Case Report, J Clin Image Case Rep Vol: 5 Issue: 12
A Very Rare Complication of Covid-19: Pneumothorax and Penumomediastinum
Aynur Yurtseven*
Department of Advanced Cardiac Center, PGIMER, Sector 12 Chandigarh, India
*Corresponding Author: Aynur Yurtseven
Department of Emergency Medicine, Diskapi Yildirim Beyazit Education and Training Hospital, Ankara, Turkey
Tel: 05055630173
E-mail: aynuryurt7@gmail.com
Received: November 13, 2021 Accepted: December 14, 2021 Published: December 21, 2021
Citation: Yurtseven A (2021) A Very Rare Complication of Covid-19: Pneumothorax and Penumomediastinum. J Clin Image Case Re 5(12): 194.
Abstract
Background: Pneumothorax and Penumomediastinum are defined as free air within pleural ve mediastinal spaces, respectively. Spontaneous pneumothorax and Penumomediastinum combination is a very rare complication of COVID-19 pneumonia. With this case report we want to underline etiology and possible pathophysiology of these rare complications of COVID-19. At the same time, with this case, we wanted to contribute to the literature in terms of complications that may be seen due to covid-19 infection. Case report: 24 years old male patient visited emergency service due to dyspnea and pleuritic chest pain since 3 days. High resolution thorax CT scan revealed spontaneous pneumothorax, Penumomediastinum and COVID 19 pneumonia. Due to absence of predisposing factors, we considered Penumomediastinum and pneumothorax as rare complications of COVID-19 and administered patient to ICU unit. Conclusion: Spontaneous pneumothorax and Penumomediastinum are rare but significant complications of COVID-19 and should be kept in mind as a differential diagnosis of chest pain and dyspnea at this patient group. Further researches are needed for etiology of Penumomediastinum and pneumothorax due to COVID-19.
Keywords: COVID-19 Pneumonia, Spontaneous pneumothorax, Spontaneous penumomediastinum, Chest Pain
Case Report
24 years old male patient administered to emergency service with pleuritic chest pain and dyspnea of 3 days. Patient had cough with sputum and headache, without loss of taste and loss of smell. He received 2 doses of vaccination with Biontech®, last dose received 2 months ago. Physical examination revealed diffuse rhonchus bilaterally on auscultation, blood pressure 130/80 mmHg, heart rate of 134, body temperature of 36.5°C, plasma glucose 139 mg/dL, respiratory rate of 24 and saturation of 84 at room air. ECG had no specific features with sinus tachycardia. Patient had WBC 18.0000/uL, PLT 229.000 /uL, serum lactate 2, D-Dimer 620 ng/dl and troponin within normal range. COVID-19 RT- PCR test was positive. High resolution computed tomography showed bilateral minimum pneumothorax and Penumomediastinum with peripheral and peribronchovascular focal ground glass opacities compatible with COVID-19 (Figure 1). During emergency service follow-up patient developed haemoptysis and severe dyspnea. Thoracic surgery and cardiovascular surgery consultations are done and no surgical interventions planned. For further follow-up ICU admission was planned.
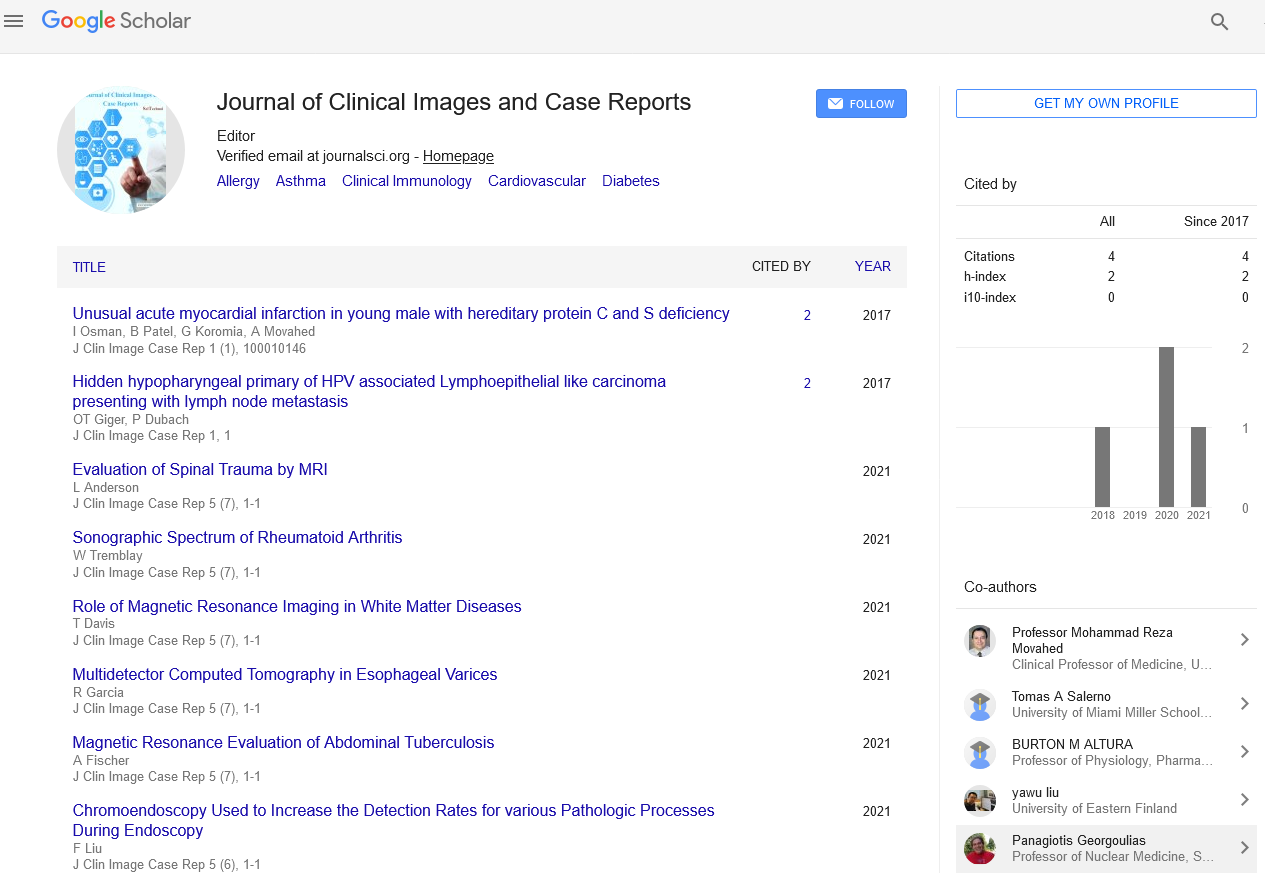
Figure 1: Images of Penumomediastinum and plastering pneumothorax in a patient who presented with Covid 19 pneumonia.
A, C, F: Chest computed tomography scan showing pneumomediastinum, plaster pneumothorax and ground glass image compatible with COVID 19 pneumoniain sagital view.
D, E: Chest computed tomography scan pneumomediastinum, plaster pneumothorax and ground glass image compatible with COVID 19 pneumoniain in coronal view.
B: Chest computed tomography scan pneumomediastinum, plaster pneumothorax and ground glass image compatible with COVID 19 pneumoniain in axial view.
Results and Discussion
COVID-19 virus passes through cell membrane via angiotensin converting enzyme 2 receptor (ACE 2) and induces wide tissue damage by stimulating immune system and causing overreaction. Interleukin 6 (IL 6) is thought to be the main trigger of this overreaction. Another important factor is IL 1B known as main causative agent of widespread lung inflammation and fibrosis [1]. Most frequent radiological findings are early phase reticular changes and mid-late phase ground glass opacities. Distribution of inflammation through lungs is usually bilateral, peripherally located and consolidation increases sequentially [2,3].
During severe acute respiratory syndrome (SARS) outbreak at 2002-2003, a research from Hong Kong, showed increased incidence of spontaneous Penumomediastinum (11.6%) (3). For COVID-19 patient’s incidence of spontaneous pneumothorax and spontaneous Penumomediastinum is not well known yet. Spontaneous pneumothorax incidence of SARS-CoV-2 infected patients is 1-2%, and spontaneous Penumomediastinum incidence is very low [4-6].
We found 15 cases of spontaneous Penumomediastinum of COVID-19 patients from literature review. 7 of these 15 patients had no history of invasive or non-invasive mechanical ventilation and no concomitant spontaneous pneumothorax was diagnosed. 6 patients have concomitant spontaneous pneumothorax. According to literature review, some of these patients’ developed pneumothorax and Penumomediastinum during follow-up while some had these complications at first contact with healthcare system [7]. For our case it was at first medical contact. Researchers declare that the main underlying mechanism for Penumomediastinum and pneumothorax is rather alveolar rupture associated with intense alveolar damage and air leakage throughout bronchoalveolar sheath and not the viral load. Main determinant is thought to be immunological damage. Also, literature review of these patients who mainly had no significant medical history or smoking habit support immune reaction theory. Our case, likewise, had no medical history or smoking habit.
Conclusion
Since spontaneous Penumomediastinum is mostly a self-limiting clinical condition, a conservative approach is preferred first. However, in order to prevent possible serious complications in the course of the disease, it is very important to detect predisposing factors and take precautions accordingly. Thorax CT scan has a very important role in determining the cause of respiratory distress and pulmonary complications associated with COVID-19 in the early period.
Spontaneous Penumomediastinum and spontaneous pneumothorax should be considered in the differential diagnosis of patients with COVID-19 whose general clinical condition worsens. More research is needed to elucidate the underlying pathophysiological process and to determine its true incidence.
Acknowledgments
Authors thank patient’s family members for consent with this publication.
Conflict of Interest
The authors have no conflict of interests to declare.
Ethics Approval
Informed consent was obtained from family of the patient prior writing this case report.
References
- Conti P, Ronconi G, Caraffa A (2020) Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): anti-inflammatory strategies. J Biol Regul Homeost Agents 34(2): 327-331.
- Vancheri SG, Savietto G, Ballati F (2020) Radiographic findings in 240 patients with COVID-19 pneumonia: time-dependence after the onset of symptoms. Eur Radiol 30(11): 6161-6169.
- Barton LM, Duval EJ, Stroberg E, Ghosh S, Mukhopadhyay S, et al. (2020) COVID-19 autopsies, Oklahoma, USA. Am J Clin Pathol 153(6): 725–733.
- Zhou C, Gao C, Xie Y, Xu M, 2020. COVID-19 with spontaneous pneumomediastinum. Lancet Infect Dis 20(4): 510.
- Chen N (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223): 507-513.
- Yang X (2020). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5): 475-481.
- Sami Elhakim T, Haleem Abdul S, Pelaez Romero C , Rodriguez-Fuentes Y. (2020) Spontaneous pneumomediastinum, pneumothorax and subcutaneous emphysema in COVID-19 pneumonia: a rare case and literature review, BMJ 13(12): e239489.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi