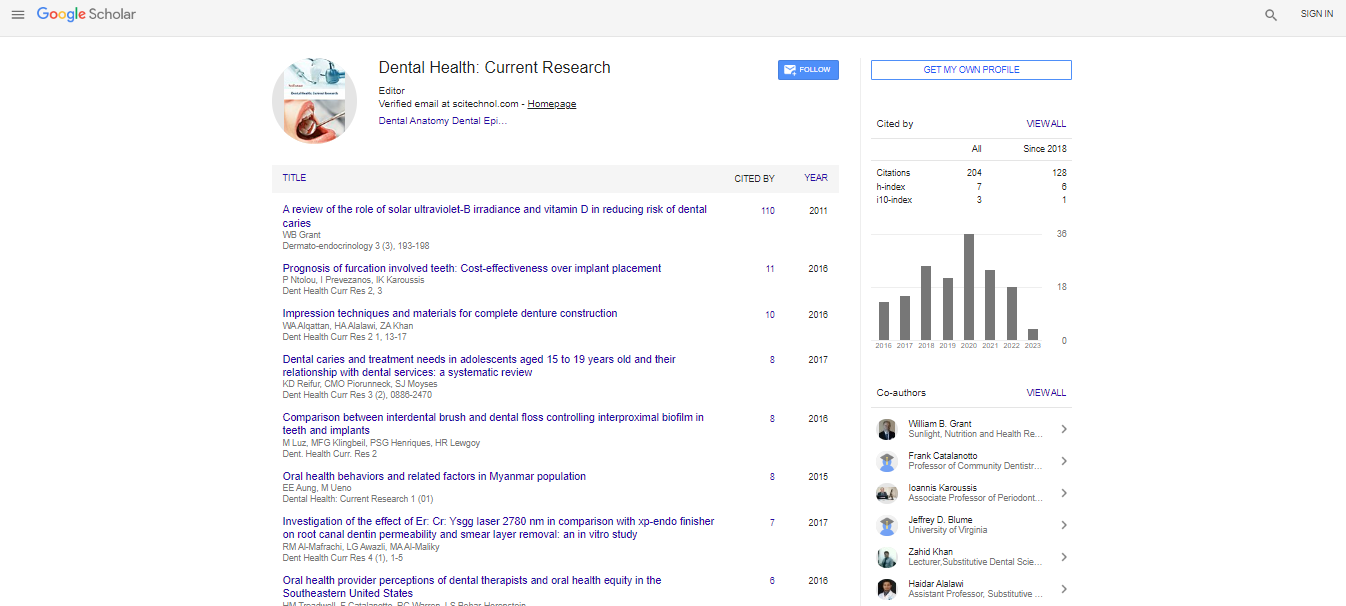
Research Article, Dent Health Curr Res Vol: 5 Issue: 1
The Internal Sinus Floor Elevation Procedure is Comparable to the Conventional Sinus Floor Elevation Procedure in Highly Atrophic Alveolar Ridges: Results Four Years after Loading in A Randomized, Controlled, Blind Pilot Study
Peter Schleier1*, Hauk Øyri2 and Jörg Törpel3
1Department of oral surgery, Helse Stavanger HF, Armauer Hansens vei, Norway
2Department of Oral Surgery and Oral Medicine, Institute of Clinical Dentistry, University of Oslo, Norway
3ENT Department, Helse Stavanger HF, Armauer Hansens vei, Norway
*Corresponding Author : Peter Schleier
Department of oral surgery, Helse Stavanger HF, Armauer Hansens vei 20, 4011 Stavanger, Norway
Tel: +0047-90893756
E-mail: Schleier@online.no
Received: September 9, 2018 Accepted: October 12, 2018 Published: October 17, 2018
Citation: Schleier P, Øyri H, Törpel J (2018) The Internal Sinus Floor Elevation Procedure is Comparable to the Conventional Sinus Floor Elevation Procedure in Highly Atrophic Alveolar Ridges: Results Four Years after Loading in A Randomized, Controlled, Blind Pilot Study. Dent Health Curr Res 7:3. doi: 10.4172/2470-0886.1000139
Abstract
To investigate whether endoscopically assisted internal sinus
floor elevation (EIS) is as good as the conventional open
surgical method (CSE) in terms of sufficient bone support for
the placement of dental implants and long-term implant
success. A split mouth model whereby 20 dental implants were
installed in 10 patients (five female and five male) following EIS
or CSE. No graft materials were used, only locally harvested
autogenous bone. Both surgical procedures were monitored
endoscopically at the time of implant placement and upon
placement of the healing abutment (three months). Panoramic
radiographs were made pre- and postoperative, and after 36
months in order to evaluate peri-implant bone. The average
preoperative maxillary alveolar bone height at the implant site
(first molar) was 4 mm. The average gain in bone height was 6
mm using EIS and 5.5 mm with CSE respectively. Clinical
parameters revealed sufficient implant stability at the time of
placement. Three implants failed during the healing period of
12 weeks. The overall implant success rate was 85 percent.
The overall success rate at the time of implant loading was 100
percent. After loading, no further implant failure was observed
over a four year period. Sinus floor elevation is a wellestablished
procedure for augmentation of the atrophic
maxillary posterior region. Our results indicate that EIS is at
least as good as CSE. Endoscopically assisted surgery helped
prevent, diagnose, and manage sinus membrane perforations.
After 48 months of loading, the clinical outcomes of the present
study showed that EIS and simultaneous implant placement
resulted in low intraoperative trauma, sufficient implant stability
upon placement, low incidence of postoperative symptoms,
and a high success rate.
Keywords: Implantology; Bone augmentation; Sinus floor elevation; Bone height, Endoscope
Abbreviations
EIS: Endoscopically Assisted Internal Sinus Floor Elevation; CSE: Conventional Open Sinus Floor Elevation
Introduction
Prosthetic rehabilitation of edentulous patients with dental implants is a well-established and reliable mode of treatment. Availability of bone with sufficient quantity and quality for dental implant placement is an important factor for the implant surgeon. As a consequence of alveolar ridge atrophy after tooth loss and the inferior extension of the maxillary sinus, the bone volume available in the maxilla premolar and molar region may be insufficient for insertion of dental implants with the necessary diameter and length [1]. Patients with severe atrophy of alveolar bone may require surgical intervention in the form of bone augmentation and/or sinus lift procedures, prior to or in conjunction with implant insertion, for a successful implant treatment outcome [2]. Shorter implants have successfully been used in cases with reduced alveolar bone height [3]. Consequently, at least one paper recommends placement of implants of at least 10 mm in length for situations with low bone quality [4]. The two main methods for accessing the maxillary sinus cavity to elevate the Schneiderian membrane are: [5] The lateral approach, conventional sinus floor elevation (CSE), the most well-known procedure despite being invasive, complicated, and long-lasting, [6] and the osteotome sinus floor elevation which was first introduced by Tatum. [7] It was originally performed with a special instrument known as a “socket former”, which was used to infracture the sinus floor and move it in a cranial direction. Later, another transalveolar technique, the bone-added osteotome sinus floor elevation, was described by Summers [8]. Osteotome sinus floor elevation is less invasive, traumatic, and time-consuming than the lateral approach [9]. Preoperative, interdisciplinary investigation and selection of patients planned to undergo CSE procedures, especially in highly atrophic cases, should be a matter of routine even if normal clinic operations are different [10]. Despite the successful use of the internal sinus lift method reported in Kfir et al. [11], the blind nature of this procedure prevents the surgeon from identifying sinus membrane tears. This may have an influence on whether an implant should be placed at the site at the time of sinus elevation or whether a two-step procedure should be used. Furthermore, the visual control when elevating the sinus floor (CSE) allows for the use of longer implants when simultaneous placement is feasible. The use of CSE combined with implant placement in cases with high atrophic maxillary bone is an established surgical procedure. On the other hand, evidence suggests that visual control of the internal sinus lift method could deliver advantages. EIS reduces the risk of perforation and increases indication for the method [12]. To the best of our knowledge, there are no data available comparing EIS and CSE in patients with severe alveolar ridge atrophy. The primary aim of this study is to investigate whether the EIS method is as good as CSE with regard to sufficient bone support for the placement of dental implants and long-term implant success in a split mouth model in 10 patients with severe atrophy of the posterior maxillary alveolar ridge (<5 mm residual bone height).
Materials and Methods
A randomized, controlled, blind trial was performed. All patients were planned to receive a primary stable implant bilaterally in the maxilla in conjunction with elevation of the sinus membrane without using bone grafts or artificial bone substitutes. By simple coin toss, one site was chosen for CSE while EIS was performed simultaneously at the other site. Both surgical procedures were endoscopically assisted. The study was approved by the Regional Committee for Medical and Health Research Ethics (REK Sør-Øst/2010/2243/REK). All patients gave their written consent to participate in the study.
Inclusion criteria
Patients above 18 years of age needing at least one implant in the molar region on each side were required. Bone height had to be <6mm bone height and alveolar ridge width at least 5mm width at the potential implant site.
All participants had to be classified as ASA 1-3, fit enough to be undergoing oral surgery, [13] and exhibit good oral hygiene. Periapical and periodontal infections were eliminated at least three months prior to enrolling in the study. All restorative and pre-prosthetic treatment was completed prior to implant surgery as part of a comprehensive treatment plan for dental rehabilitation following tooth loss.
Exclusion criteria
Patients were excluded from the study where bone height at the prospective implant area was more than 6 mm or less than 2 mm, and where alveolar ridge width was less than 5 mm.
Further exclusion criteria were:
1. Chemotherapy for the treatment of malignant tumors at any point during the three months prior to surgery.
2. Bone deficiencies as a result of chronic infections.
3. Systematic use of steroids and or bone modulating medications (bisphosphonates).
4. Untreated, serious renal and hepatic diseases.
5. Psychological or neurological illness.
6. Poor oral hygiene or non-compliance with previous medical or dental treatments.
Preoperative diagnostics
The preoperative diagnostics included a full medical and dental history and clinical assessment. As for clinical evaluation of the potential surgical sites, the following parameters were evaluated: Mucosal resilience and bone volume/quantity at the proposed implant sites (from static, functional, and aesthetic points of view), as well as the thickness and extent of keratinized tissue at these sites. Study models were used to fabricate diagnostic wax-ups in order to illustrate to the dentist and patient the final outcome of the prosthetic therapy. This also helped when determining the most prosthetically favorable implant position. Additionally, the diagnostic wax-up served as a template when preparing an individual surgical guide for each case, through which the planned implant position (location and angulation) could be clearly ascertained for intraoperative use at the time of osteotomy.
Preoperative radiographs
For each case, a panoramic radiograph with a 5 mm metal ball in the planned implant position, fixed in an individual plastic guide, was made (Oralix Multiscan CEPH by Gendex, Hamburg, Germany). This enabled a comprehensive evaluation of the bone volume and the exclusion of pathological conditions of the bone and surrounding areas such as maxillary sinusitis, osteomyelitis, cysts, and tumors. The bone volume was evaluated by applying the rule of three described by Schleier et al. 2008 [14]. In instances where radiological findings in the conventional radiographs were uncertain, computer tomography scanning (CT) was performed (required for 50 percent of patients in this study). Cross-sectional, three-dimensional, panoramic digital images were generated from the original CT data to evaluate pathology in the maxilla and paranasal sinuses. CT scans were carried out at the Department of Radiology, Stavanger University Hospital, Stavanger, Norway, using a Siemens Somatom Plus 4 (Siemens Healthcare GmbH, Erlangen, Germany).
Surgical technique
All patients were given a preoperative mouth rinse with 0.2 percent chlorhexidine (Corsodyl 2 mg/ml, GlaxoSmithKline, Oslo, Norway) for two minutes, supervised by the study nurse. Regional anesthesia of the infraorbital and palatal nerves was carried out using Xylocaine 2% with epinephrine (Xylocaine Dental Adrenaline, Dentsply Ltd, Surrey, England). In addition, local infiltration with 3 ml of Articaine (Septocaine Dental Adrenaline, Dentsply Ltd, Surrey, England) in the vestibule was added.
CSE procedure: A midline alveolar crest incision with medial and distal release incisions were made with a number 15 blade. Soft tissue overlying the crest of the alveolar ridge was elevated at the implantation site [15]. Elevation was extended from the canine fossa to zygomatic alveolar crest. The osteotomy sites were marked along with the site of implant placement using the surgical guide and a low speed (800 RPM) round carbide bur. The lateral window was outlined and prepared 3 mm above the alveolar ridge with a surgical hand piece (W&H Dentalwerk, Bürmoos, Austria) and round carbide bur (1600 RPM) while maintaining continued cooling with physiological NaCl solution (50 ml/min). Careful elevation of the bony window cranially and the attached sinus membrane 6–10mm was then performed. In a second step, the endoscopy was carried out by perforating the thin bone in the canine fossa with a trocar. The endoscope was inserted through a guiding tube. A 2.9 mm sinuscope with 70-degree view and digital camera head (Karl Storz, Tuttlingen, Germany) was used. A complete functional sinuscopy was carried out, including video documentation of the osteomeatal complex and observation of the elevation site. Implant placement was then carried out under endoscopic control of the sinus membrane as described by Schleier et al. 2008. After successful placement of a primary stable implant, the mucoperiosteal flap was readapted and sutured with the help of 4-0 Vicryl (Ethicon, Sommerville, USA).
EIS procedure: This procedure has been described earlier (Schleier et al. 2008). Anesthesia, mid-line alveolar crest incisions, and elevation of the implantation site were performed in exactly the same way as the CSE procedure. Following that, a 5 mm long stab incision of the mucosa approximately 5 mm cranial to the apex of the canine tooth (fossa canina) was made for endoscopy of the paranasal sinus as outlined above. The implant osteotomy was prepared with a maximum speed of 300 rpm carried out with continued cooling through physiological NaCl solution (50 ml/min) to approximately 1 mm before the sinus membrane. After fracturing the cortical bone of the sinus floor with a rounded, tapered osteotome (Karl Storz, Tuttlingen, Germany), the maxillary sinus membrane was elevated to reach a total implant osteotomy height of 8–12 mm. This elevation was carried out while the operator was viewing from the superior aspect of the sinus membrane with the endoscope. Afterwards, implant placement was also carried out under visual control by endoscope.
Postoperative clinical evaluation
For all patients, clinical assessments were carried out one week, six weeks, and three months after surgery and a further six, 12, 30, 36, and 48 months after loading. Sutures were removed and clinical assessments carried out during the first postoperative examination. Subjective patient complaints, postoperative swelling, sensation disturbances, and pathological conditions such as fistula formation were noted. Special attention was given to the peri-implant soft tissue.
The following particular assessments were made:
subjective pain assessment (0=no pain, 1=pain)
assessment of the peri-implant soft tissue situation (level I=free of inflammation, II=moderate inflammation, III=acute inflammation)
assessment of sensation of the intraoral mucous membrane and corresponding facial skin (two-point discrimination test)
Postoperative radiographs
In order to assess implant position and the implant’s relation to neighboring structures, a panoramic radiograph was carried out immediately after the sinus elevation and implant placement. A second panoramic, radiographic assessment along with periapical radiographs were made during the fifth control session (one year after functional loading) as part of a comprehensive evaluation.
Abutment Surgery and Second Sinuscopy/Prosthetic Treatment
Approximately three months after implant placement, abutments were inserted during the control procedure using sinuscopy as outlined above. Video data from the endoscopy were collected using the Storz system (Karl Storz, Tuttlingen, Germany).
Two weeks after placement of healing abutments, the patients started prosthetic rehabilitation and subsequent loading of the implants. Screw-retained abutments were used. Clinical and radiological assessments took place during the fifth and sixth recall sessions. The following parameters were measured and assessed:
1. integrity and stability of the prosthesis on the implant(s)
(0=prosthesis lacks structural integrity; 1=prosthesis intact)
2. quality of the restoration edge at the interface with implant
3. nature of static and dynamic occlusion
4. absence of proximal contacts
5. periodontal status (probing depth in mm; bleeding when probing 0=no bleeding, 1=bleeding)
6. subjective patient satisfaction (1=satisfied, 2=dissatisfied)
The survey of all criteria was made by the examiner with the use of suitable aids (dental explorer, periodontal probe, occlusal foils, dental floss, etc.). The “subjective patient satisfaction” results were attained through conversation with the patient.
Statistical Comparisons
Implants installed through EIS were compared to implants installed through CSE. Differences in implant function and the number of severe perforations between the conventional and internal methods were evaluated utilizing McNemar’s test. Confidence intervals for differences between paired proportions were calculated using an exact method through the “ExactCIdiff” package in R. We employed box plots to visualize the effect of bone height on implant function and perforations. SPSS (version 22.0, IBM Corp., Armonk, NY) was used for all analyses if not otherwise stated. The significance level was set at five percent.
Results
From November 2011 to March 2013, a total of 10 patients (five female and five male) aged 43 to 78 (average age: 64) were enrolled in the present study.
The preoperative panoramic radiographs demonstrated that there were two minor pathological findings in the maxillary sinuses not related to the surgical sites (attested by CT scan). No signs of infection, tumors, or cysts were found. For all sites, pre-surgical bone height averaged 3.8 mm. For the right side, the range was 2–6 mm (mean of 3.3 mm) and, on the left, the range was 3–6 mm (mean of 4.2 mm). The following implants were used:
SP RN implants (Straumann, Basel, Switzerland) in 8, 10 and 12 mm lengths with a diameter of 4.1 mm
TE RN implants (Straumann, Basel, Switzerland) in 8, 10 and 12 mm lengths with a diameter of 4.1 mm
Intraoperative
Twenty primary stable implants were successfully placed in 10 patients. We observed perforations (sizes ranging from 1.2–5.0 mm) of the Schneiderian membrane in five patients. Two perforations were observed during EIS and three during CSE. The simultaneously placed implants were fully covered by mucosa in all implant sites. In two cases (CSE) we observed minor complications, such as bleeding, reducing the clear view from the endoscope.
17 of the 20 implants integrated successfully. We lost three implants, all on the right side (two could be replaced successfully during abutment surgery). This corresponds to a success rate of 85 percent. No further implant loss was observed after prosthetic loading. At the first postoperative evaluation (one week after surgery), one patient had a mucosal swelling on the right side (EIS), while a second patient showed signs of inflammation around the surgical site on the left (CSE). The mucosa surrounding the implant in the second patient was red and swollen. Both patients responded well to systemic antibiotic therapy with clindamycin (Dalacin 300 mg qid) for one week. Due to implant mobility in the second patient, we had to remove the implant after three weeks. Successful re-implantation was accomplished during abutment insertion and the second sinuscopy (three months afterprimary surgery). The postoperative radiographs, one week after surgery, showed a liquid level in the sinus in three patients: Two on the right side (CSE) and one on the left (EIS). The average sinus membrane elevation was 6.7 mm (range 5–9 mm). Mean sinus floor elevation on the right side was 6.3 mm (ranging from 6 mm to a maximum of 9 mm) and 6.7 mm (ranging from 5 mm to 8 mm) on the left side was observed. All radiographs demonstrated the positioning of the implants at the locations planned prosthetically.
Abutment Insertion/Second Endoscopy–Three Months after Implant Placement
Endoscopic evaluation did not reveal any pathological findings around the implants or in the maxillary sinus floor in eight patients. The apices of all 18 implants were completely covered by healthy sinus mucosa (Figure 1). One patient (CSE) had peri-implant inflammation and slight movement of the implant, but no signs of intrasinusal inflammation. The implant was subsequently removed. The implant was later replaced using the EIS method. Furthermore, the patient who underwent early implant removal (three weeks after primary surgery) received an implant in accordance with the EIS procedure as described above.
Another implant was removed in a different patient due to complete resorption of tissue around the intrasinusal portion of the implant and luxation of the implant from its original position. The patient chose conventional prosthetic rehabilitation of the missing tooth.
Clinical and Radiological Analyses Two, Three and Four Years after Functional Loading
All prosthetic constructions attached to the implants were in a fully functional state. No major bone loss, pockets, or infections around the implants were observed. All prosthetic implant-borne reconstructions were in a fully functional state. The patients expressed complete satisfaction with the functional results.
None of the clinical findings showed any major changes between the three-month and final recall exams with regard to implant stability and peri-implant soft tissue structures, except for one patient who showed bleeding during peri-implant probing at the right side (CSE). The patient was referred to periodontics for professional cleaning and hygiene instruction. In addition, there were no peri-implant pathologic changes noted in the radiographs. The comparison of bone height measurements (marginal bone level–apical bone level of elevated bone fragment) between post-surgery and 36 months after implant loading showed an average difference of 2 mm (minimum 0.2 mm and maximum 2.4 mm). We lost one patient three years after successful implant surgery and prosthetic rehabilitation due to liver cancer.
Results of the Statistical Evaluation
For the conventional method, the results showed that only patients with very low jaw heights (2–3 mm) have experienced severe perforations (Figure 2). The only individual not to have a functioning implant after one year had the minimum jaw height value of 2 mm (Figure 1).
McNemar’s test showed no significant differences between the two groups in any case (Tables 1 and 2), though confidence intervals were very wide (-0.48811, 0.29665).
| Conventional | Internal | p | Diff prop (95% CI) | |
|---|---|---|---|---|
| Non-Severe | Severe | |||
| Non-severe | 7 | 1 | 1.000 | -0.1 (-0.5, 0.3) |
| Severe | 2 | 0 | ||
Table 1: Effect of Operation Type on the Development of a Severe Perforation (The p-value is derived from McNemar’s test of group differences).
| Conventional | Internal | P | CI | |
|---|---|---|---|---|
| No | Yes | |||
| No | 0 | 1 | 1.000 | -0.1 (-0.5, 0.3) |
| Yes | 2 | 7 | ||
Table 2: Effect of Operation Type on the Success of Implant After One Year (The p-value is derived from McNemar’s test of group differences).
Discussion
The aim of this study is to evaluate if either CSE or EIS are superior for creating sufficient bone in simultaneous implant placement. Selection of ideal, severely atrophic maxilla patients with less than 6 mm bone height in the maxilla on both sides enabled the comparison of CSE and EIS in the same individual under almost equal conditions in terms of clinical outcome over more than three years.
The split mouth model is frequently used in clinical trials, and especially in studies with a focus on investigating the outcome of different sinus augmentation procedures. The anatomical requirement makes the model superior to a study design with single side treatment [16]. Several factors, such as the extent of remaining bone height and width in the implant area, remaining dentition, oral hygiene, smoking, and quality of the remaining alveolar bone, may influence the healing process and clinical outcome [17]. The evaluated methods for sinus floor augmentation are popular and accepted in modern invasive dentistry, especially in cases with more than 6 mm remaining alveolar crest [18]. In the present study, no significant difference was observed in either of the groups, however the success rate was clearly lower than implant treatment in patients with sufficient bone at the implant site [19]. One study, published in 2000, described a comparison of endoscope-guided internal sinus floor elevation with the direct lateral window sinus floor augmentation procedure [20]. This earlier report stated that 132 implants were placed in 62 clinically healthy patients. The residual height of the alveolar crest in the implant site was more than 6 mm on average. Internal sinus floor elevation with endoscopically guided surgery was chosen on 18 occasions. There were maxillary sinus opacities evident in panoramic radiographs at 40 of the 45 lateral window sinus augmentation sites one week after surgery. While the implant success for both methods six months after operation was 95%, the authors attributed these early negative outcomes to hematoma formation and sinus mucosa swelling. The advantages of CSE are the high certainty of clinical success and good visual control of the region being augmented. [21] Sinus lift procedures depend greatly on fragile structures and anatomical variations. The maxillary sinus has an anatomical form that varies very strongly from individual to individual and includes septa and bone cavities. The size, septum thickness, and structure of the bones forming the maxillary sinus are also highly variable. In particular, basal septa in the alveolar recess present the surgeon with problems during conventional sinus elevation owing to the risk of tearing the thin membrane. This increases the risk of complications such as bleeding, infection, and so on, and also determines the surgical approach used. Conditions such as sinus floor convolutions, sinus septum, transient mucosa swelling and narrow sinus structures, especially in the area of recessus alveolaris may contraindicate CSE. Absolute contraindications are maxillary sinus diseases such as tumors and chronic inflammation. The sinus is covered by the Schneiderian membrane, which is usually thin and easily penetrable with rotating or sharp instruments or even implants during insertion [22]. If the perforation is too large, and residual bone height low, the success rate will decrease and complications, such as sinus inflammation and finally loss of implant stability, can easily be the result.[23] The internal sinus lift with the use of graft material is described as an established procedure in oral implantology. [24] Various authors have provided guidelines for this procedure, most finding a residual bone height between 5 – 9 mm preferable [25]. Commonly accepted dimensions for dental implants used in the posterior maxilla through osteotomy sites while achieving primary stability should be approximately 4 mm in diameter and at least 10 mm in length. The preoperative residual alveolar ridge should be at least 5 mm wide and at least 6 mm high [26]. If the available bone height and width is lower, the surgeon may choose a lateral window approach with or without placement of graft material and possibly lateral augmentation and implant insertion at a later stage [27]. The success rate for lateral window sinus elevation techniques has been reported at between 85 and 97 percent [28]. The success rate for the internal sinus lift procedures hovers around 90 percent depending on the residual bone height, technique, observation time, and existence or absence of sinus [29].
The combination of an established diagnostic method for maxillary sinus (endoscopy) and minimally invasive transcrestal sinus floor elevation seems to increase indications for and can reduce complications of the minimally invasive procedure and implant placement [30]. Reduction in the number of perforations can easily be explained by the possibility of intraoperative visual guidance and control provided by the endoscope. The decrease in complications is the result of being able to inspect the sinus before elevating the Schneiderian membrane. The control of other important physiologically structures like the osteomeatal complex may contribute to an undisturbed healing process [31]. There is no doubt about the risk of treatment in cases with high atrophic alveolar crest being considerably higher than in cases with sufficient bone supply. The former leads to proportionally more complications such as loss of implants, sinusitis, and infections [32]. We have also observed in our study a higher complication rate when it comes to successful implantation in situations with proper bone. However, there were no significant differences in the method used and time of occurrence. All failed implants were observed at an early stage. The increased risk of early implant loss while expanding indications is known and an ethical dilemma for the surgeon [33]. On the other hand, if the implant survived the first three month period after insertion, there were no other problems or complications that were later observed. This observation is supported by the outcomes of other clinical trials examining the same topic [34]. The advantages of the EIS procedure observed in our study, such as reduced/short operation time, no donor site morbidity, no serious complications in even expanded indications, and long-term stability in terms of functional loading, are generally accepted and published in earlier trials, though with an initial bone amount at the implant site that was clearly larger [35]. Forgoing bone substitutes is discussed very frequently in literature [36]. Benefits like the short healing period, possibility of early implant loading, decreased treatment cost, no allergic reaction, and no risk of complications while dislocating bone substitutes in the sinus are mentioned [37].
Expanded indication of EIS/CSE without additional bone grafting/ bone substitutes in situations with less than 6 mm bone in the molar region is common, demands from patients are increasing, and the technical possibilities are increasing too. On the other hand, challenges with the method include practical excitement, technical sensitivity and the requisite experience for performing surgery and choosing the correct indication [38,39]. In this clinical trial, we observed that, after a three month healing period, no other implants were lost during the almost four year follow-up period. According to literature, the survival rate of implants after CSE is between 91 and 95 percent [40]. Failure rates increase when the amount of original bone is less than 6 mm. We found that an average alveolar crest bone height of 4 mm and width of at least 5 mm was sufficient to achieve and maintain implant stability and success in more than 80 percent of treatment sites. Although the sample size of the current study is not very large, a difference between the two methods could not be established. The sample size is also too small to make solid conclusions from the data. The range of jaw heights is, by chance, smaller in the internal group than in the conventional group (Table 3). In addition, the internal group has no jaws with <3 mm height (Table 4). Although there is no guarantee that these relationships coincide with the population as a whole, we cannot ignore these trends and they should be considered in future studies comparing both methods.
| Conventional jaw height (mm) | Internal jaw height (mm) | |
|---|---|---|
| N | 10 | 10 |
| Mean | 3.6 | 3.9 |
| Median | 3.0 | 4.0 |
| Standard deviation | 1.350 | .876 |
| Variance | 1.822 | .767 |
| Minimum | 2 | 3 |
| Maximum | 6 | 6 |
Table 3: Descriptive Statistics of Jaw Height for Each Method of Sinus Lift.
| Group | Height | Frequency | Percentage |
|---|---|---|---|
| Conventional | 2 | 2 | 20 |
| 3 | 4 | 40 | |
| 4 | 1 | 10 | |
| 5 | 2 | 20 | |
| 6 | 1 | 10 | |
| Total | 10 | 100 | |
| Internal | 3 | 3 | 30 |
| 4 | 6 | 60 | |
| 6 | 1 | 10 | |
| Total | 10 | 100 |
Table 4: Frequency of Jaw Heights for Each Method of Sinus Lift.
References
- Carlsson GE (2014) Implant and root supported overdentures - a literature review and some data on bone loss in edentulous jaws. J Adv Prosthodont 6: 245-252.
- Asawa N, Bulbule N, Kakade D, Shah R (2015) Angulated implants: an alternative to bone augmentation and sinus lift procedure: systematic review. J Clin Diagn Res 9: 10-13.
- Geckili O, Bilhan H, Geckili E, Cilingir A, Mumcu E, Bural C (2014) Evaluation of possible prognostic factors for the success, survival, and failure of dental implants. Implant Dent 23: 44-50.
- Schwartz-Arad D, Kidron N, Dolev E (2005) A long-term study of implants supporting overdentures as a model for implant success. J Periodontol 76: 1431-1435.
- Aritza B, Nerea M, Fernández-Gonzalez FJ, Larrazábal C, Anta A (2014) Osteotome sinus floor elevation without grafting material: Results of a 2-year prospective study. J Clin Exp Dent 6: 479-484.
- Fugazzotto P (2003) Augmentation of the posterior maxilla: a proposed hierarchy of treatment selection. J Periodontol 74: 1682-1691.
- Tatum H (1986) Maxillary and sinus implant reconstructions. Dental Clinics of North America 30:207-22.
- Summers, R.B (1994) A new concept in maxillar implant surgery: The osteome technique. Compendium of continuing education in dentistry 21: 152-162.
- Chen L, Cha J (2005) An 8-year retrospective study: 1,100 patients receiving 1557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol 76: 482-491.
- Torretta S, Mantovani M, Testori T, Cappadona M, Pignataro L (2013) Importance of ENT assessment in stratifying candidates for sinus floor elevation: a prospective clinical study. Clin Oral Implants Res 24: 57-62.
- Kfir E, Kfir V, Mijiritsky E, Rafaelof R., Kaluski E (2006) Minimally invasive antral membrane balloon elevation followed by maxillary bone augmentation and implant fixation. J Oral Implantol 32: 26-33.
- Matern JF, Keller P, Carvalho J, Dillenseger JP, Veillon F, Bridonneau T (2015) Radiological sinus lift: a new minimally invasive CT-guided procedure for maxillary sinus floor elevation in implant dentistry. Clin Oral Implants Res 13: 126-131.
- Silvestre FJ, Miralles-Jorda L, Tamarit C, Gascon R (2002) Dental management of the patient with ischemic heart disease: an update. Med Oral 21: 222-230.
- Schleier P, Bierfreund G, Schultze-Mosgau S, Moldenhauer F, Küpper H, Freilich M (2008) Simultaneous dental implant placement and endoscope-guided internal sinus floor elevation: 2-year post-loading outcomes. Clin Oral Implants Res 19: 1163-1170.
- Gomez-Roman G (2000) Influence of flap design on peri-implant interproximal crestal bone loss around single-tooth implants. Int J Oral Maxillofac Implants 116: 61-67.
- Baldini N, D'Elia C, Bianco A, Goracci C, de Sanctis M, et al. (2016) Lateral approach for sinus floor elevation: large versus small bone window - a split-mouth randomized clinical trial. Clin Oral Implants Res 5: 10-11.
- Mohan N, Wolf J, Dym H (2014) Maxillary sinus augmentation. Dent Clin North Am 59: 375-388.
- Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, et al. (2010) Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol 3: 7-26.
- Moy PK, Nishimura GH, Pozzi A, Danda AK (2016) Single implants in dorsal areas - A systematic review. Eur J Oral Implantol 9: 163-172.
- Wiltfang J, Merten HA, Kessler P, Ludwig A, Engelke W (2000) Endoscopic and ultrasonographic evaluation of the maxillary sinus after combined sinus floor augmentation and implant insertion. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 89: 288-291.
- Schwarz L, Schiebel V, Hof M, Ulm C, Watzek G, Pommer BJ (2015) Risk Factors of Membrane Perforation and Postoperative Complications in Sinus Floor Elevation Surgery: Review of 407 Augmentation Procedures. Oral Maxillofac Surg 12: 278-281.
- van den Bergh JP, Bruggenkate CM, Disch FJ, Tuinzing DB (2000) Anatomical aspects of sinus floor elevations. Clin Oral Implants Res 11: 256-265.
- Clementini M, Ottria L, Pandolfi C, Bollero P (2013) A novel technique to close large perforation of sinus membrane. Oral Implantol 6: 11-14.
- Uckan S, Tamer Y, Deniz K (2011) Survival rates of implants inserted in the maxillary sinus area by internal or external approach. Implant Dent 20: 476-479.
- Kim JM, Sohn DS, Bae MS, Moon JW, Lee JH, et al. (2014) Flapless transcrestal sinus augmentation using hydrodynamic piezoelectric internal sinus elevation with autologous concentrated growth factors alone. Implant Dent 23:168-74
- Boffano P, Forouzanfar T (2014) Current concepts on complications associated with sinus augmentation procedures. J Craniofac Surg 25: 210-2.
- Stern A, Green J (2012) Sinus lift procedures: an overview of current techniques. Dent Clin North Am 56: 219-233.
- Caudry S, Landzberg M (2013) Lateral window sinus elevation technique: managing challenges and complications. J Can Dent Assoc 79: 101.
- Pjetursson BE, Lang NP (2000) Sinus floor elevation utilizing the transalveolar approach. Periodonto 66: 59-71.
- Garbacea A, Lozada JL, Church CA, Al-Ardah AJ, Seiberling KA, et al. (2012) The incidence of maxillary sinus membrane perforation during endoscopically assessed crestal sinus floor elevation: a pilot study. J Oral Implantol 38: 345-359.
- Felisati G, Borloni R, Chiapasco M, Lozza P, Casentini P, et al. (2010) Maxillary sinus elevation in conjunction with transnasal endoscopic treatment of rhino-sinusal pathoses: preliminary results on 10 consecutively treated patients. Acta Otorhinolaryngol Ital 30: 289-293.
- Lee JW, Yoo JY, Paek SJ, Park WJ, Choi EJ (2016) Correlations between anatomic variations of maxillary sinus ostium and postoperative complication after sinus lifting. J Korean Assoc Oral Maxillofac Surg 42: 278-283.
- Kim YK, Hwang JY, Yun PY (2013) Relationship between prognosis of dental implants and maxillary sinusitis associated with the sinus elevation procedure. Int J Oral Maxillofac Implants 28: 178-183.
- Stefanski S, Svensson B, Thor A (2016) Implant survival following sinus membrane elevation without grafting and immediate implant installation with a one-stage technique: an up-to-40-month evaluation. Clin Oral Implants Res 20: 1111-12993.
- Nahlieli O, Zagury A, Michaeli E, Bruck N, Nahlieli DD, et al. (2016) Four-years' experience with dynamic implants with internal port for minimally invasive sinus elevation. Quintessence Int 47: 669-675.
- Artzi Z, Parson A, Nemcovsky CE (2003) Wide-diameter implant placement and internal sinus membrane elevation in the immediate postextraction phase: clinical and radiographic observations in 12 consecutive molar sites. International Journal of Oral & Maxillofacial Implants 18: 242-249.
- Kim YH, Choi NR, Kim YD (2017) The factors that influence postoperative stability of the dental implants in posterior edentulous maxilla. Maxillofac Plast Reconstr Surg 39: 86-90.
- Cara-Fuentes M, Machuca-Ariza J, Ruiz-Martos A, Ramos-Robles MC, Martínez-Lara I (2016) Long-term outcome of dental implants after maxillary augmentation with and without bone grafting. Med Oral Patol Oral Cir Bucal 21: 229-235.
- Lundgren S, Cricchio G, Hallman M, Jungner M, Rasmusson L, et al. (2017) Sinus floor elevation procedures to enable implant placement and integration: techniques, biological aspects and clinical outcomes. Periodontol 73: 103-120.
- Del Fabbro M, Testori T, Francetti L, Weinstein R (2004) Systematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent 24: 565-577.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi