT-CT camera for pulmonary embolism diagnosis. Nucl Med Commun 36: 922-930.
[Crossref] [Google Scholar] [PubMed]
- Viau P, Franken P, Padovani B, Koulibaly PM, Benoliel J, et al. (2011) Hybrid imaging in acute pulmonary embolism: Contribution of CT coupled to ventilation and perfusion tomoscintigraphy. Nuclear Med 35: 117-125.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi