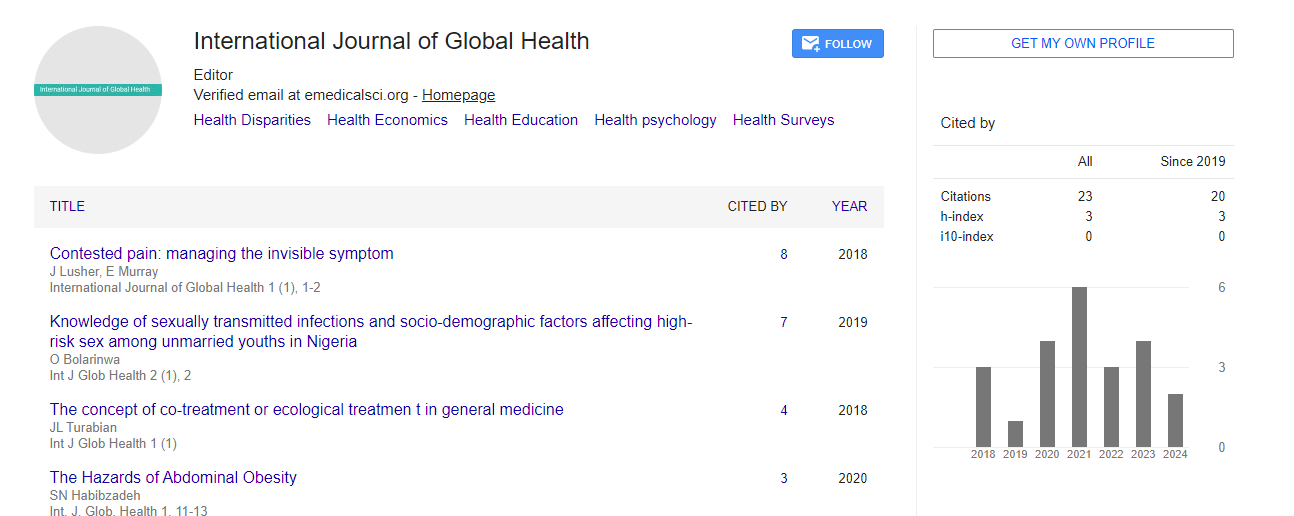
Review Article, Int J Glob Health Vol: 4 Issue: 4
The effect of an intervention to reduce household air pollution and carbon monoxide levels among Sudanese women cooking with biomass fuels and their children.
Kristin Sznajder*
Masters of Science Global Health Equity, Medical College of Wisconsin, Wauwatosa, USA
- *Corresponding Author:
- Kristin Sznajder
Masters of Science Global Health Equity, Medical College Of Wisconsin, Wauwatosa, USA
Tel: 3125479422
E-mail: ksznajde@phs.psu.edu
Received Date: July 02, 2021; Accepted Date: July 09, 2021; Published Date: July 16, 2021
Citation: Sznajder K (2021) The effect of an intervention to reduce household air pollution and carbon monoxide levels among Sudanese women cooking with biomass fuels and their children. Int J Glob Health 4:4. 139.
Copyright: © All articles published in International Journal of Global Health are the property of SciTechnol, and is protected by copyright laws. Copyright © 2021, SciTechnol, All Rights Reserved.
Keywords: Mortality Rate, Non-communicable Diseases, Pollution studies, household air pollution
Introduction
Energy poverty presents a serious challenge in Sub-Saharan Africa. Only 12% of Africans use cook stoves that run on fuels such as liquefied petroleum, electricity or renewable fuels such as biogas, ethanol or solar [1]. Thus, the vast majority of households rely on biomass fuels for cooking which traditionally occurs in small poorly ventilated dwellings and produces the smoky air of household air pollution. Evidence from the World Bank 2014 report shows that approximately 600,000 Africans die annually and many more suffer from chronic illnesses due to household air pollution [1].
Monitoring of indoor air pollution has been carried out primarily by measuring indirect exposure in dwellings and on the clothes of the residents [3]. These techniques measure the primary products of partial biomass fuel combustion: carbon monoxide, nitrogen dioxide, sulfur dioxide, and particulate matter [4] and are associated with variations of exposure within households and sub-groups. Carbon monoxide [CO] is absorbed into the body after inhalation and blood levels can be measured. Health related effects similar to those reported with household air pollution [HAP] exposure have been reported with CO poisoning including symptoms involving the heart, [5] central nervous system, [6] and placenta [7].
In Sub-Saharan Africa, where the majority of the population cooks indoors with biomass fuels, global efforts continue to develop improved stoves which may reduce HAP exposure [8]. Behavioral studies have looked at cooking practices but have not looked at the importance of cooking location nor have they measured the CO levels associated with improved cook stoves nor a change in cooking location [9].
In 2015, Suliman and colleagues carried out a study [10] in Port Sudan, Sudan which looked at the CO levels of women and their children living and cooking in small poorly ventilated dwellings with biomass fuels or gas. Data points included CO levels and several health effects of CO poisoning. The women who cooked with biomass fuels had mean CO levels of 18%. The women who cooked with gas had mean CO levels of 12%. Both groups had symptoms of CO poisoning. The current study was a natural follow up, an effort to educate women about the effects of HAP and to provide them with a cooking location with less HAP exposure and an opportunity to decrease their symptoms of CO poisoning. The study hypothesis was that regular cooking in a well-ventilated cooking site would result in a drop of 50% in the CO levels among study participants and some abatement of their CO poisoning symptoms.
Materials and Methods
Port Sudan, a large city in eastern Sudan was chosen for this study for several reasons. There is a large population of lower socioeconomic status women with children 1-5 years of age living in small poorly ventilated dwellings who cook with biomass fuels and congregate in government sponsored women’s centers where they learn to read and write. Members of the faculty of the Red sea University Faculty of Medicine were interested in the study and had access to the target population. A previous study which enrolled this Port Sudan population had been carried out successfully [10].
A Sudanese research team which included a field director, a study director, 3 female physicians, and 6 women’s center counselors was recruited.
Information sheets were developed for the Sudanese research team and study participants to explain the effects of HAP, the study purpose, why a consent form was necessary, and why children under 5 years of age were included. Because study participants were illiterate or semiliterate, a verbal consent form was written using the Penn State Milton S. Hershey Medical Center Institutional Review Board guidelines. Permission to include children was part of the verbal consent form.
Questionnaires for women and children were developed to obtain a history of HAP exposure due to a variety of factors such as cooking fuels, tobacco use, incense use, and dwelling size. A second questionnaire was developed to obtain a history of potential health effects of HAP exposure. All documents were translated into Arabic and the accuracy of the translations verified by third parties not involved in the study. CO-oximetry was performed on mothers and children. The Wong-Baker pediatric pain scale was used to assess headache severity.
Ethical approval
The study was approved by the Penn State Milton S. Hershey Medical Center Institutional Review Board, the Ethics Committee of the Redsea University Faculty of Medicine as well as the Minister of Health Red sea State.
Participant Recruitment and Enrollment
This was a four year study, 2016-2019. Each year prior to starting/ restarting the study the health related effects of HAP exposure, the consent process, the questionnaires and how to use the CO- oximeter were reviewed with the team. Counselors at the women’s centers were initially trained to recruit potential subjects and were asked in each subsequent year to gather previously enrolled subjects for follow up evaluation as well as to evaluate the new cooking location at their weekly visits. At each of the two women’s centers chosen for the study, approximately 50-60 local women come regularly to learn to read and write. All potential subjects recruited by the counselors were offered an opportunity to participate in the research. The research team reviewed the educational materials and why children under 5 years of age were to be included and the consent form. Each subject was asked to check or initial the consent form if she agreed to participate. All subjects initially recruited were included with the exception of women who appeared to be severely ill and were excluded and referred for hospital care.
Subjects who owned their own home were recruited to the experimental group and subjects who did not own their home were recruited to the control group. Subjects were divided in this way because the construction of a well-ventilated cooking location was only possible if the property was owned by the woman or her family. Following the consent process, demographic and subjective data on dwelling size, cooking fuels and health information were collected on the women and their children. CO levels were measured in duplicate on both adults and children. The identical procedures were carried out by the research team in 2017, 2018, and 2019.
A well-ventilated outside cooking location [6ft x 7ft x 6ft] without walls, a cooking site in one corner and a corrugated iron roof [rakoobah] was built for each subject who owned her home and these women received a short discussion about the health effects of smoky air associated with cooking inside.
Counselors made weekly visits to each rakoobah recipient to ensure regular use of the new cooking location. The women assigned to the control group did not own their home, received no rakoobah and no discussion about the health effects of smoky air.
In 2017, when the results of the first year of study became available, a more formal HAP education program was started for the rakoobah recipients and counselors. In bi-monthly meetings at the women’s centers the study director reviewed the negative health effects of breathing smoky air and the symptoms of chronic CO poisoning. The counselors continued their weekly home visits to reinforce and encourage regular rakoobah use. This process started in August of 2017 and continued into January 2018. The education programs at the women’s centers continued throughout 2018 and concluded with the last study visit in February 2019.
Equipment
Three Masimo Rad-57 CO-oximeters together with pediatric and adult sensors were provided by the Masimo Corporation, Irvine, California. The Masimo CO-oximeter is a non-invasive monitoring platform which uses eight wavelengths of light to measure oxygen and carbon monoxide saturation. The Masimo Corporation reports that the standard deviation for accuracy of the CO-oximeter is +/- 3% [11] while Zaouter and Zavesky [12] report readings of +4% to -6% when the true COHb% is in the 10-14% range.
The CO-oximeters and sensors were tested each year prior to starting the study and daily during the study. The CO determinations for the three instruments were consistent with values ranging from 1-3% on the investigators. Normal CO values as measured by the CO-oximeter for individuals with no risk factors, such as tobacco use, are up to 5%. Levels of 10% or more are considered to be distinctly abnormal and may be associated with symptoms of CO poisoning.
Statistical Analysis
Frequencies and percentages of potential sources of household air pollution exposure were reported and compared between the study and control groups using Chi-square and Fisher’s exact tests. Mean CO levels and headache pain severity scores were estimated and compared between the study and control groups in repeated measures analysis of covariance models with the factor for year nested within groups. Results are reported in terms of model-estimated means, 95% confidence intervals and p- values. Frequency of headache, fatigue, weakness and dyspnea were compared between the study and control groups in repeated measures logistic regression models with the factor for year nested within groups. Results are reported in terms of annual percentages with p-values for trend estimated from the models. Cross-sectional comparisons from additional data collected in 2020 were performed using Fisher’s exact tests. Significance was defined as p<0.05 and analyses were performed using SAS version 9.4 statistical software.
Results
Sixty-five study group women who received a rakoobah plus some HAP education and 46 control women who did not receive a rakoobah nor HAP education were enrolled in 2016. Factors potentially affecting levels of HAP exposure are listed in Table 1.
The course of the mean CO levels in the study and control groups is presented in Figure 1. At enrollment, the study group women had mean CO levels of 17.8% (95%CI 17.1-18.5) while the controls had mean CO levels of 17.5% (95%CI 16.7-18.3). One year later, 51 study group women and 31 controls were available for reevaluation. The CO levels in the study group dropped to a mean of 15.9% (95%CI 15.1-16.6) while the control group means levels remained stable. Careful questioning of the study group women revealed that eleven women did not use their rakoobah at all and their mean CO levels were 19.2%. At the same time, the mean CO levels of the 40 compliant or semi-compliant actually were 14.8%. After 24 weeks of formal HAP education [2017-2018] by the study director, the mean CO levels of the study group dropped to 4.9% (95%CI 4.2-5.6) and the controls to 6.0% (95%CI 5.1-6.9). One year later, in 2019 the mean CO levels remained steady for both groups at 4.8% (95%CI 4.1-5.5) and 6.1% (95%CI 5.1-7.1), respectively.
Thirty-three children of mothers in the study group and 19 children of control mothers were enrolled. The children’s mean levels at enrollment reflected that of their mothers in the study and control groups: 14.2% (95%CI 13.3-15.2) and 13.3% (95%CI 12.0-14.6), respectively. As with the study mothers the children’s mean CO levels dropped slightly in 2017 while the children of control mothers mean CO level increased slightly to 14.0% (95%CI 12.6-15.3). In 2018 and 2019 the drop in mean CO levels of the children mirrored the change in their mothers’ levels as shown in Figure 2.
Headaches were initially reported by almost all study and control subjects, 88% and 89% respectively. Over the three study years, reports of headache decreased among study subjects (trend test p=0.004) but did not decrease among controls (trend test p=0.54). Reports of headache severity were measured using the Wong-Baker pediatric pain scale where subjects choose a picture that reflects the severity of their pain. The pain scale levels remained stable within each group although the controls consistently reported more severe pain with a mean score of 4.5 (95%CI 3.8-5.2) in 2019 compared with 2.4 (95%CI 1.8-3.0) among study subjects in the same year (p<0.001).
<| Rooms in Dwelling | Research (n=65) | Control (n=46) | P-value | ||
|---|---|---|---|---|---|
| No. Subjects | Percentage | No. Subjects | Percentage | ||
| One | 50 | 76.9 | 29 | 63.0 | 0.28 |
| Two | 12 | 18.5 | 14 | 30.4 | |
| Three | 3 | 4.6 | 3 | 6.5 | |
| Cooking Fuels | |||||
| Charcoal/Wood | 65 | 100.0 | 46 | 100.0 | --- |
| Dung | 4 | 6.2 | 2 | 4.4 | 0.68 |
| Crop Residues | 42 | 64.6 | 31 | 67.4 | 0.76 |
| Plastic | 50 | 76.9 | 32 | 69.6 | 0.38 |
| Household Lighting | |||||
| Wood | 2 | 3.3 | 0 | 0.0 | 0.50 |
| Kerosene | 9 | 15.0 | 11 | 23.9 | 0.25 |
| Gas | 0 | 0.0 | 0 | 0.0 | --- |
| Flashlight | 50 | 83.3 | 35 | 76.1 | 0.35 |
| Other | |||||
| Tobacco | 10 | 15.4 | 6 | 13.0 | 0.73 |
| Incense | 63 | 96.9 | 45 | 97.8 | 0.77 |
| Dukhon | 35 | 53.8 | 23 | 50.0 | 0.69 |
Table 1: Potential Sources of Household Air Pollution Exposure.
p>At enrollment less than half of the study subjects reported dyspnea (45%), while only 33% of control women recognized this symptom. Over the three study years, 43% of the study group who initially reported dyspnea reported improvement in their dyspnea while only 6% of the controls reported improvement. Even fewer study women at enrollment reported fatigue (40%) and weakness (25%) while fewer still of the control women reported fatigue (33%) and weakness (20%). Reports of improvement in these symptoms were inconsistent and varied without explanation from year to year.In 2019, 90% of the study women reported fewer visits for health care versus 76% of the controls (Fisher’s exact p=0.13). In a brief 2020 follow up study all study women reported that they were cooking in the rakoobah while 19% of the controls reported that they were not cooking outside. In an effort to better understand some of the differences between the control and study groups information concerning years of schooling was collected. Sixty-seven percent of study women either reported not attending school or attending up to sixth grade (average 3.5 years) while 90% of control women reported no school attendance or attending up to sixth grade (average 1 year) (Fisher’s exact p=0.08).
< h3>DiscussionThe hypothesis prior to the start of the study was that a well-ventilated cooking location would be associated with drops in the mean CO level of approximately 50% and improvement in the symptoms of CO poisoning among study group women. In the first year of the study, 2016/2017 the team learned that for women with low socioeconomic status and who were unable to read or write, a change in cooking location and minimal education about HAP was not sufficient and clearly required a much more robust educational component. In 2016-2017, 22% of the study group women failed to use their rakoobah and the others cooked in the rakoobah sporadically. When the new more intensive education component was introduced, the study women started to use their rakoobah regularly and their mean CO levels dropped significantly.
Why did the mean CO levels of the control women unexpectedly drop in 2018? The control women may have participated in some of the bi-monthly education sessions carried out at the women’s centers or the control women noticed improvement in the health of the women in the study group. This theory is substantiated by reports to the investigators by control women who noted that the women who cooked in the rakoobah appeared to feel better so they too began to cook outside and their CO levels also dropped.
The mean CO levels of the children in the study group reflected that of the mothers. A small drop in CO levels in 2017 followed by a large drop in 2018 which remained stable in 2019 while the control children, like their mothers, had a slight rise in 2017 followed by a big drop in 2018 and a stable 2019 level. This is likely because children spend a lot of their time held or near their mothers. Therefore, interventions to reduce exposure to biomass fuels will usually improve both the mother and child CO levels.
CO, a colorless odorless gas is excreted almost entirely in exhaled air. At rest, the elimination half-life of blood CO is approximately 320 minutes for a subject inhaling 21% oxygen or room air at normal atmospheric pressure. [13] The half-life may increase with age and decrease with physical activity.
Initially elimination is rapid but then becomes slower when the level of carboxyhemoglobin drops. In this study the study and control subjects were breathing a mixture of smoky and fresh air thus the elimination half-life must have been considerably longer. However, 24 weeks, the period of intensive HAP education, provided between late 2017 and early 2018 was sufficient to decrease study subjects’ mean CO levels by 69% [15.9% to 4.9%] and the controls by 66% [17.8% to 6.0%]; the study children by 79% [13.1% to 2.8%] and the control children by 69% [14.0% to 4.4%]. The mean levels continued to drop during 2018 so that in early 2019 the levels were at normal physiologic levels of less than 5%.
< p>The incomplete combustion of biomass fuels results in several pollutants: carbon monoxide, sulfur dioxide, nitrogen dioxide and particles of various sizes. Carbon monoxide [CO] is the only product of incomplete biomass combustion which can be measured in the body. Exposure to CO can lead to a variety of lesions in the central nervous system which in turn can lead to reports of headache.[14] The use of plastic, primarily bags, to start cooking fires is a different source of HAP and results in the release of toxic gasses such as dioxins, furans, polychlorinated biphenyl, and CO. Inhalation of these gasses aggravates chronic respiratory disease, may cause headache, and may affect the central nervous system.[15] It is unclear how long the neurologic/headache recovery period is for chronic CO poisoning, but Betterman states that the neurologic outcome is highly variable with acute CO poisoning.[16] And hampson reports that 35% of patients with acute CO poisoning had headaches after one year.[17] There are no long term studies which report the neurologic outcome in individuals with chronic CO poisoning due to HAP nor due to long term dioxin/furan exposure which would help us to understand the study results.It is unclear why women in the control group reported more headaches and greater severity of headaches throughout the study when the course of their mean CO levels paralleled that of the study group women and their exposure experience appeared to be similar. However, the women chosen to be controls were different in several respects. Not only did they not own their houses but they reported more physician visits and fewer years of schooling for an average of one year compared with 3.5 years for the study subjects. As a result they may not have understood the questions, may have had more health problems, or have exaggerated their symptoms in an effort to get more help from the investigators or counselors.
Measuring a single pollutant may not be an adequate surrogate for other pollutants. Carter et al report that exposure to CO is not a reliable measure of exposure to particulate matter [PM 2.5]. [3] Studies have not been done which correlate PM 2.5 exposure with CO levels as measured by the CO-oximeter. Yet, the particulate matter in smoky air of HAP is the major cause of respiratory disease in adults and children and there is strong evidence linking HAP exposure to chronic obstructive pulmonary disease and chronic bronchitis. [18, 19] In this study, the smoky air exposure due to cooking was decreased but not eliminated, the levels of ambient air pollution were unchanged, and the use of tobacco, incense, and plastic continued. Thus, subjects and controls continued to inhale smaller amounts of the same pollutants producing persistent respiratory symptoms albeit improved in some cases. The reports of weakness and fatigue were inconsistent over the study period among both study and control groups.
Perhaps these women did not recognize these symptoms or considered this to be their normal state. Or an alternative explanation is that in this population of women there are other commonly found diagnoses which are associated with dyspnea, weakness and fatigue such as chronic lung disease, anemia, malnutrition and tuberculosis.
One of the limitations of this study is the small number of study and control subjects enrolled and the failure of the investigators to factor in the nomadic nature of this population. As a result 18-22% of the study group and 24-33% of the controls were not available for follow up in any given year. The study team questioned the counselors about the absentees and found that two of the study subjects had died, three were seeking medical help, and two had very heavy henna changes on their hands which prevented CO-oximetry. An additional seven women in the study group were thought to be “traveling.” Similarly, many of the absent control women were thought to be “traveling.” At this season of the year both groups might have traveled to plant their crops. However, after year one [2017] the total number of subjects in each group was stable. A second limitation was the failure to perform CO levels at a greater number of time points which would have provided more data points and helped to better understand the changes in CO levels over 3 years. A third study limitation was failure to consider and collect more data concerning the effects of incineration of other substances such as garbage, plastic and other potentially toxic products on ambient air pollution. The combustion of these products may have had a significant effect on the symptoms which we were trying to measure, and explained the fact that in spite of achieving CO levels in a normal physiologic range the symptoms of CO poisoning did not improve significantly.
This is an imperfect study in many ways but the study clearly demonstrates that: 1. An effective education program can result in major changes in cooking behavior; 2. The changes in cooking behavior endured for more than one year; 3. The changes in cooking behavior/location are associated with lower CO levels; 4.There was a ripple effect among control women who began to cook outside when they realized the effects of the education program and recognized that their friends cooking in the rakoobah felt better. The results further suggest that a similar education program might be effective in developing a solar cooking program for a similar group of women. A change to solar cooking could decrease exposure to smoky air, decrease the cost of biomass fuels, decrease the risk of burn injuries among children and mothers, decrease the rate of deforestation and eliminate the danger of attack for girls and women sent to scavenge for wood although it might not alter the symptoms which these women report.
References
- World Bank Group Report 98664 second edition Clean and Improved Cooking in Sub-Saharan Africa, a Landscape Report (2014).
- Carter E, Norris C, Dionisio KL, Balakrishnan K, Checkley W, et al. “Assessing exposure to household air pollution: a systemic review and pooled analysis of carbon monoxide as a surrogate measure of particulate matter.” Environ Health Perspect 125(2017): 076002.
- WHO Environmental health Criteria 213 Carbon Monoxide W.H.O.I.P.O.C. Safety (1999).
- Townsend C, Maynard R. “Effects on health of prolonged exposure to low concentrations of carbon monoxide.” Cooup Environ Med 59(2002): 708-7111.
- Prockop LD, Chickova RI. “Carbon Monoxide Intoxication: An Updated Review.” J Neurol Sci 262(2007): 122-130.
- Farrow JR, Davis GJ, Roy TM, McCloud LC, Nicholas GR. “Fetal death due to non-lethal maternal carbon monoxide poisoning.” J Forensic Sci 35(1990): 1448-1452.
- Clark MI, Peel JL, Balakrishnan K, Breyese PN, Chilrud SN, et al. “Health and Household Air Pollution from solid fuel use: the need for improved exposure assessment.” Environmental Health perspectives 121(2013): 1120-1128.
- Wiedmer D, Jouslin-De-Noray P, Graveaud F, Jahangirl V. “Socioeconomic Impacts of the Deployment of Improved fuel Efficient Stoves: the ILF Uganda Commercialization Program.” 8(2015): 1-13.
- Suliman AK, Saleh MM, Malek AA, Karrar AFP, Kitch D, et al. “Assessment of carbon monoxide exposure among women cooking with biomass fuels and their children living in Sudan. “Int J Glob health 1(2018): 1-12.
- Operators manual Masimo Corporation. Irvine, California.
- Zaouter C, Zavorsjy GS. “The measurement of carboxyhemoglobin and methemoglobin using a non-invasive pulse CO-oximeter.” Respir Physiol Neurobiol 182(2012): 88-92.
- Mathieu D (2006) Handbook on Hyperbaric Medicine. New York, Springer
- Gorman D, Drewery A, Huang YL, Sames C. “The clinical Toxicology of Carbon Monoxide.” Toxicology 187(2003): 25-38.
- Verma R, Vinoda KS, Papireddy M, Gowda ANS. “Toxic Polutants from Plastic Waste-A Review.” Procedia Environmental Sciences 35(2016): 701-708.
- Betterman K, Patel S. “Handbook of Clinical Neurology.”120(2014): 971-979
- Hampson NB, Hampson LA. “Characteristics of headache associated with acute carbon monoxide poisoning.” Headache 42(2002): 220-223.
- Smith KR, Mehta S, Feuz M. “Indoor air pollution from household use of solid fuels in Ezzati M and Rodgers A, Lopez AD, Murray CL, editors Comparative Quantification of Health Risk: Global and Regional Burden of disease due to Selected Major Factors.” Geneva: WHO (2004) 143-193.
- Amegah AK, Jaakola JJK. “Household air pollution and the sustainable goals.” Bulletin of the World health Organization 94(2016): 215 -221.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi