Research Article, J Food Nutr Disor Vol: 12 Issue: 1
Treatment Outcomes and Barriers for Outpatient Management of Acute Malnutrition among 6-59 Months Children in Eastern Ethiopia: Mixed Study Design 2022
Tariku Derese*, Mikiyas Solomon and Bereket Tefera
Department of Public Health, Lecturer at Dire Dawa University, Dire Dawa, Ethiopia
- *Corresponding Author:
- Tariku Derese
Department of Public Health,
Lecturer at Dire Dawa University,
Dire Dawa,
Ethiopia;
Email: t.derese@yahoo.co.uk
Received date: 16 September, 2022, Manuscript No. JFND-22-74872; Editor assigned date: 19 September, 2022, PreQC No. JFND-22-74872 (PQ); Reviewed date: 03 October, 2022, QC No. JFND-22-74872; Revised date: 09 January, 2023, Manuscript No. JFND-22-74872 (R); Published date: 23 January, 2023, DOI: 10.4172/2324-9323.1000336.
Citation: Derese T, Solomon M, Tefera B (2023) Treatment Outcomes and Barriers for Outpatient Management of Acute Malnutrition among 6-59 Months Children in Eastern Ethiopia: Mixed Study Design 2023. J Food Nutr Disor 12:1.
Abstract
Background: In Ethiopia children suffering from acute malnutrition are at significantly higher risk of morbidity and mortality. Most of the studies indicated that the treatment outcome of severe acute malnutrition is below the sphere standard. Different enablers and barriers influence treatment outcomes of children in outpatient therapeutics centers. This study is designed to describe treatment outcome and the main barriers hinder the treatment outcomes.
Methods: A mixed study design was implemented from January 20/2022-July 1/2022 and a total sample was 183. All cases from selected health facilities involved in the study and health professional trained on malnutrition were followed each case for 8 weeks. To explore facilitators and barriers of treatment outcomes in-depth interview of 14 key in formant was implemented. Quantitative data were collected by Kobo tool and the qualitative data were collected by tape recorder. Data were export to SPSS version 21 quantitative analysis and Nvivo 11 was used for qualitative data analysis. Outcome indicators were presented by tables and text. The qualitative data was presented with thematic area of the main findings.
Results: This finding revealed that 147 (81.2%) with (SD: 0.57 95% CI, (75.1-87.3)), 22 (12.2%) with (SD: 0.57 95% CI (6.6-17.4)) and 12 (6.6%) with (SD: 0.57 95% CI (3.1-10.7)) were cure, defaulter and non-recovery rates respectively. The average length of stay were 39 days and Mean weight gain was 1.36 g/kg/day. Discussants had identified: Collaboration, providers activity, structural factors, referral and communications and monitoring and reporting were a facilitators. Furthermore, sub-themes community perception, defaulting, family wealth, food sharing, maternal education and awareness, supplies, RUTF selling, training opportunities and professional burn-out identifies as barrier factors.
Conclusion: The results of treatment outcomes of severe acute malnutrition in outpatient centers were in acceptable range compared to sphere project reference values. Discussants identified that “community perception, defaulting, family wealth, food sharing, maternal education and awareness, supplies, RUTF selling, training opportunities and professional burn-out” as main barriers for treatment outcomes. Developing appropriate intervention and mass communication strategies on identified barriers for better treatment outcome is important.
Keywords: Treatment outcomes; Severe acute malnutrition; Outpatient; Facilitators; Barriers; East Ethiopia
Abbreviations:
CI: Confidence Interval; CMAM: Community Management of Acute Malnutrition; HC: Health Center; HEW: Health Extension Worker; IDI: In-Depth Interview; MAM: Moderate Acute Malnutrition; MUAC: Middle Upper Arm Circumference; OPD: Out-Patient Department; OTP: Out-Patient Treatment Program; RUTF: Ready-to-Use Therapeutic Food; SAM: Severe Acute Malnutrition; SD: Standard Deviation; SPSS: Social Package for Statistical Software; UNICEF: United Nation International Child Emergency Fund; WFH: Weight For Height; WHO: World Health Organization.
Introduction
Out-patient management program for severe acute malnutrition without complications is the components of CMAM (Community Management Acute Malnutrition) [1]. The OTP (Out-Patient Program) offers service to severely malnourished children age 6–59 months. Children enrollment for OTP according to the WHO Protocol for Severe Acute Malnutrition (SAM) management is mid-upper arm circumference of less than 110 mm or WFH of less than 70%. Children who passed appetite test with plumpy’ nut, with no edematous and children without medical complications are eligible for the outpatient therapeutics program [2].
Even though the burden is high, currently very few countries incorporation of Severe Acute Malnutrition (SAM) management into regular government budget programming. United Nation International Child Emergency Fund (UNICEF) evaluations show that a portion of investments and recurring costs are being met domestically in Chad, Ethiopia, Kenya, Nepal and Pakistan [3,4].
A meta-analysis data from 19 studies indicated that the pooled recovery rate is below the sphere standard of 75% and is clearly affected by the non-recovery and defaulter rates. Evidence revealed that recovery rate ranges 32.7% to 92.7%. Key issues noted with recovery rate were ready-to-use therapeutics food sharing at home, lack of supportive medication for treatment and distance of child residence from outpatient therapeutics centers are hampering treatment adherence [5].
Over the past ten years, there have been numerous attempts to scale up severe wasting treatment with the ultimate goal of establishing national and international coverage of a reliable, high-quality service delivered as a crucial component of the healthcare system and backed by a solid community basis.
However, the analysis revealed that a variety of possible facilitators and constraints were found to be impacting the expansion of the OTP program. The World Health Organization (WHO) health system strengthening framework categorized the treatment barriers under six pillars. Health system, health personnel, logistic supplies, health information systems, leadership and financing [6]. Moreover, the quality and effectiveness of outpatient program depends on: An enabling policy environment; sustained financing a competent and responsive workforce; consistent stock of equipment; timely availability of supplies; supportive environment in which quality services are delivered and information management systems to monitor implementation are important are very important barriers for out-patient treatment outcomes [7,8].
Ethiopia national level quality health care strategies (2016-2020) included that the reduction of child mortality and morbidity through effective prevention and management of severe wasting is pointed as a key priority [9,10]. Focusing on household food security and scaling up nutrition programs have a made tremendous contribution to reducing under nutrition. However, millions of Ethiopians children still suffer from acute malnutrition and related problems. The country ranks at the top both in Sub-Saharan Africa and the world for malnutrition [11,12].
The health extension program of Ethiopia included Essential Nutrition Action (ENA) as nutritional packages and although the program has been effectively in increasing service coverage, it suffers from gaps in terms of resources, service integration and access, limited supervision from higher official, training and poor referral to higher levels of care [13].
To enable meaningful engagement from community-led and nongovernmental organization in decision making at all levels to demand support and ensure delivery of outpatient program in a manner that is responsive, inclusive, and participatory and representative is important. To this end qualitative and quantitative evidence is crucial to accelerate the success. However, there is data gap on the treatment outcomes of OTP (Out-Patient Program), and barriers contributing for poor treatment outcome of uncomplicated severe acute malnutrition management program. Therefore, this study was aims to describe the treatment outcomes and explore barriers for out-patient acute malnutrition management among 6-59 months children in eastern Ethiopia: Mixed study, 2021/22.
Materials and Methods
Study area and study period
The study was carried out in selected health facilities of eastern Ethiopia. Dire dawa town administration has a total urban population of 297,361 people and 26,594 were children among the age group of 6-59 months. Dire dawa town administration has 8 health centers and all provide OTP service for children. Haramaya district is found in east Harergie zone, Oromia regional state. Haramaya has a total population of 332,574 and children <5 years of the district is 54,645. Erer is located in Somalia regional state and 70 km from Dire Dawa. Erer has one health center which provides OTP service for children. A total of 25,367 populations live in Erer town. The total number of children living in Erer selected health center catchment is 10867 [14]. Follow up data was collected from January 20/2022 to July 1/2022.
Study design
A mixed study design was implemented. For quantitative data prospective cohort study design was implemented to assess the treatment outcomes of outpatient management of acute malnutrition among 6-59 months children. All children enrolled since January 20/2022 in each outpatient treatment centers and followed for eight weeks. To explore the facilitators and barriers for community based management of acute malnutrition among 6-59 months children key informant in depth interview were conducted.
Source and study population
All among 6-59 months old children enrolled in outpatient management of acute malnutrition program during the study period for follow up in Dire Dawa, Haramaya and Erer health facilities were considered as the source of population. All children enrolled in outpatient program in selected health facilities since January 20/2020 was the study population. For qualitative data the participants were selected purposively based on the assumption that they have more prior knowledge/information on community based management of acute malnutrition (OTP) program from all centers (health extension supervisors, health professional working under five OPD, health facility managers and health extension workers) were participated.
Inclusion and exclusion criteria
All among 6-59 months children enrolled in to out-patient therapeutic program since January 20/2022 and follow their follow up at out-patient program for uncomplicated severe acute malnutrition in each selected treatment centers were included in the study. All among 6-59 months children those followed their follow up for other medical cases were excluded.
Sample size determination
The sample size was determined using single population proportion formula and the proportion was taken from previous study in Ethiopia. According to previous study conducted in Ethiopia, defaulter rate=13.8%, was taken by considering 95% Confidence Interval (CI) and 5% marginal error and calculated as follows; level of significance to be 5% (α=0.05), Zα/2=1.96 and absolute precision or margin of error to be 5% (d=0.05) [15].
Where n=sample size,
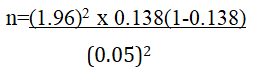
The total sample size of this study is 183
For qualitative data: A total of 14 in-depth interviews were conducted in all selected health facilities until the idea was saturated.
Sampling procedure and technique
By reviewing the last one year total treatment outcomes of outpatient management of acute malnutrition case load of each health facilities and feasibility: Haramaya, Dire Dawa and Erer were selected. The three health facilities were selected from Dire Dawa, two health facilities were selected from Haramaya and Erer by simple random sampling technique. Finally, based on the last year’s total case load, proportionally 122 cases were taken from dire dawa, 44 cases from haramaya and 17 from Erer followed for eight weeks. For qualitative data; our key informant in-depth interview were from five community based management acute malnutrition facilities (health extension coordinators, health professional working under five OPD and health extension workers) were participated in our in-depth interview.
Operational definitions
Outpatient program/OTP: Involved from community based therapeutic program, a community-based approach for the management of acute malnutrition 2001 [16].
Barriers: Are those factors at least one hindrance existed (indirect cost of care, opportunity costs, lack of availability of services, lack of culturally competent care/acceptability of care) which could be the respondents wanted to see health professionals but not and/or respondents not seeking and utilizing health care services totally for community based management of acute malnutrition care [17].
Uncomplicated severe acute malnutrition: Is defined by a weight for height index <-3 z-score, MUAC <11.5 cm and/or without medical complication [18].
Recovery rate: Number of children graduate or successfully complete children their treatment follow up for 2 months divided by the total number of children enrolled for OTP follows up in all selected facilities [19].
Defaulter rate: Number of children defaulted from their treatment follow up within 2 months divided by the total number of children enrolled for OTP follow up in 2021 in all selected facilities. Two consecutive absence from OTP follow up considered as defaulters.
Mean rate weight gain: Is the difference in weight gain, discharge to admission, multiplying the result by 1000, and then divided by number of days stayed in the treatment.
The average length of stay/mean: The sum of a number of days that the child stays in the outpatient therapeutic feeding program per total number of patients in a program.
Non-recovery: Patient that did not reach the discharge criteria after 2 months or 8 weeks in the OTP follow up.
Wealth index: "Possessions owned by a household are based on asset based wealth indices. The index was built using household asset data using "Principal Component Analysis" (PCA) [20].
Data quality control
Data quality was maintained by recruiting data collectors trained on outpatient management program and supervisors were provided with intensive training. Questionnaire was pre-tested and compared with community-based management acute malnutrition logbook and all variables were included. Two days training for quantitative and qualitative data collectors were provided about interviewing technique, probing, communication skill and techniques about filling of the questionnaire. Weight and height measurement was demonstrated by data collectors after training. Quantitative data were collected using structured questionnaire developed from previous studies [21-23]. Admission and follow-up weight were measured by UNICEF self-zeroing digital weight measuring tool and height measuring board were checked the accurate to 0.5 cm tool which is denoted by UNICEF. Measurements tool were calibrated between each measurement using a 1 kg weight and adjusted to zero. At each visit all information including child outcome (cure, default, transfer or nonrecovery) had been recorded on KOBO tool. The maximum follow up period for the children on OTP was 8 weeks based on national guideline. During data collection, completeness, consistency and discrepancies of the data were managed by investigators. Data clearance, range and logic checks carry out regularly to ensure the quality of data before data entry. Any incomplete data and inconsistent data were excluded from the data. A total of 8 data collectors were recruited to collect follow up data from each out-patient therapeutic centers. All in-depth interviews were recorded by sonny tape recorder by local language and the audio translated to verbatim. Translation of key informant interview data verbatim response to English was performed. The transcribed english language in-depth interview were categorized and coded in to case before exporting in to Nvivo 11.
Data processing and analysis
Quantitative data were collected by KOBO tools; exported to excel and data clearance performed, and analyzed by SPSS Version 21. The treatment outcomes were described as: recovery, default, and nonrecovery rates. Weight gain and recovery time were calculated based on national protocol. Cross tabulation, and frequency tables were used to report the descriptive data.
Qualitative data analysis was conducted using Nvivo 11. Fourteen 14 in-depth interviews coded separately as a case and exported to Nvivo 11. Then, under the main two themes, facilitating and barrier factors, we have identified 12 sub themes, where 5 are categorized under the facilitating factors, 6 subthemes were identified under the barrier factors and an additional one floating theme was identified. Finally, the summary was presented with text.
Results
Mothers/care givers socio-demographic characteristics
A total of 183 cases were enrolled to the cohort. During data clearance two data were excluded from the analysis since they have incomplete follow up history. A total of 181 cases were analyzed, and 147 cases were cured and 34 cases were censored. Most of the child mothers or caregivers aged were 86 (47.5%) between 25 and 29 years with (SD: 0.90 95% CI (41.2-54.7)), and 69 (38.1%) child mothers or care givers were married before the age of 18 years. Among child mother/care givers, 118 (65.2%) did not have formal education and 11.6% families registered for General Food Ratio (GFD). However, 8 (45.3%) of the child care givers have not received any nutritional counseling about plumpy nut or RUTF during their facility visit. Regarding the wealth index, 42 (23.2%) with (SD: 3.3 95% CI (22.7-28.1)) households were in the poorest wealth index and 54 (29.8%) with (SD: 3.1 95% CI (16-36.5)) richest wealth index Table 1.
| Variables | Cured No (%) | Defaulter No (%) | Non-recovery No (%) | Overall | |
|---|---|---|---|---|---|
| Age of the child mothers or caregivers | 15-19 | 3 (2%) | 3 (1.7%) | ||
| 20-24 | 40 (27.2%) | 7 (31.8%) | 3 (25%) | 50 (27.6%) | |
| 25-29 | 66 (44.9%) | 12 (54.5%) | 8 (66.7%) | 86 (47.5%) | |
| 30-34 | 29 (19.7) | 3 (13.6%) | 1 (8.3%) | 33 (18.2) | |
| ≥ 35 | 9 (6.2%) | 9 (5%) | |||
| Maternal age at 1st marriage | <18 Years | 61 (41.5%) | 6 (27.3%) | 2 (16.7%) | 69 (38.1%) |
| ≥ 18 years | 86 (58.5%) | 16(72.7%) | 10(83.3%) | 112(61.9%) | |
| Child mother/care giver marital status | Married | 130 (88.4%) | 18 (81.8%) | 10 (83.3%) | 158 (87.3%) |
| Single | 10 (6.8%) | 3 (13.6%) | 13 (7.2%) | ||
| Divorced/widowed | 7 (4.8%) | 1 (4.6%) | 2 (16.7%) | 10 (5.5%) | |
| Child mother/care giver educational Status | No formal education | 98 (66.7%) | 13 (59%) | 7 (58.3%) | 118 (65.2%) |
| Primary | 46 (31.3%) | 9 (41%) | 3 (25%) | 58 (32%) | |
| Secondary | 3 (2%) | 2 (16.7%) | 5 (2.8%) | ||
| Household family size | <4 Families | 101 (68.7%) | 19 (86.4%) | 12 (100%) | 132 (72.9%) |
| ≥ 4 Families | 46 (31.3%) | 3 (13.6%) | 49 (27.1%) | ||
| Travel time from residence to health facility | <1 hrs | 136 (92.5%) | 4 (18.8%) | 1 (8.3%) | 141 (77.9%) |
| ≥ 1 hrs | 11 (7.5%) | 18 (81.2%) | 11 (91.7%) | 40 (22.1%) | |
| Family registered for General Food Ratio (GFD) | No | 131 (89.1%) | 20(90.9%) | 9 (75%) | 160 (88.4%) |
| Yes | 16 (10.9%) | 2 (9.1%) | 3 (25%) | 21 (11.6%) | |
| Plumpy-nut selling a common practice in your area | No | 106 (72.1%) | 17 (77.3%) | 9 (75%) | 132 (72.9%) |
| Yes | 41 (27.9%) | 5 (22.7%) | 3 (25%) | 49 (27.1%) | |
| Received any nutritional counseling about plumpy-nut or RUTF | No | 52 (35.4%) | 20 (90.9%) | 10 (83.3%) | 82 (45.3%) |
| Yes | 95(64.6%) | 2 (9.1%) | 2 (16.7%) | 99 (54.7%) | |
| Household wealth index | Richest wealth index | 51 (34.7%) | 3 (13.6%) | 0 (58.3%) | 54 (29.8%) |
| Medium wealth index | 63 (42.9%) | 14 (63.6%) | 8 (66.7% | 85 (47%) | |
Poorest wealth index |
33 (22.4%) |
5 (22.7%) |
4 (33.3%) |
42 (23.2%) |
|
Table 1: Socio-demographic characteristics of mothers/care givers in out-patient therapeutic feeding program/OTP centers in eastern Ethiopia, 2022 (n=181)
Clinical history of the child at admission
Among children affect by severe acute malnutrition, 122 (67.4%) were under the age of two years. Diarrhea at admission were 51 (28.2%) and 132 (72.9%) were breast feeding children. Among a total, 176 (97.2%) were newly admitted for OTP and 76 (42%) were admission criteria were MUAC (Table 2).
| Variables | Cured No (%) | Defaulted No (%) | Non-recovery No (%) | Overall No (%) | |
|---|---|---|---|---|---|
| Child age (in months) | 6-11 | 43 (29.3%) | 7 (31.8%) | 6 (50%) | 56 (30.9%) |
| 12-23 | 55 (37.4%) | 8 (36.4%) | 3 (25%) | 66 (36.5%) | |
| 24-35 | 33 (22.4%) | 6 (27.3%) | 2 (16.7%) | 41 (22.7%) | |
| 36-47 | 14 (9.5%) | 1 (4.5%) | 1 (8.3%) | 16 (8.8%) | |
| 48-59 | 2 (1.4%)) | 2 (1.1%) | |||
| Child gender | Female | 65 (44.2%) | 10 (83.3%) | 7 (58.3%) | 82 (45.3%) |
| Male | 82 (55.8%) | 12 (54.5%) | 5 (41.7%) | 99(54.7%) | |
| Admission criteria | Edema | 21 (14.3%) | 5 (22.7%) | 3 (25%) | 29 (16%) |
| MUAC and Z-score | 44 (29.3%) | 9 (40.9%) | 4 (33.3%) | 57 (31.5%) | |
| MUAC | 64 (43.5%) | 7 (31.8%) | 5 (41.7%) | 76 (42%) | |
| Z-Score | 18 (12.2%) | 1 (4.5%) | 19 (10.5%) | ||
| Type of admission | New | 143 (97.3%) | 22 (100%) | 11 (91.7%) | 176 (97.2%) |
| Repeat | 4 (2.7%) | 1 (8.3%) | 5 (2.8%) | ||
| Type of supplemented food | Plumpy-SUM | 7 (4.8%) | 4 (33.3%) | 11 (6.1%) | |
| RUTF | 140 (95.2%) | 22 (100%) | 8 (66.7%) | 170 (93.9%) | |
| Diarrhea at admission | No | 108 (73.5%) | 17 (77.3%) | 5 (41.7%) | 130 (71.8%) |
| Yes | 39 (26.5%) | 5 (22.7%) | 7(58.3%) | 51 (28.2%) | |
| Cough and difficulty to breath at admission | No | 120 (81.6%) | 20 (90.9%) | 11 (91.6%) | 151 (83.4%) |
| Yes | 27(18.4%) | 2 (9.1%) | 1 (8.3%) | 30 (16.6%) | |
| Fever at admission | No | 129 (87.7%) | 18 (81.8%) | 8 (66.7%) | 156 (86.2%) |
| Yes | 18 (12.2%) | 4 (18.2%) | 4 (33.3%) | 25 (13.8%) | |
| Breast feeding status of the child | Still breast feeding | 104 (70.7%) | 17 (77.3%) | 11 (91.6%) | 132 (72.9%) |
| Stopped breast Feeding | 43 (29.3%) | 5 (22.7%) | 1 (8.3%) | 49 (27.1%) | |
Table 2: Clinical history of 6-59 month children at admission of outpatient therapeutic feeding program/OTP centers in eastern Ethiopia, 2022 (n=181)
Treatment outcomes of OTP program
Out of 181 enrolled children in outpatient therapeutic feeding program in Eastern Ethiopia, 147 (81.2%) with (SD: 0.57 95% CI, (75.1-87.3)) were cured, 22 (12.2%) with (SD: 0.57 95% CI (6.6-17.4)) were defaulter and 12 (6.6%) with (SD: 0.57 95% CI (3.1-10.7)) were non-recovered. Average length of stay were 39 days with (SD 13.47: 95% CI (12.61-14.18) and mean weight gain were 1.36 g/Kg/day with (SD: 0.48 95% CI (0.48-0.5)). Treatment outcome of severe acute malnutrition in therapeutics centers of this study were in acceptable range compared to the sphere project reference values. However, the mean weight gain in the outpatient treatment center was not in acceptable range compared to sphere standard (Table 3).
| Treatment outcome indicators (OTP) | Frequency (n=181) | (%) | Sphere standard acceptable | Alarming |
|---|---|---|---|---|
| Cure rate | 147 | 81.20% | >70% | <50% |
| Defaulter arte | 22 | 12.20% | <15% | >30% |
| Non-recovered rate | 12 | 6.60% | <10% | >> |
| The mean length of stay (in OTP centers) | 39 days | 5.6 weeks | <8 weeks | >8 weeks |
| Mean weight gain | 1.36 g per Kg/day | 3 g/Kg/day | <3 g/kg/day |
Table 3: Performance indicator of treatment outcomes of severe acute malnourished among 6-59 month children in OTP centers in eastern Ethiopia as compared to sphere project reference values/standard, 2022.
Qualitative result
Barriers and facilitators severe acute malnutrition treatment/ OTP: We have conducted qualitative study to explore barriers and facilitators of OTP (Outpatient Therapeutic Program), using an open ended interview guide. Data were collected from health professionals directly involved in out-patient therapeutic centers. Transcription, translations and back translation were done by different practitioners familiar with language under the discussion. A total of 14 key informants who were health extension workers, nurses, health officers and medical doctors, and directly involved in the screening and treatment of malnourished children (Table 4).
| IDI_ID | Name of facility | Gender | Age | Profession | Position | Experiencing years |
|---|---|---|---|---|---|---|
| IDI_1 | Melka Jebdu HC | Male | 35 | Health education | Health extension coordinator | 7 |
| IDI_2 | Melka Jebdu HC | Female | 33 | Diploma nurse | Health extension worker | 12 |
| IDI_3 | Melka Jebdu HC | Female | 36 | Diploma nurse | // | 5 |
| IDI_4 | Melka Jebdu HC | Male | 31 | BSC nurse | Nutrition focal | 3.5 |
| IDI_5 | Addis Ketema HC | Female | 37 | Diploma nurse | Health extension worker | 5 |
| IDI_6 | Addis Ketema HC | Male | 29 | BSC nurse | Health extension coordinator | 7 |
| IDI_7 | Addis Ketema HC | Male | 38 | BSC nurse | OTP focal | 7 |
| IDI_8 | Legehare HC | Female | 39 | Diploma nurse | Health extension worker | 10 |
| IDI_9 | Legehare HC | Female | 35 | BSC nurse | Health extension coordinator | 15 |
| IDI_10 | Gende Gerada HC | Male | 30 | Environmental health | // | 6 |
| IDI_11 | Gende Gerada HC | Female | 33 | Diploma nurse | Health extension worker | 11 |
| IDI_12 | Gende Gerada HC | Female | 34 | BSC nurse | OTP focal | 12 |
| IDI_13 | Erer HC | Male | 28 | Health officer | OTP focal | 4 |
| IDI_14 | Erer HC | Male | 29 | Doctor | U5 OPD | 2 |
Table 4: Attributes of qualitative study participants in outpatient therapeutic feeding program centers in eastern Ethiopia, 2022 (n=14).
Analysis was done using NVivo 11. Under the main two themes, facilitating and barrier factors, we have identified 12 sub themes, where 5 are identified under the facilitating factors, 6 sub themes were identified under the barrier factors and an additional one floating theme was identified. Under the facilitating factors we have identified themes: Such as collaboration, providers activity, structural factors, referral and communications, and monitoring and reporting. Furthermore, we have identified sub themes: Such as community perception, defaulting, family wealth, food sharing, maternal education and awareness, supplies, RUTF/Plumpy-Nut selling, training opportunities and professional burn-out under barrier factors. Provider forward was identified as floating theme.
Facilitating factors
Collaboration: Under collaboration sub theme, participants had identified working with; “community figures”, “family health team leaders”, “women development army”, “regional health bureau, kebele leaders”, and “presence of non-governmental organizations working on management of child malnutrition” (IDI_4, IDI_9, IDI_10, and IDI_13) confirmed as the main facilitators.
Providers activity: Most of the participants understood and “dedicated for” their activity, and identified out-patient program was health extension worker activities as their “main duty”. “Regular home visit” is their main activity with “children nutritional screening using MUAC, providing vitamin A and deworming, referral of malnourished children to health center and OTP centers, consultation to mothers and care givers on child feeding and nutritional education, personal and environmental hygiene”. However, “presence of overlapping campaign activities” and “family folder updating had highly impacted” their routine service, have missed children with possible signs of nutritional disorders (IDI_1, IDI_5, IDI_6, IDI_7, IDI_8, IDI_9, IDI_10, IDI_11, IDI_12, and IDI_13).
Structural factors: Interviewees were identified structural issues, where the main point of concern were implementation activities, presence of OTP and stabilization centers in health centers, presence of early detection systems, adequate availability of assessment tool (anthropometrics measurement assessment tools), NGO’s support and motivation was highly valued, focused screening activity for a catchment presented with many under nourished children, working with facility staffs and community agents increases service acceptability, benefited from regular nutritional screening to detect children with MAM (Moderate Acute Malnutrition), freely available service to all MAM and SAM management, mothers who are enrolled to CBHI (Community Based Health Insurance) are committed to follow their routine appointments, nutritional counseling service given to mothers who have under nourished children, availability of different guidelines in the facility; health extension program packages, Management of SAM and MAM, though there exist understanding gap among health extension workers (IDI_1, IDI_2, IDI_3, IDI_4, IDI_5, IDI_6, IDI_7, IDI_9, IDI_10, IDI_11, IDI_12, IDI_13, and IDI_14).
Referral and communication: Under referral and communications sub theme health extension workers discussed that there is a functional referral system and any child screened using MUAC and confirmed for having severe acute malnutrition will be referred to OTP centers. Children with complications will be referred to OTP centers and focal persons manage the children and follow their progress based on the guideline. Interviewee had discussed that there was an increasing trend of self-referral, where mothers brought their children with feeding and weight complaints (IDI_4, IDI_6, IDI_7, IDI_8, IDI_9, IDI_11, IDI_12, IDI_13, and IDI_14).
Monitoring and reporting: Health extension workers mentioned that they are not responsible to monitor the child’s health condition after referral, while they receive feedback from OTP focal person working at the facility. This feedback mechanism enables them to track children status. The interviewees believe that regular screening activity and supportive supervision can help strengthen early detection of children with nutritional disorders and reduce related complications. They indicated that, timely reporting and supervision also helps in maintaining logistic supplies (IDI_1, IDI_2, IDI_3, IDI_4, IDI_7, IDI_8, IDI_9, and IDI_11).
Barrier factors
Community perception: We understood that there is a diverse understanding and perception towards under nutrition and its management, where it is evidenced by mother’s diverse level of understanding about nutritional disorders, health care seeking behaviors, management preference, indications and use of RUTF/ Plumpy-Nut, and consequences of under nutrition.
Most mothers know that under nutrition is a series condition and it can complicate their child to other diseases. Most of mothers did have poor health care seeking behavior, referred mothers usually visit health facility very late. They initially prefer traditional remedies and discuss with neighbors if they suspect their child has nutritional disorders; they will come to facilities if they are not satisfied with the traditional management progress and the child shows worsening. Because, Plumpy-Nut is widely available in the local shops, mothers believe that it is a kind of food; they don’t consider that it is a therapeutic diet, and they usually share it with older siblings. Mothers who had normal children also visit facilities for RUTF/Plumpy-Nut.
Furthermore, mothers perceive that the source of fever during OTP management is the RUTF/ plumpy-nut, and they usually refuse to continue the management. They consider their child is totally cured if the child shows moderate weight improvement and they default from the program (IDI_3, IDI_4, IDI_5, IDI_6, IDI_7, IDI_8, IDI_9, IDI_10, IDI_11, and IDI_13).
Supply: Interviewees had different opinion regarding supply of RUTF/plumpy-nut and other necessary facilities. Some had indicated there were RUTF/Plumpy-Nut shortages at facility level and sometimes store keepers were not available around and mothers might not receive their RUTF/Plumpy-Nut. In addition folic acid and amoxicillin stock outs were the common problems discussed. These events had let mothers to default in their next visit and affected children treatment progress. Absence of weighing and height measurement facilities in the field visit lets health extension workers over classifies MAM cases, where children may not be eligible to OTP when checked with weight for age or weight for height (IDI_4, IDI_8, IDI_9, and IDI_14).
Defaulting: We have tried to explore why mothers default from OTP after they have properly engaged to the program and found various explanations. As most mothers are from low economic population segment, they live in a rented house and usually move to another place in search of low cost houses, and most mothers are daily labors and they usually change their living area looking for jobs, where they have no permanent living address. Some mothers come from distant villages and returning back is difficult due to transportation and expense issues. Others come from Djibouti and local cities during hot seasons and back to home during the colder season, others are traders and move to local cities and djibouti, and health professionals at facility might have incomplete address to follow-up, poor communication of OTP providers, mothers work load, mothers poor awareness about the consequences of malnutrition, mothers belief that minor improvements mean total cure, mothers perception that RUTF/Plumpy-Nut worsen children temperature, Some mothers may start treatment without the referral system and failed to capture their full detail, and shortage of supplies usually let others default their appointment (IDI_2, IDI_3, IDI_4, IDI_6, IDI_7, IDI_8, IDI_9, IDI_10, IDI_11, IDI_12, and IDI_13).
RUTF/Plumpy-Nut sharing and sell: We understood that RUTF/ Plumpy-Nut sharing to siblings are a common practice. Mothers share the RUTF/ Plumpy-Nut because they may not have enough food to feed for their children, when they want to silent a disturbing child, when they are busy an older child will take care of the younger one and they will share the RUTF/ Plumpy-Nut, and mothers believe that RUTF or Plumpy-Nut is a type of food and can be shared with others. Interviewees have been hearing that mothers sell the RUTF/ plumpy- Nut to local shops, and they have confirmed that they found the same batch of RUTF/Plumpy-Nut at the market. Whenever a mother is provided a RUTF/Plumpy-Nut, the product batch is registered and the mothers will be asked to bring the used sachets when they came for refill. However some mothers sell some of it and come to facility with different product sachets. They do so because they don’t have adequate income to cover other expenses (IDI_1, IDI_2, IDI_4, IDI_6, IDI_7, IDI_8, IDI_11, IDI_12, and IDI_13).
Training opportunities: Though substantial share of the interviews took at least a single relevant training, we understood that training opportunities are limited and not continuous, and limited refreshment trainings are being provided. The interviewees said that “though refreshment trainings are essential, they are not provided adequately.” Most of the time training is provided to health extension workers, coordinators and OTP focal persons do not have such opportunities. Some health extension workers are working simply by taking informal orientations about nutritional screening (IDI_1, IDI_2, IDI_3, IDI_4, IDI_5, IDI_6, IDI_7, IDI_8, IDI_9, IDI_10, IDI_11, IDI_12, IDI_13, and IDI_14).
Professional burn-outs: We understood that, most of health extension workers had extensive years of service, some had 11, 12, 15 years of service at the same area. The health extension workers are looking for further professional career opportunities, whereas there is “no known structure to upgrade”. Some of them had completed and have degree in nursing. Some health professionals do not consider health extension workers as an allied profession and consider them as a lower grade professional, which is disappointment to the HEW’s. Some members of the community believe that they are visiting homes for “personal payments” and this discourages them, though the service is very challenging and needs personal commitment. We have understood that some HEW’s feel they are “fade-up”, “need to be changed”, need to “end the HEW here” (IDI_3, IDI_5, IDI_9, and IDI_11).
Floating theme
Providers forward: We have summarized health care providers’ recommendations for better implementation of the service. They have forwarded that, community mobilization, mass awareness creation campaigns; working with community figures, family health team leaders, women development army and other stakeholders, improving access and utilization of family planning and child spacing, market surveys and control for black market RUTF/Plumpy-Nut sells, basic awareness to mothers on exclusive breast feeding, complementary feeding and food preparation demonstrations, shared responsibilities to other health professionals working in the facility and local stakeholders, regular screening service, first 1000 days maternal counseling, community income generation mechanisms, availing affordable food supplies in the market, tackle food insecurity problems, routine supervision and follow-ups, and health extension workers maternal leave associated workloads should be given due attention.
Discussion
This study illustrated that the treatment outcome of Outpatient Therapeutic Program (OTP), and explore barriers and facilitators with treatment outcomes of uncomplicated severe acute malnutrition in Eastern Ethiopia. The rate of treatment outcomes were 81.2%) with (SD: 0.57 95% CI, (75.1-87.3)), 22 (12.2%) with (SD: 0.57 95% CI (6.6-17.4)) and 12 (6.6%) with (SD: 0.57 95% CI (3.1-10.7)) were cure, defaulter and non-recovery respectively. The results of treatment outcome of severe acute malnutrition in therapeutics centers were in acceptable range compared to the sphere project reference values. This study was markedly in lined with the finding from Shebedino, Southern Ethiopia 79.6% (95% CI: 74.2-85.0%) of cases recovered, non-recovery was (11.1%).
This outcome was greater compared to similar finding from different countries: Wolaita zone, southern Ethiopia recovery rate was 64.9% (95% CI (61.5, 68.1) and defaulter rate (2.2%), tigray, northern Ethiopia recovery rate 61.78% and defaulter rate was 13.85%, northern Ethiopia 6.8% had recovered, north Shewa zone of Oromia region cure rate was 77.3%, non-recovery 9.9% and 7.8% was defaulter, Southwest Ethiopia the magnitude of recovery, defaulter and non-responder were 54.4%, 17%, 21.4% respectively, Gubalaf to Wereda, North Wollo Zone the recovery rate was 65%, and defaulter rate 16%, Dire Dawa Ethiopia recovery rate was 79.8%, defaulter rate 11.2%, non-responders was 3.8%. This finding was far greater than in Accra, Ghana 56·3 % defaulted, 34·5 % recovered and 8·6 % were not cured, Kabale district in southwestern Uganda indicated the cure rate was 36.3% with a median recovery time of 21 days. The default rate was 58.6% [24-28].
However, this result was less than with other finding from Gursum district, Somali region the recovery rate of severe acute malnutrition was 81.7%, defaulter rate was 12.6% and non-respondent was 0.9% [29], and Pakistan 98.7% had recovered [30]. This may be due to follow up quality, supplies availability and providing appropriate counseling of child mothers/care givers.
The qualitative finding of this study illustrated that the discussants have identified as the main themes under facilitating factors such as “collaboration, provider’s activity, structural factors, referral and communications and monitoring and reporting”. This finding has been support by different qualitative and quantitative studies: Study on a review of operational experiences in delivering severe acute malnutrition treatment through community health platforms [31], study from India [32], report on quality and effectiveness of CMAM services provision [33,34] and WHO framework on potential enablers and barriers influencing progress for the scale-up of CMAM program. However, discussant in sighted that “collaboration and provider activity” as facilitating factor for treatment outcomes. Logically working with stakeholders and health provider commitment has enormous contribution for treatment outcomes. It is known that for out-patient program effectiveness stakeholder’s involvement and community participation was crucial.
Furthermore, we have identified sub-themes discussants intensified that “community perception, defaulting, family wealth, food sharing, maternal education and awareness, supplies,” under barrier factors. Providers forward was identified as floating theme. This finding is similar with WHO framework of potential enablers and barriers influencing progress for the scale-up of CMAM program, the quality and effectiveness of CMAM services, study from India four main features as contributing to the success of the OTP program, A qualitative study in Rural Bangladesh, Bottleneck study from doolo zone of Somali region, report from community case management of severe acute malnutrition in Southern Bangladesh and a qualitative study in Pakistan and Ethiopia focused on common barriers.
However,” RUTF sharing, RUTF/Plumpy-Nut selling, training opportunities and professional burn-out” are identified as new barriers in this study. Indeed, the discussants ratified that “RUTF/Plumpy-Nut selling and sharing” were as main problem.
Limitation of the study was lacks of control mechanism for censoring cases because of the design nature. The seasonal variations of severe acute malnutrition were not considered and due to the prospective design of the study, confounding from unmeasured variables (e.g. vaccination status, exclusive breast feeding practice) cannot be entirely excluded. In addition, we were unable to incorporate statistical methods which account for small sample size.
Conclusion
All outcome indicators in this study showed that there were in the minimum standard set of sphere project values. However, the mean weight gain in the out-patient treatment center was not in acceptable range compared to sphere standard. The main barriers identified by discussants were “community perception, defaulting, family wealth, RUTF/Plumpy-Nut sharing, maternal education and awareness, supplies, RUTF/Plumpy-Nut selling, training opportunities and professional burn-out”. However,” RUTF/Plumpy-Nut sharing and selling, training opportunities and professional burn-out’ were barriers identified in this study. Policy makers, NGOs and managers need to consider those barriers seriously during program design. Providing nutritional behavioral change communication education through mass media regarding to RUTF/Plumpy-Nut, strengthening logistic supplies, training opportunities and design career development for health care providers can promote a better out-patient treatment outcomes.
Declaration
Ethics approval and consent to participate
Ethical approval was obtained from Institutional Review Board (IRB) Dire Dawa University. A formal letter of permission and support was taken and submitted to the dire dawa health bureau, haramaya woreda health office and Erer town health office. Bureau and health office wrote a formal letter for each health facilities. Informed, voluntary and written consent were taken. They were informed to keep the information confidential about the respondent. All data collection, cleaning, data entry, data processing and interpretation were performed based on Dire Dawa University research guidelines and protocols.
The Author’s Contributions
T.D, M, S. and B.T designed and conducted research; T.D and B.T, evaluate the content, analyzed, interpreted and wrote data; T.D, developed and writes manuscript draft and had primary responsibility for final validation. All authors read and approved the final manuscript.
Consent for Publication
Consent for publication is not necessary, because this manuscript did not contain any personal details like photos, images, or videos. All the summary from qualitative data has been cited properly.
Availability of Data and Materials
The data that support the findings of this study are available from correspondence author but restrictions apply to the availability of these data for privacy reason and so are not publicly available. Data are however available from the author upon reasonable request.
Competing Interests
The authors declare that there is no competing interest regarding this manuscript.
Funding
This project was funded by the research affairs directorate of Dire Dawa University. Dire Dawa University's main roles were to maintain ethical integrity throughout the process and validate the findings based on schedule.
Acknowledgements
First of all, we would like to thank Dire Dawa University for giving us the fund for this research. We are grateful to thank Dire Dawa regional health department's public health emergency management staff, Haramaya and Erer town health office for their positive corporation during the data collection process and ethical clearance processing. We also thanks all our data collectors and study participants.
References
- Frank T (2017) A mobile health application to manage acute malnutrition. Lessons from developing and piloting the app in five countries. World Vision/Save Children.
- Simachew Y, Zerfu T, Alemu W (2020) Treatment outcomes and predictors of recovery from severe acute malnutrition among children aged 6–59 months attending an outpatient therapeutic program in wenago district, Southern Ethiopia. Nutr Diet Suppl 12:189-200.
- UNICEF (2015) Management of severe acute malnutrition in children: Working towards results at scale. UNICEF programme guidance document New York (NY): UNICEF.
- Akwanyi B, James P, Lelijveld N, Mates E (2021) Scale-up of severe wasting management within the health system: A stakeholder perspective 5. Current Progress.
- Ayele S, Zegeye EA, Nisbett N (2020) Multi-sectoral nutrition policy and programme design, coordination and implementation in Ethiopia.
- Quak E-j (2021) Lessons learned from Community-based Management of Acute Malnutrition (CMAM) programmes that operate in fragile or conflict affected settings.
- Magge H, Kiflie A, Nimako K, Brooks K, Sodzi-Tettey S, et al. (2019) The Ethiopia healthcare quality initiative: Design and initial lessons learned. Int J Qual Health Care 31:180-186.
[Crossref] [Google Scholar] [PubMed]
- Organization WH (2017) Achieving quality universal health coverage through better water, sanitation and hygiene services in health care facilities: A focus on Ethiopia.
- Assefa Y, Hill PS, Gilks CF, Admassu M, Tesfaye D, et al. (2020) Primary health care contributions to universal health coverage, Ethiopia. Bull World Health Organ 98:894-905.
[Google Scholar] [PubMed]
- Yebyo HG, Kendall C, Nigusse D, Lemma W (2013) Outpatient therapeutic feeding program outcomes and determinants in treatment of severe acute malnutrition in Tigray, northern Ethiopia: A retrospective cohort study. Plos One 8:65840.
[Crossref] [Google Scholar] [PubMed]
- Tang A, Dong K, Deitcher M, Chung M, Maalouf-Manasseh Z, et al. (2013) Food and Nutrition Technical Assistance III project (FANTA). use of cutoffs for Mid‐Upper Arm Circumference (MUAC) as an Indicator or predictor of nutritional and health‐related outcomes in adolescents and adults: A systematic review.
- Puett C, Guerrero S (2015) Barriers to access for severe acute malnutrition treatment services in Pakistan and Ethiopia: A comparative qualitative analysis. Public Health Nutr 18:1873-1882.
[Crossref] [Google Scholar] [PubMed]
- Bekalu A, Sahlu D, Tadesse AW, Asmare B, Hune Y, et al. (2022) Time to recovery and determinants of uncomplicated severe acute malnutrition among 6 to 59 months children from the outpatient therapeutic feeding program in north Shewa zone of Oromia region, Ethiopia: A prospective follow-up study. Nutr Metab Insights 15:11786388221106984.
- Desalegn M, Kifle W, Birtukan T, Amanuel T (2016) Treatment outcome of severe acute malnutrition and determinants of survival in Northern Ethiopia: A prospective cohort study. Int J Nutr Metab 8:12-23.
- Hadley C, Linzer DA, Belachew T, Mariam AG, Tessema F, et al. (2011) Household capacities, vulnerabilities and food insecurity: Shifts in food insecurity in urban and rural Ethiopia during the 2008 food crisis. Soc Sci Med 73:1534-1542.
[Crossref] [Google Scholar] [PubMed]
- Galipeau R, Baillot A, Trottier A, Lemire L (2018) Effectiveness of interventions on breastfeeding self‐efficacy and perceived insufficient milk supply: A systematic review and meta‐analysis. Matern Child Nutr 14:e12607.
[Crossref] [Google Scholar] [PubMed]
- Kabalo MY, Seifu CN (2017) Treatment outcomes of severe acute malnutrition in children treated within Outpatient Therapeutic Program (OTP) at Wolaita Zone, Southern Ethiopia: retrospective cross-sectional study. J Health Popul Nutr 36:1-8.
[Crossref] [Google Scholar] [PubMed]
- Teshome G, Bosha T, Gebremedhin S (2019) Time-to-recovery from severe acute malnutrition in children 6-59 months of age enrolled in the outpatient treatment program in Shebedino, Southern Ethiopia: A prospective cohort study. BMC pediatr 19:1-10.
[Crossref] [Google Scholar] [PubMed]
- Wondie SG, Zinab B, Gizaw G, Tamrat M (2022) Time to recovery and its predictors among children aged 6-59 months with severe acute malnutrition admitted to outpatient therapeutic program in Southwest Ethiopia: retrospective cohort study. BMC pediatr 22:1-13.
[Crossref] [Google Scholar] [PubMed]
- Abate BB, Tilahun BD, Kassie AM, Kassaw MW (2020) Treatment outcome of severe acute malnutrition and associated factors among under five children in outpatient therapeutics unit in Gubalafto Wereda, North Wollo Zone, Ethiopia, 2019. PloS one 15:e0238231.
[Crossref] [Google Scholar] [PubMed]
- Atnafe B, Roba KT, Dingeta T (2019) Time of recovery and associated factors of children with severe acute malnutrition treated at outpatient therapeutic feeding program in Dire Dawa, Eastern Ethiopia. PloS one 14:e0217344.
[Crossref] [Google Scholar] [PubMed]
- Takyi A, Tette E, Goka B, Insaidoo G, Alhassan Y, et al. (2021) Treatment outcomes among children treated for uncomplicated severe acute malnutrition: A retrospective study in Accra, Ghana. Public Health Nutr 24:3685-3697.
[Crossref] [Google Scholar] [PubMed]
- Wamani H, Kitutu FE, Atukwase A (2022) Cure rate and associated factors for children 6-59 months with severe acute malnutrition under the outpatient therapeutic care programme in the health centres of Kabale District in Southwestern Uganda: A cross sectional study. BMC Nutr 8:1-8.
[Crossref] [Google Scholar] [PubMed]
- Budul AB, Farah AM, Nour TY (2020) Treatment outcome of severe acute malnutrition among children (6-59 months) in outpatient therapeutic feeding program in Gursum District, Somali region, Ethiopia. Science 8:36-42.
- Aguayo VM, Badgaiyan N, Qadir SS, Bugti AN, Alam MM, et al. (2018) Community Management of Acute Malnutrition (CMAM) programme in Pakistan effectively treats children with uncomplicated severe wasting. Matern Child Nutr 14:e12623.
[Crossref] [Google Scholar] [PubMed]
- López‐Ejeda N, Charle Cuellar P, Vargas A, Guerrero S (2019) Can community health workers manage uncomplicated severe acute malnutrition? A review of operational experiences in delivering severe acute malnutrition treatment through community health platforms. Matern Child Nutr 15:e12719.
[Crossref] [Google Scholar] [PubMed]
- More NS, Waingankar A, Ramani S, Chanani S, D'Souza V, et al. (2018) Community-based management of acute malnutrition to reduce wasting in urban informal settlements of Mumbai, India: A mixed-methods evaluation. Glob Health Sci Pract 6:103-127.
[Crossref] [Google Scholar] [PubMed]
- Ireen S, Raihan MJ, Choudhury N, Islam MM, Hossain MI, et al. (2018) Challenges and opportunities of integration of community based management of acute malnutrition into the government health system in Bangladesh: A qualitative study. BMC Health Serv Res 18:256.
[Crossref] [Google Scholar] [PubMed]
- Shrimpton R, du Plessis LM, Delisle H, Blaney S, Atwood SJ, et al. (2016) Public health nutrition capacity: Assuring the quality of workforce preparation for scaling up nutrition programmes. Public Health Nutr 19:2090-2100.
[Crossref] [Google Scholar] [PubMed]
- Mathur M, Halim A, Gupta M, Panda B, Syed A (2018) Community-based Management of Acute Malnutrition (CMAM) in India: A position paper. Int J Res Med Sci 6:4128-4135.
- Arafat Y, Islam MM, Connell N, Mothabbir G, McGrath M, et al. (2018) Perceptions of acute malnutrition and its management in infants under 6 months of age: A qualitative study in rural Bangladesh. Clin Med Insights Pediatr 12:1179556518771698.
[Crossref] [Google Scholar] [PubMed]
- Farah AE, Abas AH, Ahmed AT (2020) Bottlenecks and met needs for the treatment of severe acute malnutrition in pastoralists: Doolo zone of Somali region, Ethiopia.
- Sadler K, Puett C, Mothabbir G, Myatt M (2011) Community case management of severe acute malnutrition in southern Bangladesh. Boston: Tufts University.
- Deconinck H, Swindale A, Grant F, Navarro-Colorado C (2008) Review of Community-based Management of Acute Malnutrition (CMAM) in the post-emergency context: Synthesis of lessons on integration of CMAM into national health systems. Washington DC: FANTA.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi