Review Article, J Pulm Med Vol: 2 Issue: 1
The Outcome of an Emergency Respiratory Admission: Influence of Air Pollution and Humidity
Nadim Akasheh*, Declan Byrne, Deirdre O’Riordan and Bernard Silke
Department of Internal Medicine, St James’s Hospital, Dublin 8, Ireland
*Corresponding Author : Dr. Nadim Akasheh
Department of Internal Medicine, St James’s Hospital, Dublin 8, Ireland
Tel: +353 1 4103000
Fax: +353 1 410 3451
E-mail: naakasheh@stjames.ie
Received: November 19, 2018 Accepted: December 03, 2018 Published: December 10, 2018
Citation: Akasheh N, Byrne D, O’Riordan D, Silke B (2018) The Outcome of an Emergency Respiratory Admission: Influence of Air Pollution and Humidity. J Pulm Med 2:1.
Abstract
Background: Both prevailing air pollution or humidity levels may influence the outcome of an acute hospital episode; we investigated whether higher pollutant or humidity levels on the day of a respiratory admission were associated with worse outcomes.
Methods: Between 2002 and 2016, we studied all emergency medical admissions (96,526 episodes in 50,731 patients) and investigated air pollutant levels (sulphur dioxide) and humidity levels on the day of admission. We employed a logistics multiple variable regression model, to identify the extent to which the prevailing pollutant or humidity levels influenced 30day hospital mortality outcome, stratified by respiratory or nonrespiratory type, having adjusted for other outcome predictors including Acute Illness Severity and Case Co-morbidity/ Complexity.
Results: Respiratory admission were older-70.2 yr. (IQR: 55.0, 79.9) vs. 59.6 yr. (IQR: 39.1, 77.8], had a longer hospital length of stay – 7.0 days (IQR: 3.4, 14.7] vs. 5.1 days (IQR: 1.9, 11.8%] and a higher 30-day hospital episode mortality – 7.9% (95% CI: 7.7%, 8.2%] vs. 4.0% (95% CI: 3.8%, 4.2%]. The pollutant level on the day of admission (SO2 quintiles) predicted worsening outcomes from Q2 – OR 1.40 (95% CI: 1.21, 1.62) to Q5 – OR 2.57 (95% CI: 2.18, 3.03) with an overall Odd Ratio for SO2 level of 1.27 (95% CI: 1.23, 1.32). There was significant interaction between pollutant and humidity levels and respiratory category. With saturated air (humidity>95%), the predicted 30-day hospital mortality for SO2 quintiles Q3 and Q5 was 11.2% and 12.4% respectively but with dry air (humidity<70%) the predicted mortality rose to 14.2% and 16.7% respectively. At any given humidity and pollutant level, respiratory patients had worse outcomes.
Conclusion: Baseline air pollutant and humidity levels influenced 30-day hospital mortality outcomes. At any given levels, the outcome for respiratory patients was significantly worse.
Keywords: Air pollution; Humidity; Interactions; Mortality outcomes
Introduction
According to the World Health Organization (WHO) report in 2008, 1.3 million deaths were estimated to be related to ambient air pollution globally. By 2012, this figure had nearly tripled to 3.7 million [1]. Long-term ambient air pollution exposure has been associated with an increase in all-cause mortality [1]. It is an etiological and aggravating factor of many respiratory diseases such as chronic obstructive pulmonary disease (COPD) [2,3], asthma [4], and lung cancer [5,6]. Poor air quality also deleteriously impacts other organ systems and is associated with cardiovascular [7,8], gastrointestinal [9] and neurological diseases [10].
Concern raised regarding the public health implications of urban air pollution in a paper from our institution [11] in Dublin resulted in legislation in 1990 controlling the marketing, sale and distribution of bituminous coals. The average black smoke concentration fell by approximately 35.6 μg/m3 with an estimated reduction in respiratory deaths by 15.5% and cardiovascular deaths by 10.3% [12].
Both temperature and humidity are also important determinants of mortality. The humidity-mortality relationship is U-shaped and large in magnitude at the extremes [13]. In the epidemiological literature regarding the effects of humidity on health is difficult to interpret. This is due to the fact that the effects of humidity are often inferred from measurements that are directly linked to temperature (relative humidity) or synoptic climatological analyses [14].
In general, water vapour status is linked to mortality and morbidity through its role in affecting fluid homeostasis and thermoregulation due to impaired surface evaporation rates with high humidity levels and dehydration which could be worsened by dry weather conditions [14]. Low humidity levels have been associated with increases in COPD exacerbations [15] and bronchial hyper reactivity in asthmatic patients [16]. Low absolute humidity was found to be a critical determinant of human influenza mortality [17] and is thought to trigger a variety of other respiratory tract infections [18]. Humidity could also indirectly adversely impact respiratory disease via the spread of bacteria, fungi, and dust mites [13]. Over the last 10 years reports in the literature have also suggested that humidity may modify the effects of air pollution on respiratory disease.
Our hospital serves an inner city catchment area with high levels of social deprivation living in close proximity to severe motor traffic congestion [19]. Car ownership levels in the area have increased substantially in the last 5 years to levels proceeding the economic recession of 2008-2014. In this study therefore we examined data relating to 106,586 emergency medical admissions to St James’ Hospital, Dublin over a 16-year period (2002-2017) to evaluate how ambient Sulphur Dioxide (SO2) concentrations and humidity levels on the day of admission impact the 30-day mortality outcomes of acute respiratory and non-respiratory admissions.
Methods
Background
St James’s Hospital, Dublin serves as a secondary care centre for emergency admissions in a catchment area with a population of 270,000 adults. All emergency medical admissions were admitted from the ED to an Acute Medical Admission Unit, the operation and outcome of which have been described elsewhere [20,21]. As a city centre hospital St James’s admits person resident elsewhere but working in the capital in addition to visitors to Dublin who became acutely ill. The number of emergency medical admissions resident in the catchment area was 74.5%; this compares with a figure of 59% for emergency department presentations where the social influences on emergency department visitations on two London hospitals have been examined [22].
Data collection
An anonymous patient database was employed, collating core information of clinical episodes from the Patient Administration System (PAS), the national hospital in-patient enquiry (HIPE) scheme, the patient electronic record, the emergency room and laboratory systems. HIPE is a national database of coded discharge summaries from acute public hospitals in Ireland [23,24]. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) has been used for both diagnosis and procedure coding from 1990 to 2005 with ICD-10-CM used since then. Data included parameters such as the unique hospital number, admitting consultant, date of birth, gender, area of residence, principal and up to nine additional secondary diagnoses, principal and up to nine additional secondary procedures, and admission and discharge dates. Additional information cross-linked and automatically uploaded to the database includes physiological, haematological and biochemical parameters.
Our hospital catchment area contains many small areas characterised by a high deprivation status [19]. The Republic of Ireland census (Central Statistical Office) report small area population statistics (SAPS); the smallest reporting unit is the Electoral Division (ED). Of the total of 3409, 74 Electoral Divisions are in the hospital catchment area. The catchment area population, measured in 2006, was 210,443 persons, with a median population per ED of 2845 (IQR 2020, 3399). Deprivation metrics have been determined by the Small Areas Health Research Unit (SAHRU) of Trinity College Dublin using methodology similar to Townsend [25] and Carstairs [26] to derive a Deprivation Score based on four indicators, relating to unemployment, social class, type of housing tenure and car ownership [27]. The assignment of patients to small area population area used the ArcGS Geographic Information System software implementation of the wellknown Point-in-Polygon algorithm as outlined by Shimrat [28].
Acute illness severity score
Derangement of biochemical parameters may be utilised to predict clinical outcome. We derived an Acute Illness Score based on laboratory data – this is an age adjusted 30-day inhospital mortality risk estimator, representing an aggregrate laboratory score based on the admission serum sodium (Na), serum potassium (K), serum urea, red cell distribution width (RDW), white blood cell count (WCC), serum albumin and troponin values at admission and applied as an Acute Illness Severity score [29,30]; the score predicts 30-day inhospital mortality from the biochemical parameters recorded in the Emergency Department [31]. The Illness Severity score can be enhanced with data from the ICD9/10 discharge codes to compute Co- Morbidity (as per the Charlson Index [32]) and chronic disabling disease status [33]. This Risk Score is exponentially related to the 30- day episodes mortality outcome with a range of model adjusted mortality outcomes from 2.5% (2.3%– 2.6%) to 32.1% (30.4%-33.8%). We have demonstrated using a nomogram that this laboratory models derives most of its predictive power from the values of albumin, urea and haemoglobin recorded at the time of admission [34].
Air quality
For the current study, data over the last decade (2002-2016) from three stations within our hospital catchment area (Winetavern and Coleraine Street or Rathmines stations) were assessed and hourly SO2 were recorded, according to methods detailed elsewhere [35]. A single average value for each day was calculated for the analyses. We divided the daily levels into equally spaced quintiles – SO2 quintile cut-points were 0.93, 1.54, 2.32 and 4.14 μg/m3 respectively.
Statistical Methods
Descriptive statistics were calculated for demographic data, including means/standard deviations (SD), medians/interquartile ranges (IQR), or percentages. We examined 30-day in-hospital mortality as the primary outcome. We performed comparisons between categorical variables and 30-day in hospital mortality using chi-square tests; multiple comparisons were adjusted for multiplicity using Scheffe’s comparison statistic. Logistic regression analysis was employed to examine significant outcome predictors (p<0.10 by Wald test from the univariate analysis) of 30-day in hospital mortality to ensure that the model included all variables with predictive power. Adjusted Odds Ratios (OR) and 95% confidence intervals (CI) were calculated for those significant model predictors. A stepwise logistic regression analysis examined the association between 30-day mortality and the following predictor variables: Acute Illness Severity [30,36,37], Charlson Co-Morbidity Index [32], and Chronic Disabling Disease [33], sepsis status [38] and Deprivation index according to the Quintiles of the SAHRU deprivation number.
We used the margins command in Stata to estimate and interpret adjusted predictions for sub-groups, while controlling for other variables such as time, using computations of average marginal effects. Margins are statistics calculated from predictions of a previously fitted model at fixed values of some covariates and averaging or otherwise over the remaining covariates. In the multiple variable logistic model we adjusted univariate estimates of effect, using the previously described outcome predictor variables. The model parameters were stored; post-estimation intra-model and cross-model hypotheses could thereby be tested.
Statistical significance at P<0.05 was assumed throughout. Stata v.15 (Stata Corporation, College Station, Texas) statistical software was used for analysis.
Results
Patient demographics
A total of 96,526 episodes in 50,731 unique patients were admitted as medical emergencies from the hospital catchment area over the 15- year study period (2002-2016). These episodes represented all emergency medical admissions, including patients admitted directly into the Intensive Care Unit or High Dependency Unit, respectively. The proportion of males was 48.6%. The median (IQR) length of stay (LOS) was 4.4 (1.8, 8.9) days. The median (IQR) age was 58.7 (38.0, 76.2) yrs, with the upper 10% boundary at 84.9 yrs. (Table 1).
| Other | Respiratory | ||
|---|---|---|---|
| (N=58723) | (N=37803) | p-value | |
| Age (yr) | |||
| Mean (SD) | 58.03 (21.73) | 66.17 (17.85) | <0.001 |
| Median (Q1, Q3) | 59.6 (39.1, 77.6) | 70.2 (55.0, 79.9) | - |
| Length Stay (day) | |||
| Mean (SD) | 13.74 (35.33) | 16.43 (36.18) | <0.001 |
| Median (Q1, Q3) | 5.1 (1.9, 11.8) | 7.0 (3.4, 14.7) | - |
| Gender | - | ||
| Male | 28800 (49.2%) | 18080 (47.9%) | <0.001 |
| Female | 29789 (50.8%) | 19636 (52.1%) | - |
| 30-day Hospital Mortality | |||
| Alive | 56246 (96.0%) | 34723 (92.1%) | <0.001 |
| Dead | 2344 (4.0%) | 2993 (7.9%) | - |
| Illness Severity Score | |||
| 1 | 2234 (4.2%) | 313 (0.9%) | <0.001 |
| 2 | 4844 (9.2%) | 1070 (3.0%) | - |
| 3 | 7510 (14.2%) | 2542 (7.2%) | - |
| 4 | 9080 (17.2%) | 4787 (13.6%) | - |
| 5 | 9982 (18.9%) | 7042 (19.9%) | - |
| 6 | 19132 (36.2%) | 19545 (55.4%) | - |
| Disabling Disease | |||
| 0 | 8098 (13.8%) | 1727 (4.6%) | <0.001 |
| 1 | 15993 (27.3%) | 7027 (18.6%) | - |
| 2 | 17806 (30.4%) | 10180 (27.0%) | - |
| 3 | 11035 (18.8%) | 10273 (27.2%) | - |
| 4 | 5658 (9.7%) | 8509 (22.6%) | - |
| Charlson Index | |||
| 0 | 32705 (55.9%) | 9922 (26.4%) | <0.001 |
| 1 | 12501 (21.4%) | 14104 (37.5%) | - |
| 2 | 13264 (22.7%) | 13608 (36.2%) | - |
| Sepsis Group | |||
| 1 | 45421 (77.5%) | 25520 (67.7%) | <0.001 |
| 2 | 10764 (18.4%) | 10260 (27.2%) | |
| 3 | 2405 (4.1%) | 1936 (5.1%) | |
Table 1: Characteristics of respiratory medical admission episodes.
The demographic characteristics (Table 1) are outlined for with comparison of the characteristics of respiratory and non-respiratory cases, by principal admission diagnosis. The characteristics are tabulated by Acute Illness Severity [29,30], Chronic Disabling Score [33], Charlson Co-morbidity Index [32] and Sepsis status [38]. In terms of baseline characteristics, respiratory admissions were older 70.2 yr. (IQR: 55.0, 79.9) vs. 59.6 yr. (IQR: 39.1, 77.8], had a longer hospital length of stay – 7.0 days (IQR: 3.4, 14.7] vs. 5.1 days (IQR: 1.9, 11.8%] and a higher 30-day hospital episode mortality – 7.9% (95% CI: 7.7%, 8.2%] vs. 4.0% (95% CI: 3.8%, 4.2%]. Respiratory admissions were clearly at higher risk as evidenced higher levels of Acute Illness Severity, Chronic Disabling Score, Charlson Co-morbidity Index and Sepsis grade.
Temperature and Humidity Variation with Season
The median and range (IQR) for Humidity levels were 84% (78%, 91%) with respective 10 and 90 cent values at 54% and 91%. The variation by season range from a maximum of 88% (83%, 91%) in winter to a minimum of 80% (74%, 87%) in summer. Humidity cutpoints per quintile were at 77%, 82%, 86% and 91% values; high humidity was taken to be at Q3 or above (>= 83%). The median temperature was 11.1°C (7.2, 12.8) with respective 10 and 90 cent values at 4.4°C and 15.2°C. The variation by season range from a maximum of 17.3°C (15.2, 19.5) in summer to a minimum of 3.7°C (1.8, 5.7) in winter.
Logistic multiple variable predictor model of air pollutant level (SO2) humidity and their interaction of 30-day mortality outcome
Both humidity and the air pollutant level on the day of admission predicted the 30-day hospital mortality; higher levels of pollutant or drier air predicted worse outcomes. The SO2 level on the day of admission showed worsening outcomes with rising pollutant levels. The median increase in pollutant levels was from Q2-0.59 μg/m3 (IQR: 0.31, 0.76) to Q3-1.87 μg/m3 (IQR: 1.70, 2.08) and Q5 – 5.90 μg/m3 (IQR: 5.00, 8.25). The 30-day hospital mortality risk increased from Q2 (comparisons with base QI level) – OR 1.40 (95% CI : 1.21, 1.62) to Q5 – OR 2.57 (95% CI : 2.18, 3.03) with an overall Odd Ratio for SO2 level of 1.27 (95% CI : 1.23, 1.32) (Table 2, Figure 1).
| Predictor variable | Odds ratio | Std. Err. | z | P>|z| | [95% Conf. Interval] | |
|---|---|---|---|---|---|---|
| SO2 Quintile | ||||||
| QII | 1.4 | 0.1 | 4.6 | 0 | 1.21 | 1.62 |
| QIII | 1.73 | 0.13 | 7.2 | 0 | 1.49 | 2.01 |
| QIV | 2.39 | 0.19 | 11 | 0 | 2.05 | 2.79 |
| QV | 2.57 | 0.22 | 11.2 | 0 | 2.18 | 3.03 |
| Humidity Group | ||||||
| >=70%<85% | 1.26 | 0.15 | 1.9 | 0.05 | 1 | 1.61 |
| >=85%<95% | 1.28 | 0.17 | 1.9 | 0.06 | 0.99 | 1.65 |
| >=95% | 1.39 | 0.26 | 1.7 | 0.08 | 0.96 | 2.02 |
| Illness Severity | 3.9 | 0.17 | 30.6 | 0 | 3.58 | 4.26 |
| Charlson Index | 1.52 | 0.05 | 13.8 | 0 | 1.43 | 1.61 |
| Disabling Group | 1.16 | 0.03 | 6.3 | 0 | 1.11 | 1.22 |
| Sepsis | 2.18 | 0.07 | 22.7 | 0 | 2.04 | 2.33 |
| Deprivation | 1.08 | 0.02 | 4 | 0 | 1.04 | 1.13 |
| Average Temp | 0.98 | 0.01 | -4.2 | 0 | 0.97 | 0.99 |
| Respiratory | 1.88 | 0.15 | 7.8 | 0 | 1.61 | 2.2 |
| SO2 # Humidity | 0.95 | 0.01 | -3.8 | 0 | 0.92 | 0.97 |
Table 2: Multivariable logistic regression model of mortality outcome.
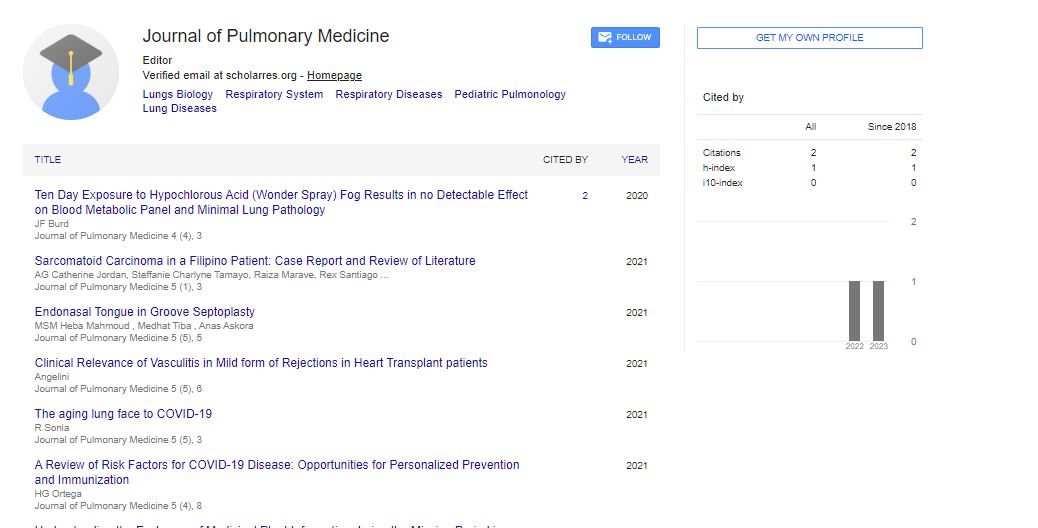
Figure 1: The risk of a death by the 30-day of a hospital episode increased essentially as a linear function of to the underlying SO2 Quintile at the time of hospital admission. The mortality outcome, plotted against discrete Humidity levels was adjusted in the model for Acute Illness Severity, Charlson Co-Morbidity Score, Chronic Disabling and Sepsis Status. Lower admission humidity levels, at a given pollutant quintile, independently predicted worse outcomes.
Humidity had a weaker trend to predict worse outcomes as the level of humidity fell; the interaction term between air pollution level, the level of humidity and being a respiratory patient was significant (Table 2). Mortality was higher with drier air overall. We used margins statistics to estimate and interpret adjusted predictions for sub-groups, while controlling for other variables, using computations of average marginal effects. We adjusted these predictors for other confirmed outcome factors including the Acute Illness Severity, Chronic Disabling Disease Score, Charlson Co-morbidity Index, and Sepsis status. All of these variables were powerful 30-day mortality outcome predictors-Acute Illness Severity OR 3.90 (95% CI: 3.58, 4.26), Charlson Co-morbidity Index-OR 1.52 (95% CI: 1.43, 1.61), Chronic Disabling Disease Score-OR 1.16 (95% CI: 1.11, 1.22), Sepsis Status- OR 2.18 (95% CI: 2.04, 2.33) and Deprivation Index based on area of residence-OR 1.08 (95% CI: 1.04, 1.13). A Respiratory Patient classification was also a powerful (worse) outcome predictor OR 1.88 (95% CI: 1.61, 2.20).
The risk of a death by the 30-day of a hospital episode increased essentially as a linear function of to the underlying SO2 Quintile at the time of hospital admission (Figure 1). For example, when the air was saturated (humidity>95%) the predicted mortality overall at the third and fifth quintiles of SO2 were 11.2% and 12.4% but with lower humidity values between 50% and 70% would have risen to an estimated 14.2% and 16.7% respectively.
Logistic multiple variable predictor model interaction of respiratory or non-respiratory status with air pollutant level (SO2) and humidity interactions
There was significant interaction between Respiratory/Non- Respiratory status, air pollution level (SO2) and humidity on day of admission and 30-day mortality outcomes. Although admission day level (SO2) and lower humidity levels linearly increased the risk of adverse 30-day mortality outcomes, at any given level of pollutant (quintile of SO2) of humidity category, the outcome for respiratory was worse compared with non-respiratory patients (Figure 2). For example, the predicted overall mortality at the highest quintile of SO2 Q5 with humidity>95% for non-respiratory and respiratory was 12.5% (95% CI: 11.0%, 14.1%) and 14.9% (95% CI: 13.2%, 16.5%) respectively but with very dry air (humidity<70%) mortality for the same quintile was much higher predicted non-respiratory and respiratory 16.1% (95% CI: 14.3%, 18.0%) and 18.8% (95% CI: 16.9%, 20.7%) respectively (Table 2, Figure 2).
Figure 2: The risk of a death by the 30-day of a hospital episode increased essentially as a linear function of to the underlying SO2 Quintile at the time of hospital admission. Model adjusted Humidity levels (>95% high;<70% low) predicted 30-day mortality outcomes. Lower admission humidity levels, at a given pollutant quintile, independently predicted worse outcomes with respiratory patients having worse outcomes.
Discussion
These data demonstrate that the level of humidity interacted with the prevailing level of SO2 air pollution to influence the outcome of an emergency medical admission. The predictive value was independent of Acute Illness Severity, Chronic Disabling Disease Score, Charlson Co-morbidity Index and Sepsis status. While mortality increased with increasing SO2 concentrations at all humidity levels; drier air predicted worse outcomes across the SO2 concentration quintile range. The SO2 cut-points were distribution determined with cut-points at 0.93, 1.54, 2.32 and 4.14 μg/m3 respectively; for humidity with a range of 50%-100%, we used mathematical cut-points of 50, 70, 85, and 95. But, as clearly demonstrated in Figure 1, increasing levels of SO2 at time of admission were associated with worse outcomes but the underlying level of humidity worsened such outcomes (Figure 2).
For example, at the third and fifth quintile of SO2, the predicted 30- day per patient mortality at a humidity level of>95% was predicted overall, irrespective of a respiratory or non-respiratory admission, at 11.2% and 12.4% but with lower humidity values between 50% and 70% would have risen to an estimated 14.2% and 16.7% respectively. For respiratory patients, these values would have been 12.8% and 14.2% for the former and 16.1% and 18.8% for the latter.
The results of this study are consistent with reports in the literature showing interactions between humidity and pollution driven morbidity and mortality. For example, studies have demonstrated an ameliorating effect of higher humidity on the impact of air pollution on chronic bronchitis and emergency COPD admissions [39]. Two large studies examining the effects of ambient particulate matter on mortality in 29 cities across Europe showed that the impact of pollution was higher in drier countries [40,41].
The impact of SO2 concentration on mortality outcomes was disproportionately exerted on patients with a respiratory presentation. A respiratory patient classification was a powerful predictor of mortality across the SO2 quintile range. These results are consistent with data from a large study examining mortality data from 38 large Chinese cities which showed that the impact of particulate air pollution on deaths from cardiorespiratory diseases was more than twice as high as the effects on other cause mortality [42].
SO2 is a known respiratory irritant and bronchoconstrictor, but its effects seem limited to patients with asthma and bronchitis, although sensitivity to exposure varies widely [43]. Exposure to SO2 gas has also been shown to modulate autonomic function. Work by Tunnicliffe and colleagues demonstrated changes in heart rate variability in humans associated with exposure to SO2 (200 ppb for 1 h) [44]. This data is supportive evidence for systemic effects of SO2 exposure resulting in downstream effects on other organ systems.
There is emerging evidence from the epidemiological literature of a protective effect conferred by higher humidity on the harmful effects of ambient air pollution on the airways. In fact, there are data that demonstrate the potential of ambient temperature and relative humidity to alter DNA methylation on genes related to coagulation, inflammation, cortisol, and metabolic pathways [45]. Within the lung, the relative humidity of inspired air must be approximately 95% for optimal alveolar and small airway function. Levels below 95% would result in excessive evaporation from mucosal surfaces and airway dehydration, and levels closer to 100% would risk droplets precipitation at lower temperatures [46]. Low environmental humidity values may therefore create problems in individuals with underlying airway disease or poor alveolar efficiency. More humid air may also help reduce the number of inorganic salt molecules in ambient aerosols when the level of solute deliquescence is surpassed [47].
As opposed to NO2 and various particulate pollutants, SO2 is a water soluble gas which could explain its susceptibility to the effects of ambient water vapour status as noted in this study. SO2 reacts with the mucus layer of the upper airways while more soluble gases such as NO2 are more likely to reach the alveoli [48]. SO2 may alter the production and/or composition of mucus of the upper airway with potential resultant effects on the ciliary epithelium. It is also possible that gases such as SO2 may affect airway sensory cells resulting in airway hyper reactivity and increased mucus secretion [48].
Our hospital catchment area is predominantly inner city, with over 50% of population classified as deprived [19]; 47 of the 74 Electoral Divisions (small local areas) categorised in the top quintile of the National Deprivation Index [49]. This deprived population of lower socioeconomic status (SES) may typically suffer from higher air pollution level exposure [50]. Lower SES has been also linked to different pulmonary diseases including COPD, asthma, COPD and pulmonary hypertension [51]. Presentations to our emergency services with a predominant respiratory disease component represent 19.5% of all emergency medical hospital episodes although they occur in only 9.6% of unique patients. This discrepancy in health care utilization is likely in part attributed to higher levels of motor traffic pollution. We previously described that in respect of respiratory admissions that SES influenced both the admission rate incidence and 30-day in-hospital mortality [52] and that air pollution on the day of admission influenced 30-day mortality outcomes [53].
This study was conducted in a single inner city centre and this may limit the generalizability of our results. Across the island of Ireland pollutant profiles might vary considerably from one area to another. Indeed legislation in place restricting the burning of soot producing fuel for home heating in Dublin City does not apply to rural areas. This may contribute to differences in particulate air pollution regionally. Variation in volatile organic compound concentrations in rural and urban may also be of significance in quantifying the humidity effect on health outcomes given that water vapour interacts with VOC’s to form harmful organic aerosols.
Conclusion
The data demonstrated an interaction between humidity and prevailing levels of SO2 air pollution in an inner city area with high levels of social deprivation and motor traffic congestion. The harmful effects of SO2 pollution were higher among patients presenting with respiratory disease than other presentations. Higher humidity levels favorably influenced the outcome of these emergency medical admissions across the SO2 ambient concentration range. The study was based on a large database of clinical data spanning a 16 year period. These results are supported by emerging epidemiological data linking humidity to reduction in pollution driven morbidity and mortality.
References
- Jiang XQ, Mei XD, Feng D (2016) Air pollution and chronic airway diseases: What should people know and do? J Thorac Dis 8: E31-E40.
- Faustini A, Stafoggia M, Colais P, Berti G, Bisanti L, et al. (2013) Air pollution and multiple acute respiratory outcomes. Eur Respir J 42: 304-313.
- Kelly FJ, Fussell JC (2011) Air pollution and airway disease. Clin Exp Allergy 41: 1059-1071.
- Karakatsani A, Analitis A, Perifanou D, Ayres JG, Harrison RM, et al. (2012) Particulate matter air pollution and respiratory symptoms in individuals having either asthma or chronic obstructive pulmonary disease: A European multicentre panel study. Environ Health 11: 75.
- Vineis P, Hoek G, Krzyzanowski M, Vigna-Taglianti F, Veglia F, et al. (2006) Air pollution and risk of lung cancer in a prospective study in Europe. Int J Cancer 119: 169-174.
- Sax SN, Zu K, Goodman JE (2013) Air pollution and lung cancer in Europe. Lancet Oncol 14: e439-e440.
- Scarborough P, Allender S, Rayner M, Goldacre M (2012) Contribution of climate and air pollution to variation in coronary heart disease mortality rates in England. PloS One 7: e32787.
- Gold DR, Samet JM (2013) Air pollution, climate, and heart disease. Circulation 128: e411-e414.
- Genc S, Zadeoglulari Z, Fuss SH, Genc K (2012) The adverse effects of air pollution on the nervous system. J Toxicol.
- Kaplan GG, Tanyingoh D, Dixon E, Johnson M, Wheeler AJ, et al. (2013) Ambient ozone concentrations and the risk of perforated and nonperforated appendicitis: A multicity case-crossover study. Environ Health Perspect 121: 939-943.
- Kelly I, Clancy L (1984) Mortality in a general hospital and urban air pollution. Ir Med J 77: 322-324.
- Clancy L, Goodman P, Sinclair H, Dockery DW (2002) Effect of air-pollution control on death rates in Dublin, Ireland: An intervention study. Lancet 360: 1210-1214.
- Barreca A (2012) Climate change, humidity, and mortality in the United States. J Environ Econ Manag 63: 19-34.
- Davis RE, McGregor GR, Enfield KB (2016) Humidity: A review and primer on atmospheric moisture and human health. Environ Res 144: 106-116.
- Tseng CM, Chen YT, Ou SM, Hsiao YH, Li SY, et al. (2013) The effect of cold temperature on increased exacerbation of chronic obstructive pulmonary disease: A nationwide study. PloS One 8: e57066.
- Eschenbacher WL, Moore TB, Lorenzen TJ, Weg JG, Gross KB (1992) Pulmonary responses of asthmatic and normal subjects to different temperature and humidity conditions in an environmental chamber. Lung 170: 51-62.
- Barreca A, Shimshack JP (2012) Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States. Am J Epidemiol 7: S114-S122.
- Makinen TM, Juvonen R, Jokelainen J, Harju TH, Peitso A, et al. (2009) Cold temperature and low humidity are associated with increased occurrence of respiratory tract infections. Respir Med 103: 456-462.
- Walsh JB, Coakley D, Murphy C, Coakley JD, Boyle E, et al. (2004) Demographic profile of the elderly population in Dublin accident and emergency hospital catchment areas. Ir Med J 97: 84-86.
- Rooney T, Moloney ED, Bennett K, O'Riordan D, Silke B (2008) Impact of an acute medical admission unit on hospital mortality: A 5-year prospective study. QJM 101: 457-465.
- Conway R, O'Riordan D, Silke B (2014) Long-term outcome of an AMAU--a decade's experience. QJM 107: 43-49.
- Beeknoo N, Jones R (2016) Factors influencing A & E attendance, admissions and waiting times at two London Hospitals. Br J Med Med Res 17: 1-29.
- O'Loughlin R, Allwright S, Barry J, Kelly A, Teljeur C (2005) Using HIPE data as a research and planning tool: limitations and opportunities. Ir J Med Sci 174: 40-45.
- O'Callaghan A, Colgan MP, McGuigan C, Smyth F, Haider N, et al. (2012) A critical evaluation of HIPE data. Ir Med J. 105: 21-3.
- Townsend P (1987) Deprivation. J Soc Policy 16: 25-46.
- Carstairs V, Morris R (1989) Deprivation and mortality: An alternative to social class? J Public Health 11: 210-219.
- Kelly A (2013) The National Deprivation Index for Health and Health Services Research-Update 2013. Small Area Health Research Unit, Department of Health and Primary Care: Trinity College Dublin.
- Shirmat M (1962) Algorithm 112: Position of point relative to polygon. ACM Comm 5: 434.
- Silke B, Kellett J, Rooney T, Bennett K, O’riordan D (2010) An improved medical admissions risk system using multivariable fractional polynomial logistic regression modelling. QJM 103: 23-32.
- O’Sullivan E, Callely E, O’riordan D, Bennett K, Silke B (2012) Predicting outcomes in emergency medical admissions – role of laboratory data and co-morbidity. Acute Med 2: 59-65.
- Courtney D, Conway R, Kavanagh J, O'riordan D, Silke B (2014) High-sensitivity troponin as an outcome predictor in acute medical admissions. Postgrad Med J 90: 311-316.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383.
- Chotirmall SH, Picardo S, Lyons J, D'alton M, O'riordan D (2014) Disabling disease codes predict worse outcomes for acute medical admissions. Intern Med J 44: 546-553.
- Cournane S, Conway R, Byrne D, O’Riordan D, Silke B (2017) Predicting outcomes in emergency medical admissions using a laboratory only nomogram. Comput Math Methods Med 1: 1-8.
- Keary J, Jennings SG, O’Connor TC, McManus B, Lee M (1998) PM10 concentration measurements in Dublin city. Environ Monit and Assess 52: 3-18.
- Froom P, Shimoni Z (2006) Prediction of hospital mortality rates by admission laboratory tests. Clin Chem 52: 325-328.
- Prytherch DR, Sirl JS, Schmidt P, Featherstone PI, Weaver PC, et al. (2005) The use of routine laboratory data to predict in-hospital death in medical admissions. Resusc 66: 203-207.
- Chotirmall SH, Callaly E, Lyons J, O’connell B, Kelleher M, et al. (2016) Blood cultures in emergency medical admissions: A key patient cohort. Eur J Emerg Med 23: 38-43.
- Qiu H, Yu IT, Wang X, Tian L, Tse LA, et al. (2013) Season and humidity dependence of the effects of air pollution on COPD hospitalizations in Hong Kong. Atmospheric Environ 76: 74-80.
- Aga E, Samoli E, Touloumi G, Anderson HR, Cadum E, et al. (2003) Short-term effects of ambient particles on mortality in the elderly: results from 28 cities in the APHEA2 project. Eur Respir J Suppl 40: 28s-33s.
- Katsouyanni K, Touloumi G, Samoli E, Gryparis A, Le Tertre A, et al. (2001) Confounding and effect modification in the short-term effects of ambient particles on total mortality: Results from 29 European cities within the APHEA2 project. Epidemiol 12: 521-531.
- Yin P, He G, Fan M, Chiu KY, Fan M, et al. (2017) Particulate air pollution and mortality in 38 of China's largest cities: time series analysis. BMJ 14: 356:j667.
- Kan H, Wong CM, Vichit-Vadakan N, Qian Z (2010) Short-term association between sulfur dioxide and daily mortality: the Public Health and Air Pollution in Asia (PAPA) study. Environ Res. 11: 258-664.
- Tunnicliffe WS, Hilton MF, Harrison RM, Ayres JG (2001) The effect of sulphur dioxide exposure on indices of heart rate variability in normal and asthmatic adults. Eur Respir J 17: 604-608.
- Bind M-A, Zanobetti A, Gasparrini A, Peters A, Coull B, et al. (2014) Effects of temperature and relative humidity on DNA methylation. Epidemiology 25: 561-569.
- Bind M-A, Zanobetti A, Gasparrini A, Peters A, Coull B, et al. (2014) Effects of temperature and relative humidity on DNA methylation. Epidemiology 25: 561-569.
- Negus VE (1952) Humidification of the air passages. Acta Oto-Laryngologica 41: 74-83.
- Kunzli N, Perez L, Rapp R (2010) Air quality and health. Eur Respir Soc.
- Kelly A, Teljeur C (2007) SAHRU National Deprivation Index Trinity College, Dublin.
- Leitte AM, Petrescu C, Franck U, Richter M, Suciu O, et al. (2009) Respiratory health, effects of ambient air pollution and its modification by air humidity in Drobeta-Turnu Severin, Romania. Sci Total Environ 407: 4004-4011.
- Havard S, Deguen S, Zmirou-Navier D, Schillinger C, Bard D (2009) Traffic-related air pollution and socioeconomic status. Epidemiology 20: 223-230.
- Sahni S, Talwar A, Khanijo S, Talwar A (2017) Socioeconomic status and its relationship to chronic respiratory disease. Adv Respir Med 85: 97-108.
- Cournane S, Byrne D, Conway R, O'Riordan D, Coveney S, et al. (2017) Effect of social deprivation on the admission rate and outcomes of adult respiratory emergency admissions. Respir Med 125: 94-101.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi