Research Article, Res Rep Gastroenterol Vol: 2 Issue: 1
Successful Biliary Navigation Using Air in Malignant and Post-Surgical Hilar Strictures: A Prospective Controlled Trial
Elshimi E*, Attia AE, Eljaky A, Elshazly H and Allam M
Hepatology and Gastroenterology Department, National Liver Institute-Menoufia University, Egypt
*Corresponding Author : Esam Elshimi
Department of Hepatology, National Liver Institute, Menoufia University, Shebin Al-Kom, Menoufia, Egypt
Tel: +2-01064816073
E-mail: eelshimi@liver-eg.org
Received: January 22, 2018 Accepted: March 04, 2018 Published: March 12, 2018
Citation: Elshimi E, Attia AE, Eljaky A, Elshazly H, Allam M (2018) Successful Biliary Navigation Using Air in Malignant and Post-Surgical Hilar Strictures: A Prospective Controlled Trial. Res Rep Gastroenterol 2:1
Abstract
Background and study aim: Patient with biliary obstruction have high risk of cholangitis post ERCP We aimed to compare the feasibility and results of air versus Urographin in biliary navigation.
Patients and methods: From May 2016 to May 2017; 80 patients with hilar stricture were enrolled in this study, they were subdivided into 2 groups with equal number; Air and standard Urographin were used as a contrast in both groups respectively, Klatskin tumor was the most common cause of obstruction. Patients were evaluated at day one, day 7 and day 30 after stent placement.
Results: Successful biliary mapping, stent placement and drainage were achieved in all patients. There was no significant difference in age, gender, clinical presentation, liver function tests, and cause of stricture between both groups; (p > 0.05). Compared with the use of Urographin, more volume of air and longer operative time were observed. The rate of cholangitis and recovery from cholangitis in air group was significantly less than that in Urographin group (5.6% vs. 33.3%, p = 0.04). After ERCP, the mean hospital stay time was shorter in air group compared with control (p < 0.05). The difference of 30 days mortality between two groups was significant (p < 0.05). The X-ray time was significantly less in Urographin group.
Conclusion: Air was safe, costless and effective in biliary navigation for stent placement in hilar biliary strictures regardless the cause.
Keywords: Air cholangiogram; ERCP; Hilar strictures
Introduction
Primary liver cancer is the sixth most common cancer and third most common cause of cancer related mortality worldwide [1,2]. Although the biliary epithelium represents only about 3% of liver volume, Cholangiocarcinoma is the second most common primary malignant liver tumor after hepatocelluar carcinoma, it accounts up to 15% of primary liver cancers with 7.6 million annual cancer-related mortality worldwide and 3% of the 560,000 annual cancer-related deaths in the United States [3,4].
In 1965 Klatskin described tumors at the bifurcation of the hepatic duct in patients presented with obstructive jaundice, it is the most common type seen (60 % of cases). Gallbladder cancers and metastatic cancers can also cause hilar biliary stricture [5,6].
The 5-year survival in hilar tumors is less than 10% after the diagnosis with extremely poor prognosis, as most of them are inoperable at presentation. Biliary drainage and chemotherapy palliation are the alternative ways to improve survival and quality of life. Biliary drainage relieves; jaundice, associated pruritus, anorexia, dietary fatty food absorption, diarrhea, and disturbed sleep pattern. Endoscopic drainage is the preferred route versus percutaneous rout as it is less invasive and it restores the bile flow back to the gut [7,8].
Mapping the biliary system by contrast injection through the standard biliary catheter or tri-tome after selective biliary cannulation is very important for identification of stricture and planning for the proper way for drainage (the length, diameter and type of biliary stent). In addition, the pre-operative clarification of biliary anatomy is helpful for differentiating operable from non-operable cases in the setting of Klatskin tumors.
Postoperative biliary injuries (post-cholecystectomy, liver transplantation and post liver resection) represent the vast majority of causes of non-malignant biliary strictures. ERCP has been evolving in the last decades as the first priority in diagnosis and treatment of these settings.
Cholangitis is a potentially life threatening serious presentation in patients with obstructive jaundice. It has to be suspected early before developing systemic sepsis. Early aggressive management should be started by intra venous potent antibiotics, good hydration and biliary decompression.
Cholangitis is the most ERCP serious related complications however it is not common before biliary drainage in malignant obstruction [9-12]. This might argued to the retained contrast in non-well drained segments of the liver that leads to chemical injury of the biliary epithelium (increased rise of intrabiliary pressure) or contaminated contrast in those patients with poor immune system. So avoidance of injecting any dye during cholangiography represents the best way to decrease cholangitis.
Long time ago air was used by surgeons as a contrast material in cholangiography even prior to ERCP invention [13-15]. Many studies discussed its use as a contrast during ERCP procedure in patients allergic to Urographin or to reduce post ERCP cholangitis [16-21].
Study Design
This was a prospective randomized controlled study conducted in single tertiary referral center (National Liver Institute-Menoufia University). Sixty patients with malignant hilar obstruction plus twinty patients with non malignant hilar stricture were enrolled in this study between May 2016 and May 2017. Patients were randomized into 2 groups. The first group included 40 patients, 28 males and 12 females aged 39-82 years (31 with malignant hilar stricture and 9 with non malignant stricture). In these patients air was used as a cholangiogram. The second group included another 40 patients, 26 males and 14 females aged from 41-84 years (30 patients with malignant stricture and the rest 10 have biliary stricture caused by biliary trauma). Standard Urographin was used as a contrast agent for visualization of biliary system. Biliary drainage was planned for both groups using plastic or metal stents with variable lengths according to the level of hilar stricture.
Endoscopic Procedures
Pre-procedure medications
Good hydration and routine prophylactic broad-spectrum intravenous antibiotics administration (Cefoperazone 1 gm every 12 hours) are given for all patients. Prophylactic antibiotic started one day before the procedure and continued for at least 72 hours after procedure. Intravenous administration of Midazolam (5-15 mg), hyosine butylbromide (30-70 mg) and variable doses of I.V. Propofol as pre-operative and operative sedation.
ERCP
The ERCP procedures were done in prone position. We used Olympus side-viewing Duodenoscope (TJF190VR, Olympus, Tokyo, Japan). Zebra J-tip or straight tip guide wire (.035/400 cm from Boston Scientific Corp, Natick, Mass) was advanced through triple lumen papillotome from the same manufacturer), the guide wire was introduced through the malignant stenosis.
After attaining selective bile duct cannulation using guide wire technique cholangiogram was done. In the first group, biliary mapping was achieved by using 20 to 100 ml of air. In the second group contrast injection was obtained by injecting 10-20cc of diluted Urographin (4ml of Urographin mixed with 6 ml of normal saline).
Thereafter, dilatation of stricture-when indicated was done by using Sohendra dilator with graduated diameter 5-10f.
Minute sphincterotomy was performed in some cases. Plastic or metal stents with variable lengths according to the level of stricture were inserted under endoscopic and fluoroscopic control to drain obstructed ducts. All procedures were done only by experienced endoscopists and assistants (more than one thousand examinations).
Outcome measures
We eventually evaluated the following outcome measures: successful stent placement in proper position, successful drainage, ERCP-related complications. Effective stenting was clarified when the stents pass the stricture and free bile flow. Drop of serum bilirubin level to less than 75% of pre-treatment level within 30 days was considered a clinical success. Procedure-related morbidity and mortality was defined as complication or death directly related to the ERCP procedure within one month. Stent occlusion or primary non functioning was defined as the persistence of jaundice or bilirubin level more than 5 mg/dL, alkaline phosphatase, GG Tand transaminases 3 times the normal values and/or dilated bile ducts by ultrasound and or CT follow up indicating re-endoscopy. Cholangitis was diagnosed if fever and leucocytosis, recurrent jaundice and pain continued > 2days. Cholangitis within 2 weeks post ERCP was considered procedure-related.
Follow-up: Patients were evaluated clinically at day one, day 7, day 14 and day 30 after stent placement. Laboratory investigations were tested at; day 1, 3, 7, 14 and 30 days after the procedure.
All patients and their relatives were informed to call the investigators if they developed symptoms suggestive of cholangitis or stent occlusions.
Statistical analysis: SPSS software (SPSS, IBM, Chicago, Ill) was used for data analysis. Continuous variables were compared by using non-parametric tests for 2 related variables. Data were expressed as mean and SD.
Ethical approval: this study was discussed and met the ethical approval committee of our institution.
Results
Most of our patients with hilar biliary stricture are un-resectable due to delayed presentation, in our tertiary referral center–National Liver Institute; we evaluated all patients with obstructive jaundice, patients with normal caliber of CBD and dilated IHBR were enrolled in this study. We prospectively followed 80 patients with hilar biliary obstruction; biliary drainage was planned initially using plastic or metal stent placement as a drainage tool for palliation of the biliary stricture. Mapping of the biliary tree was done using air in mapping the biliary system in the first group of patients and Urographin in the second group.
The quality of air cholangiogram was satisfactory. Successful drainage was achieved in all patients in both groups with fall in serum bilirubin levels and relieve of symptoms of biliary obstruction. Only one patient developed Post ERCP cholangitis in group one versus 6 patients in group 2 after initial improvements. All patients in group one recovered except one while 8 out of 13 patients with cholangitis in group 2 recovered with antibiotic continuation; this was statistically significant. The 30 days mortality was significantly less in group one (one patient died versus 5).
The operative time was less in group 2 but it was not statistically significant. Although the quality of imaging using air cholangiogram was satisfactory; X- ray time was significantly longer in group one
Discussion
Most patients with hilar Cholangiocarcinoma are un-resectable. The prognosis of unresectable cases is poor, with only 5% to 20% being resectable. Palliative surgery is difficult and often impossible. Furthermore the mortality is very high; ≥ 20% [22,23].
In view of the poor prognosis plus the technical difficulties of surgery, endoscopic stent placement is considered a satisfactory goal. The palliative treatment of choice for these patients is the biliary decompression and chemotherapy and or radiotherapy [24]. Dowsett et al. stated that: drainage of 25% of the liver volume can achieve adequate palliation, improvement in biochemical parameters, patients’ general condition and relief of symptoms [25].
Cholangiography during ERCP is one of the essential steps for biliary navigation and diagnosis of biliary obstruction before stent insertion to avoid complications as perforation, pancreatic, cystic duct cannulation, or stent mal-positioning (proximal end of the stent below the strictures).
Cholangitis may be a complication of biliary obstruction; however it is more common in calcular obstructive jaundice than malignant obstruction before biliary decompression. But cholangitis is a major and fatal post ERCP complication in malignant biliary obstruction after stenting and occurs in 4% to 57% of cases [26,27].
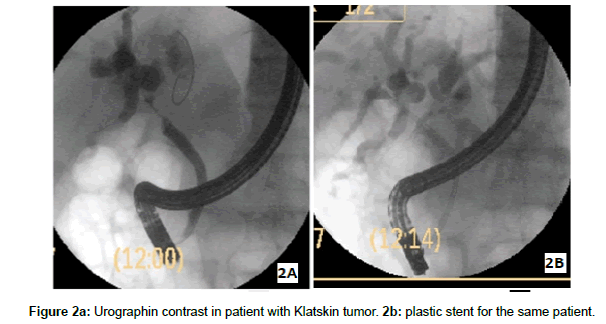
We conducted our study to test air as a potential available costless safe contrast to avoid or reduce post ERCP cholangitis in malignant and non-malignant hilar stricture and to study its value in cretin group of patient with biliary obstruction and cholangitis (Table 1 and Figure 1a-3b). We also evaluated the procedure related complications when using air in biliary navigation (Table 1). To our knowledge we are the first group studied the use of as a cholangiogram in patients with non malignant biliary strictures (Table 1).
| Group I Air cholangiogram | Group II Contrast cholangiogram | p- value | |
|---|---|---|---|
| Total number | 40 | 40 | |
| Gender (M/F) | 28/12 | 26/14 | 0.75 |
| Age (mean± SD) | 56± 8.5 | 55±7 | 0.67 |
| Etiology of hilar stricture Klatskin HCC Metastasis Gall baldder carcinoma Liver resection Post liver transplantation Post cholicystectomy |
Total =40 20 2 5 4 1 2 5 |
Total =40 22/ 2 2 4 0 3 7 |
0.71 |
| Clinical presentation Jaundice Pain Fever Itching Anorexia Weight loss Cholangitis |
40 7 5 24 30 36 7 |
39 10 7 22 35 37 6 |
0.99 |
| Laboratory data Mean direct serum Bilirubin ALT INR ALP GGT TLC |
20±754±15 2.5±1.5 350±40 170±20 7400±8000 |
17±5.5 58±11 2.1±1.6 340±65 190±25 6800±7300 |
0.14 0.34 0.42 0.56 0.008 0.37 |
| Imaging Liver metastasis PVT Ascites |
7 8 5 |
6 9 3 |
0.98 |
Table 1: The baseline characteristics of the studied patients.
Our study was a controlled prospective study. The quality of air cholangiogram was comparable to Urographin cholangiogram and both contrasts were accepted in mapping the biliary system for all subjects and the positioning of biliary stent was excellent. However the lower border of the stricture was not delineated perfectly during procedure with air contrast as air usually escapes from papilla when injected below the stricture. This issue obliged the endoscopists to choose longer metal stents to pass trans-papillary that looks sometimes technically difficult as the maximum lengths of metal stents is usually shorter than plastic stents.
We additionally compared the X-ray dose and operative time between both groups. The X-ray dose was significantly less in Urographin cholangiogram than air cholangiogram, probably the quality of Urographin cholangiogram is better or at least the endoscopists are more familiar with Urographin fluoroscopy. The operative time was longer in air group but this was not statistically significant. No available data in the literature about X-ray dose and operative time (Table 2).
| Group I Air cholangiogram | Group II Contrast cholangiogram | p- value | |
|---|---|---|---|
| Total number | 40 | 40 | |
| Pre-ERCP cholangitis Post ERCP cholangitis Total Recovered Pancreatitis Perforation: Bleeding: Air embolism Failure for cannulation 30 days mortality |
6 1 7 6 1 0 0 0 0 0 |
7 6 13 6 1 0 0 0 4 0 |
0.03 0.5 ---- |
| Operative time (time passed from selective cannulation till the end of procedure): X-ray dose (time passed from selective cannulation till the end of procedure): Hospital Stay (days): |
8±3.5 minutes 3.5±1.5minutes | 7±2.5 minutes 2±1minutes | 0.31 0.22 |
| Type of biliary stents: Metal Plastic |
11 29 |
13 27 |
Table 2: The complications, operative time, X ray dose and type of stents of the studied patients.
This is looks of some value when selecting the ideal contrast. Procedure related cholangitis was significantly high when we used Urographin as a contrast versus air contrast (only one case had cholangitis with air cholangiogram versus 6 cases (Table 2)
The high incidence of cholangitis was perfectly studied by many authors. Chang et al. reported 6.3% incidence of ERCP related-cholangitis when they drained the same opacified lobe, versus 38% when both ducts were cholangiographically mapped but only one was stented [13]. We reported less post ERCP related cholangitis; about 30% when we visualized both lobes in our series with Urographin. Probably this might argued to the use of broad spectrum antibiotics and proper hydration for all our patients as an institution wise protocol.
In air contrastography group cholangitis and recovery from cholangitis was better (less hospital stay, rapid improvement of general condition and less mortality). This could be explained simply by that injection of Urographin contrast in the biliary system with cholangitis lead to spread of infection to more biliary segments plus its chemical injury to biliary epithelium.
Sud et al. used air as a contrast media in 17 patients prior to self expandable metal biliary stent deployment and they reported no cholangitis in their studied patients, however they got cholangiogram using magnetic resonant cholangiography before ERCP procedure. They stated that air leads to lesser intra-ductal pressure compared with Urographin. As air, being far less dense than Urographin, with 800-fold difference between both of them [18].
Lee et al. studied the safety and efficacy of air cholangiography in assisting bilateral self expandable metal stents placement in hilar biliary strictures; air contrast was successful to assist in metal stent placement with significantly less cholangitis in comparison to Urographin contrast. But the authors did not discuss the operative time and X-ray dose [28].
Pisello et al. retrospectively studied 188 inoperable Klatskin patients; air cholangiography was used in 70 patients of them and Urographin contrast was used in biliary visualization in 103 patients prior to stenting. The investigators stated that: in malignant hilar strictures air is considered as a safe cholangiogram with good feasibility and successful stenting. Patients experienced significantly less cholangitis versus Urographin cholangiogram in all types of hilar stricture [29].
Many authors drained both lobes as a routine procedure in patients with Bismuth type II-IV hilar stricture. However in another study, the authors proved no advantage in draining both ducts in hilar strictures [30].
De Palma et al achieved successful drainage by unilateral stenting in 94% of patients; cholangitis occurred in 8% only but with minimal contrast injection above the stricture [31]. However it was not known what was the minimal amount of contrast injection used in their patients.
Cholangitis can be minimized by: minimal contrast to avoid filling of un-drained segments, broad spectrum antibiotics, proper hydration, metal stents insertion, less invasive procedures and reduction of the operative time [29,32,33].
The operative time and X ray dose were evaluated in our patients and we found that when we used air as a contrast medium we needed more operative time and X ray doses to get optimum biliary decompression. To our knowledge our study was the first one in literature that discussed these factors.
Sezgin et al. tested air as contrast medium but in calcular obstructive jaundice patients. They found that air is not sufficient in detection of CBD stones [34].
From our experience cholangitis is considered a multi-factorial event after ERCP especially in this sector of patients. It may be patient related factors including the extension of tumor, number of attempts to pass the stenosis by guide wire, immune system, liver condition and presence of any hidden infection, and or procedure related factors including the experience of operative team, amount of contrast injected, the disinfection roles and success to drain all liver segments.
Air embolism is a rare fatal condition post ERCP [35-40]. In our study we expected that we will find some cases in the air contrast group however no case developed pots procedure air embolism.
Conclusion
It can be concluded that air cholangiography is safe costless and effective contrastogram, however more data are required to study the feasibility and safety of air cholangiography.
References
- Bismuth H, Castaing D, Traynor O (1988) Resection or palliation: priority of surgery in the treatment of hilar cancer. World J Surg 12: 39-47.
- Guthrie CM, Haddock G, De Beaux AC, et al. (1993) Changing trends in the management of extrahepatic cholangiocarcinoma. Br J Surg; 80: 1434-1439.
- Black K, Hanna SS, Langer B, et al. (1978) Management of carcinoma of the extrahepatic bile duct. Can J Surg 21: 542-545.
- Stain SC, Baer HU, Dennison AR, et al. (1992) Current management of hilar cholangiocarcinoma. Surg Gynecol Obstet 175: 579-588.
- Nakayama T, Ikeda A, Okuda K (1978) Percutaneous transhepatic drainage of the biliary tract: technique and results in 104 cases. Gastroenterology 74: 554-559.
- Hatfield AR, Tobias R, Terblanche J, et al. (1982) Preoperative external biliary drainage in obstructive jaundice. A prospective controlled clinical trial. Lancet 2: 896-899.
- Soehendra N, Frederix RV (1980) Palliative bile duct drainage - a new endoscopic method of introducing a transpapillary drain. Endoscopy 12: 8-11.
- Tytgat GN, Bartelsman JF, HartogJager DFC, et al. (1986) Upper intestinal and biliary tract endoprosthesis. Dig Dis Sci 31: 57S-76S.
- Lammer J, Neumayer K, Steiner H (1986) Biliary endoprosthesis in tumors at the hepatic duct bifurcation. Eur J Radiol 6: 275-279.
- Luman W, Cull A Palmer KR (1997) Quality of life in patients' stented for malignant biliary obstructions. Eur J Gastroenterol Hepatol 9: 481-484.
- Ballinger AB, McHugh M, Catnach SM, et al. (1994) Symptom relief and quality of life after stenting for malignant bile duct obstruction. Gut 35: 467-470.
- Polydorou AA, Cairns SR, Dowsett JF, et al. (1991) Palliation of proximal malignant biliary obstruction by endoscopic endoprosthesis insertion. Gut 32: 685-689.
- Bertino GG, Cole JW (1958) Air contrast cholangiography: a preliminary report. Surgery. 43: 795-797.
- Esposito G, Infranziai A, Gaeta S (1960) Postoperative cholangiography after injection of air. Lyon Chir 56: 465-467.
- Esposito G, Infranziai A, Gaeta S (1958) Air contrast cholangiography; experimental and clinical study. Rass Int Clin Ter 38: 998-1002.
- Mosca S, Secondulfo M, Defez M et al. (2001) Air contrastography technique for successful urgent ERCP in a high risk allergic patient. AmJ Gastroentero 96: 3458-3460.
- Lim PL, Porter KG (1999) Air as contrast for cholangiography in a patient with a history of allergy to radiopaque media. Endoscopy 31: S9.
- Sud R, Puri R, Choudhary NS, Mehta A, Jain PK (2014) Air cholangiogram is not inferior to dye cholangiogram for malignant hilar biliary obstruction: a randomized study of efficacy and safety. Indian J Gastroenterol 2014 Nov; 33: 537-542.
- Zhang R, Zhao L, Liu Z, Wang B, Hui N et al. (2013) Effect of CO2 cholangiography on post-ERCP cholangitis in patients with unresectable malignant hilar obstruction - a prospective, randomized controlled study. Scand J Gastroenterol. 48: 758-763.
- Singh V, Singh G, Gupta V, Gupta R, Kapoor R (2010) Contrast-free air cholangiography-assisted unilateral plastic stenting inmalignant hilar biliary obstruction. Hepatobiliary Pancreatol Dis Int. 9: 88–92
- Köklü S, Koçak E, Akbal E (2011) Air cholangiography for severe hilar obstruction at ERCP. Gastrointest Endosc. 73: 1326.
- Deviere J, Baize M, de Toeuf J, et al. (1988) Long-term follow-up of patients with hilar malignant stricture treated by endoscopic internal biliary drainage. Gastrointest Endosc 34: 95-101.
- Chang WH, Kortan P, Haber GB (1998) Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic drainage. Gastrointest Endosc 47: 354-362.
- Polydorou AA, Chisholm EM, Romanos AA, et al. (1989) A comparison of right versus left hepatic endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy 21: 266-271.
- Dowsett JF, Vaira D, Hatfield AR, et al. (1989) Endoscopic biliary therapy using the combined percutaneous and endoscopy technique. Gastroenterology 96: 1180-1186.
- Rerknimitr R, Kladcharoen N, Mahachai V, et al. (2004) Result of endoscopic biliary drainage in hilar cholangiocarcinoma. J Clin Gastroenterol 38: 518-23.
- Rerknimitr R, Attasaranya S, Kladchareon N, et al. (2002) Feasibility and complications of endoscopic biliary drainage in patients with malignant biliary obstruction at King Chulalongkorn Memorial Hospital. J Med Assoc Thai 85Suppl 1: S48-53.
- Lee J, Lee SH, Jang DK, et al. (2016) Air cholangiography in endoscopic bilateral stent-in-stent placement of metallic stents for malignant hilar biliary obstruction. Ther Adv aGastroenterol 9: 189–198.
- Pisello F, Geraci G, Modica G, et al.(2009) Cholangitis prevention in endoscopic Klatskin tumor palliation: air cholangiography technique. Langenbecks Arch Surg 394: 1109-1114.
- Hintze RE, Abou-Rebyeh H, Adler A, et al. (2001) Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. GastrointestEndosc 53: 40-46.
- De Palma G, Galloro G, Siciliano S, Iovino P, Catanzano C (2001) Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc 53: 547–553.
- Ducreux M, Liguory C, Lefebvre JF, et al. (1992) Management of malignant hilar biliary obstruction by endoscopy. Results and prognostic factors. Dig DisSci 37: 778-783.
- Sezgin O, Alt├?┬▒nta├?┬? E, Fehmi A, Yara├?┬? S, Sar├?┬▒ta├?┬? B, et al. (2014) Air cholangiogram is not sufficient to detect common bile duct stones during ERCP. Turk J Gastroenterol 25: 319-20.
- Kennedy C, Larvin M, Linsel J (1997) Fatal hepatic air embolism following ERCP. Gastrointest Endosc. 45: 187-188.
- Trabanco S, Pardo S, Williams M, Diaz J, Ruiz C (2017) Cerebral air embolism after ERCP. J Clin Anesth. 36: 133-135.
- Mathew J, Wang J (2015) Pulseless electrical activity arrest due to air embolism during endoscopic retrograde cholangiopancreatography: a case report and review of the literature. BMJ Open Gastroenterol 2015 2.
- Park S, Ahn JY, Ahn YE, Jeon SB, et al. (2016) Two Cases of Cerebral Air Embolism That Occurred during Esophageal Ballooning and Endoscopic Retrograde Cholangiopancreatography. Clin Endosc 49: 191-196.
- Fernandez FJ, Real-Noval H, Rodriguez-Rodriguez E (2016) Massive cerebral air embolism following endoscopic retrograde cholangiopancreatography. A case report and review of the literature. Rev Neurol 63: 497-500.
- Sisk JM, Choi MD, Casabianca AB, Hassan AM (2017) Two Cardiac Arrests Because of Venous Air Embolism During Endoscopic Retrograde Cholangiopancreatography: A Case Report. 8: 47-50.
- Voigt P, Schob S, Gottschling S, Kahn T, Surov A (2017) Systemic air embolism after endoscopy without vessel injury - A summary of reported cases. J Neurol Sci 376: 93-96.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi