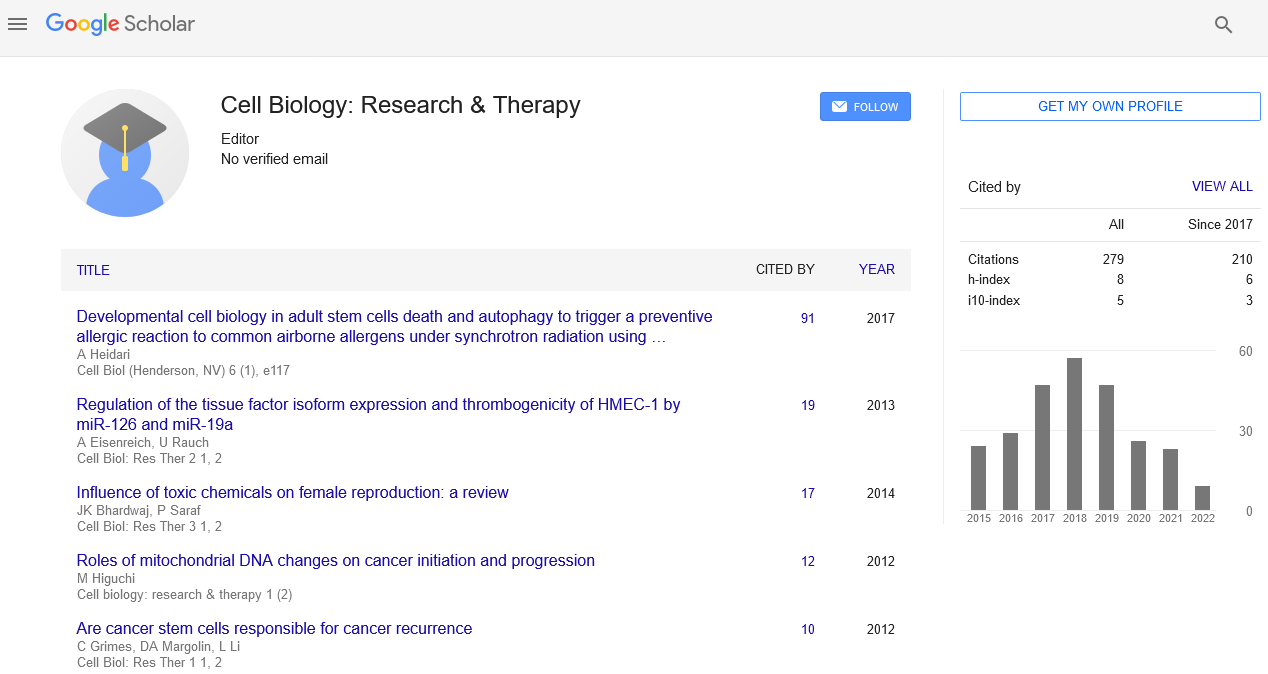
Editorial, Cell Biol Res Ther Vol: 1 Issue: 2
Roles of Mitochondrial DNA Changes on Cancer Initiation and Progression
| Masahiro Higuchi* |
| Department of Biochemistry and Molecular Biology, University of Arkansas for Medical Sciences, Little Rock Arkansas, USA |
| Corresponding author: Masahiro Higuchi, PhD Department of Biochemistry and Molecular Biology, University of Arkansas for Medical Sciences, Little Rock Arkansas, 72205 USA Tel: (501)-526-7520; Fax: (501)-686-8169 E-mail: mhiguchi@uams.edu |
| Received: October 20, 2012 Accepted: October 21, 2012 Published: October 25, 2012 |
| Citation: Higuchi M (2012) Roles of Mitochondrial DNA Changes on Cancer Initiation and Progression. Cell Biol: Res Ther 1:2. doi:10.4172/2324-9293.1000e109 |
Abstract
Roles of Mitochondrial DNA Changes on Cancer Initiation and Progression
Mitochondria are essential organelles that generate ATP through oxidative phosphorylation. This process is accomplished by a series of protein complexes and mitochondrial respiratory chains (MRC) encoded by nuclear DNA and mitochondrial DNA (mtDNA).
Mitochondrial DNA |
|
| Mitochondria are essential organelles that generate ATP through oxidative phosphorylation. This process is accomplished by a series of protein complexes and mitochondrial respiratory chains (MRC) encoded by nuclear DNA and mitochondrial DNA (mtDNA). Human mtDNA is remarkably small (16,569 bp) compared with nuclear DNA (approximately 109 bp) and encodes only a few but important proteins in the MRC: 13 polypeptides, 7 in complex I, cytochrome b in complex III, 3 in complex IV and 2 in complex V (F0-F1 ATPase), 22 transfer RNAs, and 2 ribosomal RNAs (Anderson, 1981 #1323). The majority of mitochondrial respiratory proteins (at least 74) are encoded by nuclear DNA that are translated in the cytoplasm and then imported into mitochondria. | |
Cancer and mtDNA Changes |
|
| Inhibition of the repair system for damages to mtDNA, detoxification of ROS, or increase in ROS encoded in nuclear DNA induces a lot of point mutations of mtDNA, accumulation of large-deletion mutant mtDNA, and the depletion of mtDNA. In addition, nuclear DNA mutations of the mitochondrial proteins, such as adenine nucleotide translocator 1 (ANT1) [1], Twinkle [2], and polymerase γ [3], can cause depletion and multiple deletions of mtDNA. | |
| Several studies demonstrated that mtDNA mutation is common in cancer [4,5]. Mutation of mtDNA was observed in all of the 13 coding regions, two ribosomal RNA regions, D-loop region and transfer RNA regions [5]. Frequency of mtDNA mutation is highest in D-loop region. D-loop region is non-coding displacement (D)- loop (~ 1,122 base pairs) that harbors the main promoter for the transcription of the heavy strand and the light strand of the genome. Mutation to the D-loop region causes reduction of mtDNA content [6]. Frequency of mutation is also higher in complex I region as compared with other regions. Deletion of mtDNA was also observed in several cancers [7]. Thus, association of mtDNA changes to cancer is well accepted. However, Palanichamy and Zhang indicated that more care should be taken to eliminate artifacts and mix-ups especially for clinical samples [8]. | |
| Next, I would like to demonstrate how and whether mtDNA changes regulate cancer. I will talk about the roles of mtDNA changes on two phenotypes “cancer initiation” (cancer occurrence) and “progression to aggressive phenotype” (cancer development) which are sometimes considered equal. | |
mtDNA Change and Cancer Initiation |
|
| Rasmussen et al. showed that mtDNA mutation increases in the frequency of the mutation of nuclear DNA dependent or independent of reactive oxygen species [9]. They hypothesized that these events may lead to cancer initiation and progression. Regarding cancer initiation, however, a contradictory report was published by Akimoto et al. using xenographic tumor formation model [10]. They showed that genome chimera cells (Cybrids) carrying nuclear DNA from tumor cells and mtDNA from normal cells formed tumor, whereas those carrying nuclear DNA from normal cells and mtDNA from tumor cells did not. These observations provided direct evidence that nuclear DNA, but not mtDNA, is responsible for cancer initiation at least in a short term. Human 8-oxoguanine DNA glycosylase 1 (hOGG1) gene is a repair enzyme of mtDNA. Zang et al. showed that hOGG1 overexpression in mitochondria increased mutation in mtDNA [11] and that generated hOGG1 transgenic mouse showed obesity and increased frequencies of malignant lymphoma [12]. This report clearly demonstrates that mtDNA damages can induce cancer initiation. | |
mtDNA Changes and Cancer Progression to an Aggressive Phenotype |
|
| mtDNA damage generally induces reduction of oxidative phosphorylation leading to the reduction of ATP synthesis and oxygen consumption. Another potential change induced by mtDNA damage is ROS generation. Specific inhibition of MRC complex I [13] and complex III [14] generates ROS, and therefore, specific mutation of mtDNA may generate dysfunctional complex I and/or complex III to generate ROS. | |
| First of all, to demonstrate the role of mtDNA damage on cancer progression, mitochondrial genomic knock-out (ρ0) with deficient in respiration has been utilized. Amuthan et al. showed that depletion of mtDNA induces aggressive phenotype leading to invasion [15]. We previously showed that TNF and serum starvation could not induce TNF-induced apoptosis in ρ0 cells, whereas they induced apoptosis in parental cells and cells reconstituted with normal mtDNA [16]. We also showed that AKT activation is responsible for the inhibition of apoptosis in ρ0 cells [17]. These results suggest that mtDNA change is associated with apoptosis-resistance phenotype of cancer. Additionally, Reduction of mtDNA content shifted androgen-dependent prostate cancer cells to an androgenindependent phenotype in vitro and in vivo [18], induced epithelial to mesenchymal transition changes [19] and silencing of putative tumor suppressor genes by hyper methylation of CpG islands [20]. Several signaling associated with cancer progression such as NF-κB [21,22], AKT [17-23,24], AP-1 [25], ERK [19], JNK [19] and Calcineurin [26] can be induced in ρ0 cells. | |
| In addition to the inhibition of oxidative phosphorylation, mutation to the specific coding site of mtDNA may induce ROS generation. To investigate the roles of specific mtDNA mutation on cancer progression, several researchers utilized cybrid cells. In these experiments, cybrid cells have nuclear DNA from cancer cells with specific mtDNA mutation. Cybrid cells with specific mutant mtDNA in ND6 region in an in vivo mouse model system induces metastatic phenotype, suggesting that specific mutations ND6 in complex I give a survival advantage and induce metastasis [27]. Additionally, several investigators showed enhanced growth of tumor size of cybrids with mutant mtDNA in vivo [28,29]. | |
| Regarding similarity of ρ0 and cybrids with specific mtDNA mutation, both cell types share the phenotype induced by the inhibition of respiratory function leading to reduction of ATP synthesis and inhibition of oxygen consumption. In contrast, ROS generation may be only induced in cybrid with mtDNA mutation since superoxide generation in ρ0 cells are generally inhibited [9,22] although contradictory results was reported [30]. When investigating cybrid with mutated mtDNA, the copy number of mtDNA needs to be investigated since reduction of mtDNA content may occur in cybrid with specific mtDNA mutation [31] and such cybrid will show ρ0 phenotype. | |
Mechanisms How mtDNA Damage Induces Aggressive Phenotype |
|
| Since ROS can activate the receptor tyrosine kinase [32,33], Ras [33], phosphatidylinositol 3’kinase pathways [32], NF-κB [34] and JNK [35], ROS from the cells with mutated mtDNA may activate these signaling leading to an aggressive phenotype. It is generally believed that ROS is generated in the cells with dysfunctional respiratory chain by donating electron from MRC to oxygen molecules. However, Lu et al. showed new pathways that cells with damaged mtDNA activates NADPH oxidase and induces ROS generation [36]. This alternative pathway should be considered for the roles of ROS in cells with damaged mtDNA. | |
| Pelicano et al. showed how AKT is activated in the cells with damaged mtDNA [37]. They showed that increase in NADH by respiratory deficiency inactivates phosphatase and tensin homolog (PTEN) through redox modification mechanism, leading to Akt activation. | |
Regulation of Ras Pathway by Intracellular Oxygen Concentration Regulated by mtDNA |
|
| Ras signaling is one of the most important signaling to induce cancer initiation and progression [38]. Cook et al. showed that intracellular oxygen concentration regulated by mtDNA is responsible for cancer progression [39]. Loss of mtDNA content reversibly induced activation of proto-oncogenic Ras responsible for the activation of AKT and ERK leading to cancer progression. Ras activation was mediated by high farnesylation induced by the overexpression of 3-hydroxy-3-methyl-glutaryl-CoA reductase (HMGR), the rate-limiting enzyme of the mevalonate pathway. Hypoxia is known to induce proteasomal degradation of HMGR [40,41]. Well-differentiated cancer cells had high mtDNA content, consumed a large amount of oxygen and induced intracellular hypoxia. Loss of mtDNA reduced oxygen consumption and increased in oxygen concentration in the cells. The hypoxic-to-normoxic shift led to the overexpression of HMGR through inhibiting proteasomal degradation. Therefore, damage to mtDNA induced overexpression of HMGR through hypoxic to normoxic shift. Subsequently, the endogenous induction of the mevalonate pathway activated Ras that mediates advanced phenotype. The results elucidate a coherent mechanism that directly links the mitochondrial genome with the advanced progression of the disease. | |
| Taken together, several mechanisms are generated by mtDNA damage(s) and may work cooperatively to induce cancer progression. A confirmation and an understanding of the underlying mechanisms for cancer initiation and progression induced by mtDNA damage will lead to early detection of the potential aggressive cancer, novel approaches for targeted prevention, or therapy for prostate cancer. | |
References |
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi