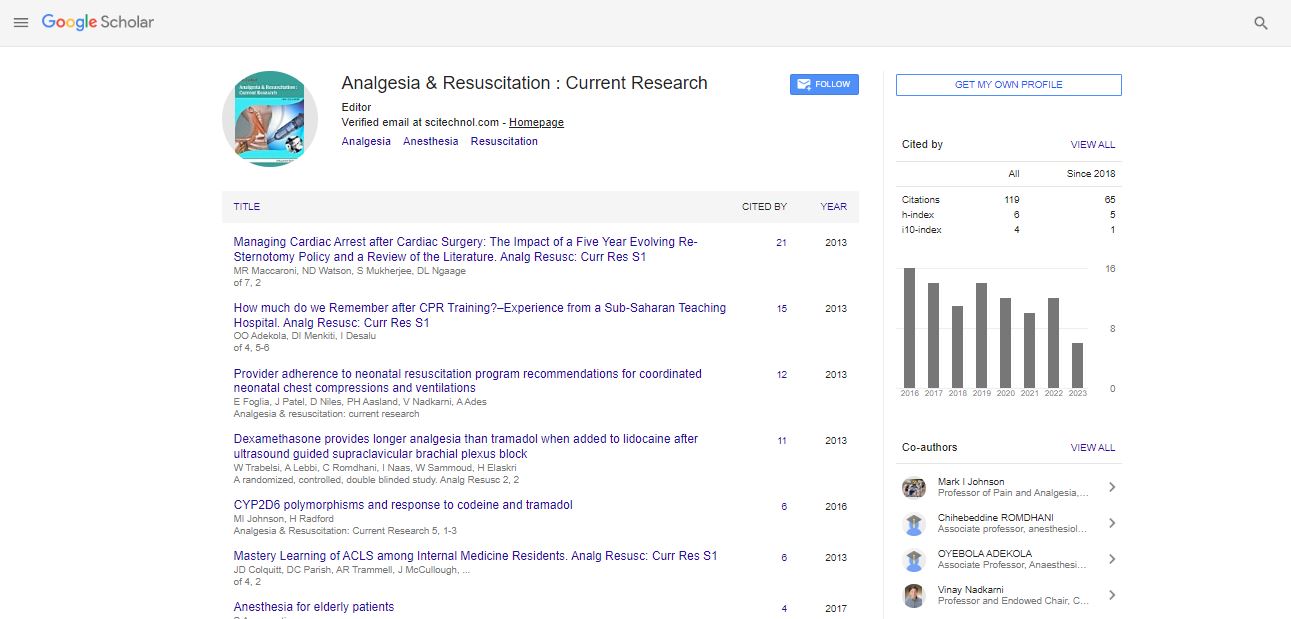
Editorial, Arcr Vol: 10 Issue: 3
The Current Role of General Anaesthesia
Matthew P Hardman*
Department of Anesthesiology, Mayo Clinic, 200 First St SW, Iraq
- *Corresponding Author:
- Matthew P. Hardman
Department of Anesthesiology, Mayo Clinic, 200 First St SW, Iraq
E-mail: matthewhardman.p@mao.edu
Received Date: June 15, 2021; Accepted Date: June 17, 2021; Published Date: June 20, 2021
Citation: Hardman MP (2021) The Current Role of General Anaesthesia. Analg Resusc: Curr Res 10:3.
Copyright: © All articles published in Analgesia & Resuscitation: Current Research are the property of SciTechnol, and is protected by copyright laws. Copyright © 2021, SciTechnol, All Rights Reserved.
Keywords: Anaesthesia
Introduction
The use of general anaesthesia for caesarean delivery has declined within the last decades thanks to the widespread utilization of neuraxial techniques and therefore the understanding that neuraxia lanesthesia are often provided even in urgent circumstances. In fact, the role of general anaesthesia for caesarean delivery has been revisited, because despite recent devices facilitating endotracheal intubation and clinical algorithms, guiding anesthesiologists facing challenging scenarios, risks, and complications of general anaesthesia at the time of delivery for both mother and neonate(s) remain significant. during this review, we’ll discuss clinical scenarios and risk factors related to general anaesthesia for caesarean delivery and address reasons why anesthesiologists should apply strategies to attenuate its use.
Despite global approaches to scale back the caesarean delivery rate worldwide, including recommendations to extend the utilization of elective inductions of labor and promote trials of labor after previous caesarean delivery, the middle for Disease Control and Prevention (CDC) reported a 31.9% caesarean delivery rate within the USA in 2018.
Striking the perfect balance between a discount within the overall caesarean delivery rate without increasing the chances for urgent/ emergent cesarean deliveries is complex, with clinical obstetric decisions potentially leading to unplanned scenarios that would significantly impact anesthetic options. If a caesarean delivery becomes emergent, the chances for general anaesthesia increase, and safe provision of any anesthetic becomes tougher . For obstetric anesthesiologists, predicting and preventing emergent situations may be a constant concern driven by the will to supply anesthesia within the safest manner to facilitate timely delivery of the neonate while ensuring a positive experience for the patient and family. With the common use of neuraxialanesthesia in obstetrics, and therefore the corresponding decrease in use of general anaesthesia , the risks related to the latter have decreased over time, as has anesthesia-related maternal mortality. the supply of improved anesthesia devices and monitoring and therefore the establishment of clinical recommendations for anesthesia management of obstetric patients are believed to elucidate the decrease in morbidity and mortality related to general anaesthesia.
Though controversial, the decision-to-delivery interval remains a standard auditing tool and has been deemed key to make sure optimal maternal and neonatal outcomes. Obstetric anesthesia practice has significantly evolved, and contemporary approaches for the supply of safe anesthesia in urgent circumstances include neuraxialanesthesia; appropriate communication between obstetricians, perinatologists, and anesthesiologists; and ongoing training including drills and simulation. A recent study evaluating the implementation of standardized team communication and processes to enhance outcomes during unscheduled cesarean deliveries reported a big decrease in decision to incision time intervals post-implementation.
Due to risks and complications related to general anaesthesia , even with the foremost recent devices facilitating endotracheal intubation and clinical algorithms guiding anesthesiologists facing challenging scenarios like cannot ventilate, cannot intubate, cannot oxygenate, the present role of general anaesthesia for caesarean delivery has been revisited.
In this review, we discuss how concerns related to general anaesthesia are different within the obstetric population as compared to the overall population, why specific efforts should be undertaken to avoid general anaesthesia for caesarean delivery, the way to minimize the necessity for general anaesthesia, and up to date considerations, including those related to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic.
Anesthesia-related complications and concerns
Securing maternal airway
An important point to know when considering general anaesthesia within the obstetric population is that procedural difficulty, complications, and failures are more prevalent within the obstetric versus general population. Besides a better risk of inauspicious intubation, pregnant women have increased morbidity during extubation, emergence, and recovery. Extubation failure is an occasion that’s relatively rare within the non-pregnant population, but this comparison between the 2 populations is difficult to form thanks to differences in definitions and number and sort of databases analyzed. Unlike for general anaesthesia , rates of major complications of neuraxialanesthesia (neurological injury, epidural hematoma, and/ or abscess) haven’t been found to be worse in pregnancy; actually , the danger for spinal epidural hematoma is probably going lower within the obstetric versus general population, even in thrombocytopenic parturients.
Over the last four decades, opportunities for training in obstetric anesthesia airway management have declined. A retrospective audit at one institution within the UK reported a decrease within the use of general anaesthesia for caesarean delivery from 76% in 1982 to 7.7% in 1998 and an extra decrease to 4.9% in 2006. With these low rates becoming more common worldwide, it’s been estimated that a lot of residents/trainees will graduate without performing a general anaesthetic during a pregnant patient. Lack of experience with general anaesthesia raises the priority of patient safety, as individual providers’ confidence is insufficient, and patients are going to be exposed to predictable complications related obstetric airway management. Simulation and advanced teaching modalities are suggested to partially alleviate or prevent such complications by providing a structured approach to avoid or steel oneself against failed intubation scenarios in obstetrics. additionally to knowledge and skill, simulation can improve behavioral aspects like interdisciplinary communication and team management, which is very relevant within the field of obstetric anesthesia.
Rates of general anaesthesia for caesarean delivery have overall decreased, and while general anaesthesia not may be a contributing factor to anesthesia-related maternal deaths, further opportunities to scale back its use should be emphasized. Raising awareness in identifying situations and patients in danger to assist avoid unnecessary general anaesthesia remains crucial.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi