Case Report, Agcr Vol: 9 Issue: 1
Treatment of Thin Endometrium with Hysteroscopic Autologous Platelet Rich Plasma Injection
Gokalp Oner*
Department of Obstetrics and Gynecology, Kayseri Acibadem Hospital, Turkey
*Corresponding Author:
Gokalp Oner
Department of Obstetrics and Gynecology
Kayseri Acibadem Hospital, Turkey
Tel: +905062346822
E-mail: onerg@yahoo.com
Received: December 02, 2020 Accepted: December 08, 2020 Published: January 16, 2021
Citation: Oner G (2021) Treatment of Thin Endometrium with Hysteroscopic Autologous Platelet Rich Plasma Injection. Androl Gynecol: Curr Res 9:1.
Abstract
In infertility treatments, one of the most hardest problem is thin endometrium which is neccessary affect implantation. Recently, autologous Platelet Rich Plasma (PRP) injection has been prefered with catheter injection into the uterin cavity. The results are conflict between the series. Our patients diagnosed with thin endometrium failed to respond medical treatment. This case series reports on three women which has thin endometrium and history of recurrent implantation failure. We defined a new technique for PRP injection into the endometrium with hysteroscopy. Following the hysteroscopic PRP treatment, three patients that previously failed In Vitro Fertilization (IVF) performed IVF and achieved pregnancy. This is the first case report to define this technique in the literature and get pregnancy.
Keywords: Platelet Rich Plasma, Hysteroscopy, Endometrium, Embryo Transfer
Keywords
Platelet Rich Plasma; Hysteroscopy; Endometrium; Embryo Transfer
Introduction
The main aim of In Vitro Fertilization (IVF) is to have a good embryo and sufficient endometrium for implantation. Two factors directly affects the pregnancy outcomes of IVF. The minimum endometrial thickness was defined as 7 mm and lower than 7 mm is defined as thin endometrium which may negatively affect the implantation and also pregnancy rates [1,2]. Although several medical treatments have been attempted to increase thin endometrium including estrogen treatment, aspirin, sildenafil, vitamin E, Granulocyte-Colony Stimulating Factor (G-CSF), there is no efficient method described [3]. Additionally, some cases have not got a response to the medical treatment. In that cases autologous Platelet Rich Plasma(PRP) injection into the uterin cavity with a catheter has been prefered recently [2-4].
PRP is blood plasma prepared from fresh whole blood included with excessive platelets. Platelets have positive effects on the tissue repair and also contain a significant amount of growth factors which stimulate proliferation and growth like Vascular Endothelial Growth Factor (VEGF), Epidermal Growth Factor (EGF), Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor (TGF), and other cytokines [5].
In Frozen Thawed Embryo Transfer (FET) cycles, thin endometrium negatively affects the implantation and because of this, cycles are cancelled in IVF. Endometrial thickness is so pivotal for implantation and more than 7 mm significantly improved pregnancy outcomes [6]. Therefore endometrial thickness is directly affected to the FET cycles in IVF. Diagnostic hysteroscopy is the golden standart technique to develop the endometrial pathologies, especially thin endometrium [3].
The aim of this study was to evaluate the effects of a new technique for PRP injection into the endometrium with hysteroscopy on implantation and pregnacy outcomes in FET cycles.
Material and Methods
All patients has previous unsuccessful IVF attempts beacuse of thin endometrium (<7mm) and referred to our clinic. After the examination of the patients, 6 mg/daily estradiol valerate (Estrofem Novo Nordisk®) were used 14 days and endometrial thichness was measure thinner than 7 mm. There has been no problem and treatment in the medical histories of the patients such as Diabetes Mellitus, Thyroid diseases, Hyperprolactinemia, and Hypertension.
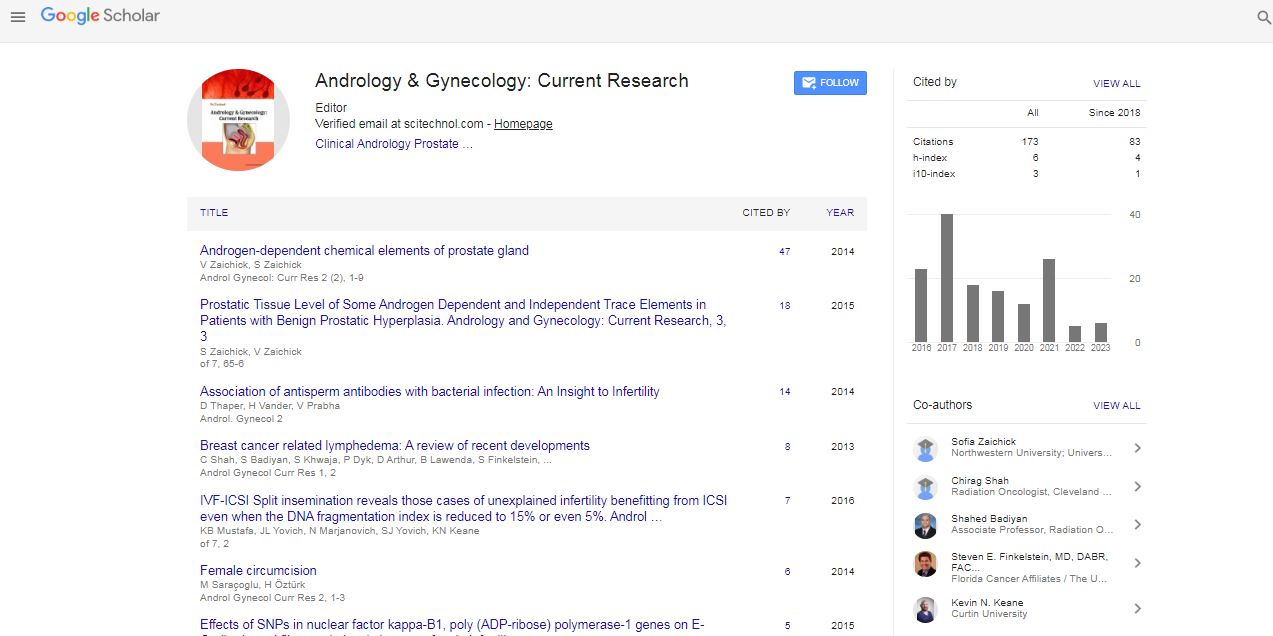
PRP was extracted from 60 ml of the patient’s peripheral blood. The concentration of platelets from the peripheral blood sample was approximately 250,000/mL and PRP was administered immediately following preparation. Office Hysteroscopy (OH) was performed to apply the injection of PRP into the uterus (Figure 1) during the proliferative phase of the menstrual cycle. In all OH procedures, a speculum and a tenaculum were used for the vaginoscopic approach. Single dose penicillin was chosen for antibiotic prophylaxis. The device used is a rigid hysteroscope (continuous flow, 30 degree forward oblique view) assembled in a 5mm diameter diagnostic rigid sheath with an atraumatic tip (Karl Storz Endoscopy®). A single hysteroscopic needle was used for injection of PRP (Figure 1). Midazolam (0.1 mg/kg) was administered to the all patients for sedation during the procedure. There has been no complication after the operations.

Figure 1: The hysteroscopic PRP injection into the thin endometrium; a)Injection of PRP by hysteroscopic needle; b) Holes of PRP into the endometrium.
In all patients, COH was performed using Gonadotropin- Releasing Hormone (GnRH) antagonist protocols and exogenous gonadotropins including recombinant Follicle Stimulating Hormone (FSH) and Human Menopausal Gonadotropin (hMG) after usage of oral contraceptive in the second day of menstrual cycle (D2). When lead follicles reached to 17 mm diameter, final oocyte maturation was induced using an intramuscular injection of 6000 IU hCG (Ovitrelle). Oocyte retrieval via transvaginal ultrason guided needle aspiration of ovarian follicular fluid was performed 36 hour later. Sperm was processed for insemination or intracellular sperm injection as previously described technique [7]. Normally fertilized zygotes exhibiting two Pronuclei (PN) were cultured to day 3 in four well dishes including approximately 400 μl single step media (LifeGlobal ® Media, USA) and monitored for embryonic development with EmbryoScope (Vitrolife AB; Sweden). The stages of blastocyst development were assessed with the Gardner classification [8]. All blastocysts subjected to TE biopsy were vitrified immediately by using the vitrification Kit and Cryotops (Kitazato, Japan). Frozen Thawed ET was scheduled after the patient’s next menses and artificial endometrium was prepared. In artificial endometrium of all patients, endometrial preparing was performed with estradiol valerate, at 6 mg/daily, taken orally from day 2 to 11 of the menstrual cycle. 11th day of the cycle endometrial thickness was measured by transvaginal ultrasound. If the endometrium measured more than 7 mm, 6 mg estradiol valerate continued and the vaginal progesterone (Crinone Jel) was added on the day of 14th of the cycle. Frozen-Thawed ET was performed on the 5th or 6th day of Progesterone adjustment. Estrogen and Progesterone was continued at 10 weeks of pregnancy.
Case Reports
Case 1
Patient 1 (aged 33 years old) was referred to our clinic with the diagnosed of thin endometrium and absence of menstrual cycle. Body Mass Index (BMI) of the patient was 27 kg/m2. In the reproductive history of the patient, one probe Dilatation and Curretage (D&C) because of missed abortion and one unsuccessful IVF attempt has been found. Bilateral ovaries are grade 3 and Anti-Müllerian Hormone (AMH) level is 2.1. After the IVF procedure, the patient has 3 frozen blastocyst embryo. Then, hysterocopy was performed in the proliferative phase of endometrium and 20 ml PRP was injected into the cavity after the opening of the adhesions with hysteroscopic scissors. Ethinyl estradiol (0.03 mg)and drospirenone (3 mg) combination of oral contraceptive was used in one month then artificial endometrium was prepared. Endometrial thisckness was 8.3 mm during the frozen thawed embryo transfer. Currently, the successful full-term delivery was happened with normal birth weights without any complications.
Case 2
Patient 2 (29 years old) was referred to our clinic with the diagnosed of thin endometrium and recurrent implantation failure. In the reproductive history of the patient, one operative hysteroscopy enlargement metroplasty for T-shaped uterus and four unsuccessful IVF attempts has been found. Bilateral ovaries are grade 2 and Anti-Müllerian Hormone (AMH) level is 1.7. After the IVF procedure, the patient has 2 frozen blastocyst embryo. Then, hysterocopy was performed in the proliferative phase of endometrium and 20 ml PRP was injected into the cavity. Ethinyl estradiol (0.03 mg) and drospirenone (3 mg) combination of oral contraceptive was used in one month then artificial endometrium was prepared. Endometrial thisckness was 11.5 mm during the frozen thawed embryo transfer. Currently, the patient is at 27 weeks gestation with normal prenatal screening tests.
Case 3
Patient 3 (34 years old) was referred to our clinic with the diagnosed of thin endometrium and recurrent implantation failure. In the reproductive history of the patient, one operative hysteroscopy for endometrial injury in order to increase implantation and six unsuccessful IVF attempts has been found. Bilateral ovaries are grade 1 and Anti-Müllerian Hormone (AMH) level is 0.9. After the IVF procedure, the patient has 1 frozen blastocyst embryo. Then, hysterocopy was performed in the proliferative phase of endometrium and 20 ml PRP was injected into the cavity. Ethinyl estradiol (0.03 mg) and drospirenone (3 mg) combination of oral contraceptive was used in one month then artificial endometrium was prepared. Endometrial thisckness was 7.5 mm during the frozen thawed embryo transfer. Currently, the patient is at 12 weeks gestation with normal prenatal screening test.
Discussion
Thin endometrium is defined as endometrial thickness <7 mm (frozen cycles) or <8 mm (fresh cycles) in Assisted Reproduction Technique (ART) [9]. The incidence of thin endometrium is between 1% and 2.5% in ART [9,10]. Most common pathological causes of thin endometrium may include Asherman syndrome, history of uterine surgery, infection, and radiation [10]. The golden standart technique to evaluate pathological reasons in the uterine cavity is hysteroscopy or sonohysterogram [9] and the efficacy of the standart medical treatments are not kindly effective [9]. Therefore, PRP has been infused to endometrium and caused successful results for endometrial growth in patients with thin endometrium, recently [1,3,9]. In our study, three patients who had a history of thin endometrium caused unsuccessful IVF attempts and unresponsive endometrium to the medical treatment.
Endemetrial thickness is pivotal for implantation and pregnancy. In patient with persistent thin endeometrium, ET has been often cancelled. Although several methods have been found for endometrial preparation, there has been no any successful method, yet. Recently, local infusion of G-CSF which is a cytokine that stimulates endometrial proliferation may used for thin endometrium [9], however there has been several growth factors and cytokines in PRP. PRP that is collected from autologous blood sample of the patient is also more accessible. In our study, PRP was effectively used without any complication.
The catheter is commonly used for the application of PRP therapy into the uterine cavity in order to prepare the endometrium in the literature [1-4]. In our study, we differently used office hysterocopy and PRP was firstly injected into the endometrium in the literature. In our hypothesis, there has been two advantage to apply hysteroscopic PRP injection; the first one is to evaluate and interfere any pathology in the uterine cavity and second one is PRP injected into the endometrium which was more absorbable and effective than surficial PRP application. In our study, three cases have adequite endometrium to have pregnancy.
In conclusion, it seems that hysteroscopic PRP technique is more safe and reliable method in patients with thin endometrium. During fresh IVF cycles, if the endometrium is not enough to transfer embryo, all embryos may be frozen and transfer after hysteroscopic PRP technique. In our study, we firstly described this technique in the literature. We suggest further prospective clinical trials.
References
- Eftekhar M, Neghab N, Naghshineh E, Khani P (2018) Can autologous platelet rich plasma expand endometrial thickness and improve pregnancy rate during frozen-thawed embryo transfer cycle? A randomized clinical trial. Taiwan J Obstet Gynecol 57: 810-813.
- Nazari L, Salehpour S, Hoseini S, Zadehmodarres S, Azargashb E (2019) E. Effects of autologous platelet-rich plasma on endometrial expansion in patients undergoing frozen-thawed embryo transfer: A double-blind RCT. Int J Reprod Biomed 17: 443-448.
- Zadehmodarres S, Salehpour S, Saharkhiz N, Nazari L (2017) Treatment of thin endometrium with autologous platelet-rich plasma: a pilot study. JBRA Assist Reprod 21: 54-56.
- Kim H, Shin JE, Koo HS, Kwon H, Choi DH, et al. (2019) Effect of autologous platelet-rich plasma treatment on refractory thin endometrium during the frozen embryo transfer cycle: A pilot study. Front Endocrinol (Lausanne) 10: 61.
- Farimani M, Bahmanzadeh M, Poorolajal J (2016) A new approach using autologous platelet-rich plasma (PRP) to treat ├?┬▒nfertility and to ├?┬▒mprove population replacement rate. J Res Health Sci. 16: 172-173.
- Krief F, Simon C, Goldstein R, Ellenberg LP, Ledee N (2019) Efficacy of tocopherol and pentoxifylline combined therapy for women undergoing assisted reproductive treatment with poor endometrial development: a retrospective cohort study on 143 patients. Hum Fertil (Camb) 10: 1-9.
- Gardner DK, Lane M (1997) Culture and selection of viable blastocysts: a feasible proposition for human IVF?. Hum Reprod Update 3: 367-82.
- Harton GL, Munne S, Surrey M, Grifo J, Kaplan B, (2013) et al. Diminished effect of maternal age on implantation after preimplantation genetic diagnosis with array comparative genomic hybridization. Fertil Steril 100: 1695-703.
- Liu KE, Hartman M, Hartman A (2019) Management of thin endometrium in assisted reproduction: a clinical practice guideline from the Canadian Fertility and Andrology Society. Reprod Biomed Online. 39: 49-62.
- Liu KE, Hartman M, Hartman A, Luo ZC, Mahutte N (2018) The impact of a thin endometrial lining on fresh and frozen-thaw IVF outcomes: an analysis of over 40000 embryo transfers. Hum Reprod 33(10): 1883-1888.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi