Research Article, J Spine Neurosurg Vol: 7 Issue: 3
True Recurrent Lumbar Disc Herniation And Arterial Hypertension: Is There Any Relation?
Reihani-Kermani H1*, Saidi S1, Zolala F2, Reihani A3 and Mehrabian M1
1Department of Neurosurgery, Shahid Bahonar hospital, Kerman University of Medical Sciences, Kerman, Iran
2Department of Epidemiology, Kerman University of Medical Sciences, Kerman, Iran
3Department of Life science, McMaster University, Hamilton, Ontario, Canada
*Corresponding Author : Hamed Reihani-Kermani, MD
Associate professor of Neurosurgery, Department of Neurosurgery, Shahid Bahonar Hospital, Neuroscience research center, University of Medical Sciences, Hezaroyekshab Street, Alley 5, Kerman, Iran, Postal code: 76186-53771
Tel: + 98 913 140 2160
E-mail: h_reihani@hotmail.com
Received: June 04, 2018 Accepted: June 15, 2018 Published: June 22, 2018
Citation: Reihani-Kermani H, Saidi S, Zolala F, Reihani A, Mehrabian M (2018) True Recurrent Lumbar Disc Herniation and Arterial Hypertension: Is There Any Relation? J Spine Neurosurg 7:3. doi: 10.4172/2325-9701.1000299
Abstract
Cardiovascular risk factors and atherosclerosis are associated with lumbar disc herniation. However, studies fail to identify a consistent risk factor for the recurrence. To investigate the association between cardiovascular risk factors and true recurrent of lumbar disc herniation, 186 patients who underwent unilateral microdiscectomy for intractable radiculopathy due to lumbar disc herniation were enrolled in this cross-sectional study. One surgeon performed all operations, and all patients were treated with the same procedure. The follow-up period was between 6 months to 5 years. The association between some cardiovascular risk factors e.g. hypertension, diabetes, hyperlipidemia, smoking and true recurrent lumbar disc herniation investigated using logistic regression analysis. Sixty-nine patients with true recurrence of lumbar disc herniation (RLDH group) were compared to 117 patients who were surgically treated with no recurrence of lumbar disc herniation (LDH group). The differences of age, gender, diabetes, morphine addiction, hyperlipidemia and smoking between two groups were not statistically significant. The prevalence of hypertension in RLDH and LDH was 61.5% and 38.5% respectively. The difference was significant (p<0.001). The logistic regression analysis showed the recurrence rate was significantly higher in hypertensive patients (OR: 1.74-7.55, CI: 95%, P = 0.001). Furthermore, there was no correlation between confounding factor of medications, diabetes, history of cardiovascular disease, hyperlipidemia, duration of the symptom-free interval, gender and the true recurrence. The results of this preliminary study showed that there might be a possible relation between arterial hypertension and true recurrence of lumbar disc herniation, so it would be advisable to pay more attention to hypertensive patients who have been operated.
Keywords: Arterial hypertension; Lumbar disc herniation; Recurrence
Introduction
In the face of favorable results of most lumbar microdiscectomies, about 7% of patients develop a recurrence at the primary surgical site [1]. Various risk factors for recurrent lumbar disc herniation (RLDH) have been noted. However, studies fail to identify a consistent risk factor for RLDH. It has been shown that cardiovascular risk factors are associated with lumbar disc herniation (LDH). Also, atherosclerosis may be involved in disc degeneration [2,3]. Accordingly, we hypothesized that some risk factors for cardiovascular and atherosclerosis might predispose the treated lumbar discs to recurrence as well. This study aimed to examine associations between these risk factors and the lumbar disc herniation recurrence at the same level and side.
Materials and Methods
Sixty-nine patients who had undergone microdiscectomy for true recurrence of lumbar disc herniation were included in this retrospective study from 2008 to 2016. All patients had a unilateral herniated disc at a single level and had no other spinal disorders such as spondylolisthesis, spondylolysis, spinal stenosis and deformities. All obese patients (BMI>30) were excluded. Diagnosis of primary and recurrence disc herniation was based on clinical findings and magnetic resonance imaging (MRI).
The first and second operations were conducted in patients with intractable radiculopathy. The only procedure performed was a unilateral single-level microdiscectomy. The degenerated nucleolus was evacuated as much as possible after unilateral partial hemilaminectomy and flavectomy using straight and angled pituitary forceps down to the anterior longitudinal ligament. One surgeon performed all surgeries. The follow-up time was between 6 months to 5 years. True recurrence of disc herniation was defined as a radiculopathy in association with compatible lesion confirmed by MRI at the same level and side as that of the primary surgical site. Patients with recurrent disc herniation on the other side or with a herniation at different levels and those with concomitant spinal disorders including epidural fibrosis were excluded. The same surgeon also operated all RLDH patients. Controls (N=117) were selected among unilateral single-level disc operated patients who had no recurrence.
Patient’s data about cardiovascular and atherosclerosis risk factors including diabetes, hypertension (HTN), hyperlipidemia, smoking and opium addiction were collected. Documented high systolic and diastolic blood pressure that was diagnosed by internist or cardiologist considered as HTN. All hypertensive patients had been treated by antihypertensive agents and were normotensive at the time of recurrence. Morphine addiction was included as a risk factor according to the evidence of the effect of morphine on intervertebral discs and serum lipids [4,5].
Most of the data gathered from patients’ medical files and the missing information were retrieved through phone calls. The university Review Board of Medical School approved the study. The absolute and relative frequencies of central tendency were used to describe data. Also, the t-test, ANOVA, logistic regression and Pearson correlation coefficient were used for data analysis.
Results
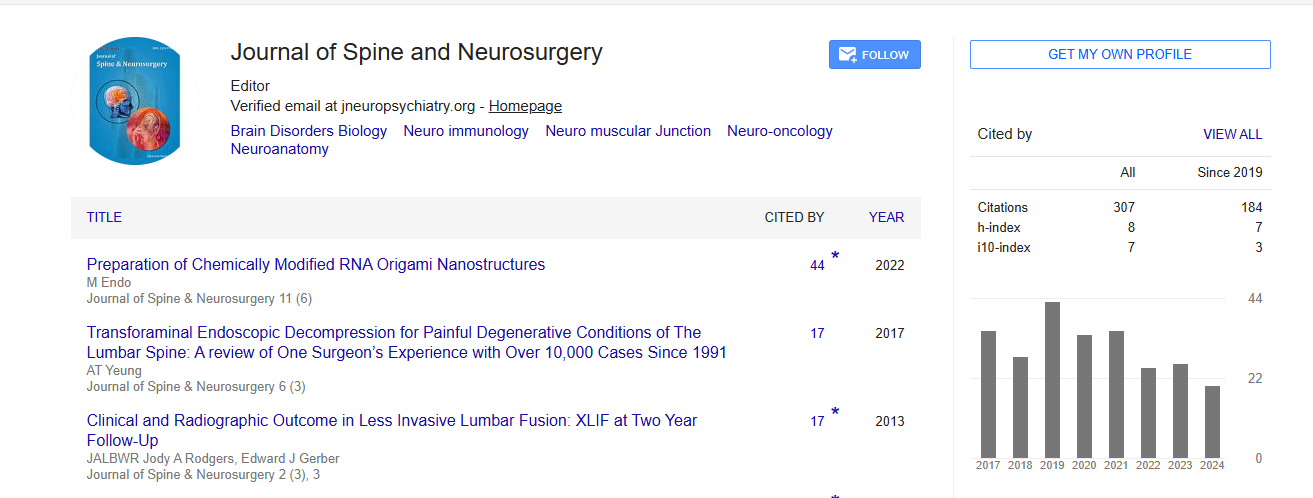
A total of 186 patients were studied. Sixty nine patients who were diagnosed with true recurrent lumbar disc herniation (RLDH group) were chosen as the experimental group compared to 117 operated patients who had no recurrence of lumbar disc herniation (LDH group) as the control group. Fifty-five percent of the patients were male, and 45% were female.
Among all patients, the mean age was 46.4 (SD ± 12.4). Mean age of RLDH and LDH patients was 45.6 ( ± 12.8) and 47.7 (
± 12.8) and 47.7 ( ± 11) respectively. The difference between the two mean values was not significant. Furthermore, the differences of gender, diabetes, morphine addiction, hyperlipidemia and smoking between two groups were not statistically significant (Table 1).
± 11) respectively. The difference between the two mean values was not significant. Furthermore, the differences of gender, diabetes, morphine addiction, hyperlipidemia and smoking between two groups were not statistically significant (Table 1).
| Risk factor | RLDH (N=39) | LDH (N=117) | p-value | |
|---|---|---|---|---|
| Sex | Male | 43.3% | 56.7% | 0.38 |
| Female | 34.3% | 65.8% | 0.08 | |
| Hypertension | 61.5% | 38.5% | 0.00 | |
| Hyperlipidemia | 40.7% | 59.3% | 0.36 | |
| Smoking | 35.6% | 64.4% | 0.80 | |
| Opium addiction | 36.0% | 64.0% | 0.89 | |
| Diabetes | 41.2% | 59.8% | 0.86 | |
Table 1: Frequency of cardiovascular risk factors in patients who underwent lumbar micro discectomy (N=186).
The prevalence of HTN in RLDH and LDH was 61.5% and 38.5% respectively. This difference was significant (P<0.001). The logistic regression analysis showed the recurrence rate was significantly higher in hypertensive patients (OR: 1.74-7.55, CI: 95%, P<0.001) (Table 2). In the hypertensive subgroup, independent confounding variables including medications, diabetes mellitus, family history of cardiovascular disease, hyperlipidemia, duration of symptom-free interval and gender were analyzed (Table 3). The result showed that there was no correlation between these variables and recurrence (P>0.05).
| Risk factors | OR (CI% 95) | Wald | S E | B | p-value |
|---|---|---|---|---|---|
| Gender | 0.59 (0.32-1.08) | 2.88 | 0.31 | -0.52 | 0.09 |
| Age | 1.01 (0.99-1.04) | 27.1 | 0.01 | 0.01 | 0.2 |
| Smoking | 0.91 (0.45-1.84) | 0.06 | 0.35 | -0.08 | 0.8 |
| Addiction | 0.96 (0.48-1.87) | 0.02 | 0.34 | -0.04 | 0.9 |
| Hypertension | 3.63 (1.74-7.55) | 11.82 | 0.37 | 1.28 | 0.001 |
| Hyperlipidemia | 1.31 (0.72-2.39) | 0.81 | 0.31 | 0.27 | 0.3 |
| Diabetes | 0.89 (0.54-1.28) | 1.25 | 0.33 | 0.35 | 0.7 |
Table 2: The effects of covariates on true recurrent lumbar disc herniation.
| Variant | OR (CI%95) | Wald | S.E. | B | p-value |
|---|---|---|---|---|---|
| Gender | 0.19 (0.03-1.19) | 3.11 | 0.91 | -1.61 | 0.07 |
| Diabetes | 1.35 (0.14 - 12.9) | 0.07 | 1.15 | 0.30 | 0.7 |
| Family history | 0.47 (0.08 -2.68) | 0.71 | 0.88 | -0.74 | 0.4 |
| Heart disease | 3.3 (0.31- 34.7) | 1.01 | 1.19 | 1.2 | 0.3 |
| Antihypertensive medications |
0.23 (0.01- 3.94) | 1.03 | 1.45 | 1.5- | 0.2 |
| Hyperlipidemia | 0.73 (0.08 - 6.38) | 0.08 | 1.11 | -0.31 | 0.7 |
| Disease-free interval | 0.48 (0.02- 13.4) | 0.18 | 1.69 | -0.72 | 0.7 |
Table 3: The effects of confounding factors for hypertension on true recurrent lumbar disc herniation.
Discussion
True recurrent disc herniation at the same level and side as the primary one differs from the contralateral herniation at the same level. This type of recurrence is defined as a real or true recurrent disc herniation [6,7]. Studies that focus exclusively on the true recurrence are not high [8-14].
Cardiovascular and atherosclerosis risk factors have shown to be related to disc degeneration and low back pain [15]. The exact mechanism by which atherosclerosis risk factors contribute to disc herniation is not fully understood. Vascular insufficiency and arterial stenosis due to atheroma formation have been noted as underlying mechanisms [2,3,16-19]. The discs have no blood supply and receive nutrients mainly from diffusion. In the presence of atherosclerosis and poor blood supply, the diffusion of nutrients gets affected, and discs degenerate. Whether or not these mechanisms apply to the true recurrence of a disc herniation is unclear.
Reviewing the risk factors for RLDH shows that none of them has been approved. The results of our study also showed that none of the factors of age, sex, diabetes, hyperlipidemia, smoking and morphine addiction predispose a surgically treated disc to true recurrence. Regarding diabetes and smoking, the results of studies are contradictory. Mobbs et al. [20] observed diabetes might be a risk factor for the recurrence, whereas Kim et al. [1] found that there was no relationship between diabetes and disc recurrence. Like our study, Shimia et al. also found the incidence of recurrence was not significantly different between diabetics and non-diabetic patients [8].
Most of the previous studies have failed to demonstrate a clear relationship between obesity and recurrence [21]. Additionally, a possible correlation between hypertension and obesity has been observed [22]. Therefore, obese patients were excluded to eliminate obesity as a confounding variable. We found that the true recurrence rate in patients with history of high blood pressure was significantly higher than those with normal blood pressure. Statistical analysis revealed that the chance of true recurrence is 3.6 times higher in hypertensive patients compared to normotensive patients. Shimia et al. [8] reviewed 40 true recurrent disc herniations to determine the possible risk factors. Regarding HTN, their findings showed that high blood pressure was not related to the recurrence. To the best of our knowledge, no other published article has evaluated the association between true recurrent of lumbar disc herniation and arterial HTN. Since most of the similar studies categorized recurrence and true recurrence in the same group, comparing the results of those studies with our results does not seem to be logical. The remaining question concerns the biologic mechanism linking HTN and disc herniation recurrence. Hypertension, as a systemic disease, may affect the surgically treated discs per se. It should affect the entire spine, but we have no data on the association between the HTN and the cervical or thoracic discs. Hypertension, as noted before, may influence treated discs as results of vascular insufficiency. It is also possible that an undetermined factor affects both the blood pressure and the treated discs simultaneously and independently. In this case, we are faced with two separate end-results rather than two dependent variables. Additional studies should examine the specificity and pathogenicity of HTN on treated discs and screen for structural and molecular changes.
Although this study was carefully conducted, we are still aware of its limitations. A prospective randomized controlled study would have been better to establish the correlation between HTN and the recurrence, which is still not established by any level 1 or level 2 studies in the literature. The sample is too small to state a definitive conclusion; for this reason the interpretation of the P value/95% confidence interval was focused on its relativeness and the possible effects. Mechanical factors including heavy lifting and work-status as well as sports activities have not considered in this study. Regarding HTN, we were faced treated patients. All hypertensive patients were placed on antihypertensive medications; therefore we were not able to investigate the net effect of high blood pressure on recurrence. Another limitation was that we did not know the duration of HTN because it is often asymptomatic, so the length of HTN was ignored. There is also no documentation of the amount of disc removed in the first surgery to establish whether the amount of disc removed were statistically significant or not in the two groups, as there might be that the remaining disc in RLDH group would be higher than the control group to cause recurrence again.
In conclusion, the present study found that among some known cardiovascular and atherosclerosis risk factors, HTN might have a role in the true recurrence of surgically treated lumbar disc herniation, however, the causal relationship between hypertension and the recurrence requires further research. Hypertensive patients had a significantly increased risk of recurrence; therefore, concern for recurrent disc herniation should be increased during outpatient follow-up. The results of this study are intriguing and open the door to an appealing research line with important practical consequences as it could lead to the reduction in the recurrence rate after herniated disc surgery.
References
- Kim MS, Park KW, Hwang C, Lee YK, Koo KH, et al. (2009) Recurrence rate of lumbar disc herniation after open discectomy in active young men. Spine 34: 24-29.
- Jhawar BS, Fuchs CS, Colditz GA, Stampfer MJ (2006) Cardiovascular risk factors for physician-diagnosed lumbar disc herniation. Spine J 6: 684-691.
- Kauppila LI (2009) Atherosclerosis and disc degeneration/low-back pain–a systematic review. Eur J Vasc Endovasc 37: 661-670.
- Reihani-Kermani H, Afshar RM, Nakhaee N (2006) Effect of morphine dependency on intervertebral disc in rat. Iran J Med Sci31: 147-150.
- Asgary S, Barkhordari HR, Hojjat H, Naderi GA, Dashti GR (2010) Does morphine use increase risk of atherosclerosis in animals on normal or high-cholesterol diet?. ARYA Atheroscler 3: 131-134.
- Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, et al. (2012) Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Ortho Sci 17: 107-113.
- Cinotti G, Gumina S, Giannicola G, Postacchini F (1999) Contralateral recurrent lumbar disc herniation. Results of discectomy compared with those in primary herniation. Spine 24: 800-806.
- Shimia M, Babaei-Ghazani A, Sadat BE, Habibi B, Habibzadeh A (2013) Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg 8: 93-96.
- O’Sullivan MG, Connolly AE, Buckley TF (1990) Recurrent lumbar disc protrusion. Br J Neurosurg 4: 319-325.
- Connolly ES (1992) Surgery for recurrent lumbar disc herniation. Clin Neurosurg39: 211-216.
- Dai L-Y, Zhou Q, Yao W-F, Shen L (2005) Recurrent lumbar disc herniation after discectomy: outcome of repeat discectomy. Surg Neurol 64: 226-231.
- Haglund MM, Moore AJ, Marsh H, Uttley D (1995) Outcome after repeat lumbar microdiscectomy. Br J Neurosurg 9: 487-495.
- Hirabayashi S, Kumano K, Ogawa Y, Aota Y, Maehiro S (1993) Microdiscectomy and second operation for lumbar disc herniation. Spine 18: 2206-2211.
- Swartz KR, Trost GR (2003) Recurrent lumbar disc herniation. Neurosurg Focus15: 1-4.
- Kauppila LI (1997) Prevalence of stenotic changes in arteries supplying the lumbar spine. A postmortem angiographic study on 140 subjects. Ann Rheum Dis56: 591-595.
- Shakeri A, Shakeri M, Behrooz MO, Behzadmehr R, Ostadi Z, et al. (2017) Infrarenal aortic diameter, aortoiliac bifurcation level and lumbar disc degenerative changes: a cross-sectional MR study. Euro Spine J 2017: 1-9.
- Kauppila LI (1994) Blood supply of the lower thoracic and lumbosacral regions. Postmortem aortography in 38 young adults. Acta Radiol 35: 541-544.
- Kauppila LI (1995) Ingrowth of blood vessels in disc degeneration. Angiographic and histological studies of cadaveric spines. J Bone Joint Surg Am 77: 26-31.
- Kauppila LI, McAlindon T, Evans S, Wilson PW, Kiel D, et al. (1997) Disc Degeneration/Back Pain and Calcification of the Abdominal Aorta: A 25-Year Follow-Up Study in Framingham. Spine 22: 1642-1647.
- Mobbs RJ, Newcombe RL, Chandran KN (2001) Lumbar discectomy and the diabetic patient: incidence and outcome. J Clin Neurosci 8: 10-13.
- Quah C, Syme G, Swamy GN, Nanjayan S, Fowler A, et al. (2014) Obesity and recurrent intervertebral disc prolapse after lumbar microdiscectomy. Ann Roy Coll Surg 96: 140-143.
- DeMarco VG, Aroor AR, Sowers JR (2014) The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol 2014 10: 364-376.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi