Research Article, J Sleep Disor Treat Care Vol: 7 Issue: 2
Short-Term Effects of the Luco Hybrid Obstructive Sleep Apnea Appliance in Adults with Sleep Bruxism: A Quasi-Experimental Study
Ken Luco*
President at Luco Hybrid OSA Appliance Inc, University of Alberta, Kingston, Canada
*Corresponding Author : Ken Luco, DDS
President at Luco Hybrid OSA Appliance Inc, 1419 Butternut Creek Road, Canada
Tel: 613 888 6019
Fax: 613 544 0885
E-mail: DrLuco@sympatico.ca
Received: October 11, 2017 Accepted: May 24, 2018 Published: June 01, 2018
Citation: Luco K (2018) Short-Term Effects of the Luco Hybrid Obstructive Sleep Apnea Appliance in Adults with Sleep Bruxism: A Quasi-Experimental Study. J Sleep Disor: Treat Care 7:2. doi: 10.4172/2325-9639.1000211
Abstract
Sleep bruxism (SB) is a sleep-related repetitive movement disorder characterized by clenching or grinding of the teeth and/or bracing or thrusting of the mandible during sleep. The Luco Hybrid OSA Appliance was FDA cleared for treatment of sleep bruxism and to aid in the treatment of associated effects.
Keywords: Sleep bruxism; OSA appliance; Sleep
Background
Definition
Sleep bruxism (SB) is a sleep-related repetitive movement disorder characterized by clenching or grinding of the teeth and/or bracing or thrusting of the mandible during sleep. It is classified in the same category as restless leg syndrome and periodic limb movement syndrome by the American Academy of Sleep Medicine (AASM) [1]. SB affects 8% - 10% of the adult population and up to 80% of patients suffering from SB also demonstrate sleep arousals associated with the SB events [1,2].
Prevalence
There are three forms of SB described: phasic, tonic, and mixed. Phasic is characterized by 1 Hz frequency repetitive jaw-muscle activity with bursts lasting 0.25 to 2 seconds, tonic consists of sustained contractions lasting longer than 2 seconds, mixed, which has characteristics of both [1]. A proposed subclassification further defines SB by supported evidence for the diagnosis. Possible SB is based upon patient-reported symptoms/questionnaires, probable SB is based upon patient-reported symptoms and physical examination findings, definite SB is based upon patient-reported symptoms, examination findings and polysomnographic evidence, preferably with audio/audiovisual recordings [3].
Etiology
Bruxism has two circadian forms: Awake bruxism (AB) and Sleep bruxism (SB) that have two different suspected etiologies [3]. SB is thought to be centrally mediated and multifactorial in etiology. Central pattern generators (CPG), involved in mastication are involved in the pathogenesis of sleep bruxism. The CPGs for mastication are located in the dorsal medullary reticular column and the nucleus solitaries and are abnormally activated in sleep bruxism [4,5].
A recent study related traumatic brain injury to an increased incidence of SB further supports a central mechanism to SB [6]. Other studies have shown that the masseter inhibitory reflex (MIR) is affected by sleep bruxism with an advancement of the first exteroceptive suppression (ES1) and reduction or elimination of the second exteroceptive suppression (ES2) of the masseter inhibitory reflex [7-11].
Recent research also has found a common gene mutation in SB patients, specifically a mutation of the HTR2A gene on chromosome 13 (specifically an HTR2A rs2770304 polymorphism), where the C allele was associated with an increase in SB [12]. This mutation is also common to obstructive sleep apnea, tension type headaches, migraine headaches (without auras) and a myriad of psychiatric disorders [13-18]. This gene normally codes for serotonin receptors in the brain and the polymorphism results in an excess of serotonin receptors on some nuclei altering their function. This can result in decreased excitability of certain nuclei in the brain (including the first and second inhibitory nuclei of the MIR in the pons). There is a second gene mutation (DRD2 polymorphism) pertaining to dopamine receptors and that could explain insensitivity to dopamine contributing in the mandibular tremor seen in SB patients when they protrude end-toend [19].
The link between SB and episodic tension-type headaches (ETTH) relates to the exteroceptive suppressions or silent periods of the MIR. Both SB and ETTH cause an advancement of the ES1 phase and reduction or complete elimination of the ES2 phase of the MIR [20,21] (Figure 1). Waking with a tension/migraine type headache is common with sleep bruxism patients. Migraine type headaches (without auras) have been shown to have an increased susceptibility when the 5-HTR2A gene polymorphism is present [22].
In contrast, AB is considered a somatoform disorder and reaction to severe stress however the etiology is currently under debate [11]. Both types of bruxism (AB, SB) have been shown to be associated with Rett syndrome, Prader-Willi syndrome and Angelman syndrome implying a mechanistic type link between epigenetic regulation and bruxism [23-25]. There are certain drugs than are associated with SB (dopaminergic, serotonergic and adrenergic types). Medications such as Clonidine [26], Benserazide [27], Pramipexole [28] and Amitriptyline [29] have been studied with regard to treatment of SB. The study with Benserazide demonstrated an attenuation effect on SB [3] however there are significant side effects for safe use in the general population. Amitriptyline and others have been studied with little effect or unsafe long-term use. The research using L-Dopa analogues reinforces the theory of polymorphism of the dopamine receptors in SB. Selective serotonin reuptake inhibitors (Citalopram, Escitalopram, Fluoxetine, Paroxetine, and Sertraline) have been used with limited results. Botox injections have been studied and effectively reduce the bite force involved but no studies have shown a reduction in the associated TCR effect on heart rate and blood pressure and sensitization over time has been observed and one study implicated Botox injections to result in osteoarthritic changes of the TMJ [30,31]. The FDA has not cleared any of these interventions for sleep bruxism to date.
Signs and symptoms
SB can occur in all stages of sleep but is most commonly seen in stages N1 and N2 [1]. There is a clear arousal sequence that occurs with every SB event:
• An increase in sympatho-cardiac activity (increased heart rate, blood pressure and rate of respiration)
• An increase in EEG activity (sleep arousal)
• An increase in muscle activity involving the suprahyoid, masseter and temporalis muscles
• Activation of the sucking reflex (frequently resulting in cheek biting during SB events)
• Often concluding with the swallow reflex [1].
When both sleep apnea and SB occur in the same individual, the SB synchronizes with the apnea/snoring events, occurring slightly before or after the apnea event. It has been suggested that SB occurring close to apnea-hypopnea events may be a secondary form of SB [32-35]. The increases in blood pressure associated with SB can be also affected by associated body movements and sleep arousals that often occur with SB, which can also affect the magnitude of blood pressure surge with these events [1,36]. The increase in heart rate associated with sleep bruxism has been found to be due to direct stimulation of the Trigemino-Cardiac Reflex (TCR) which results in stimulation of the dorsal motor nucleus of the Vagus nerve (which directly affects heart rate) [36,37]. The gasserion ganglion is one of the few regions of the trigeminal nerve where stimulation of the TCR results in a stimulation of the dorsal motor nucleus (all other regions result in a decrease in heart rate and blood pressure, as is seen with the “diver’s reflex”) [38].
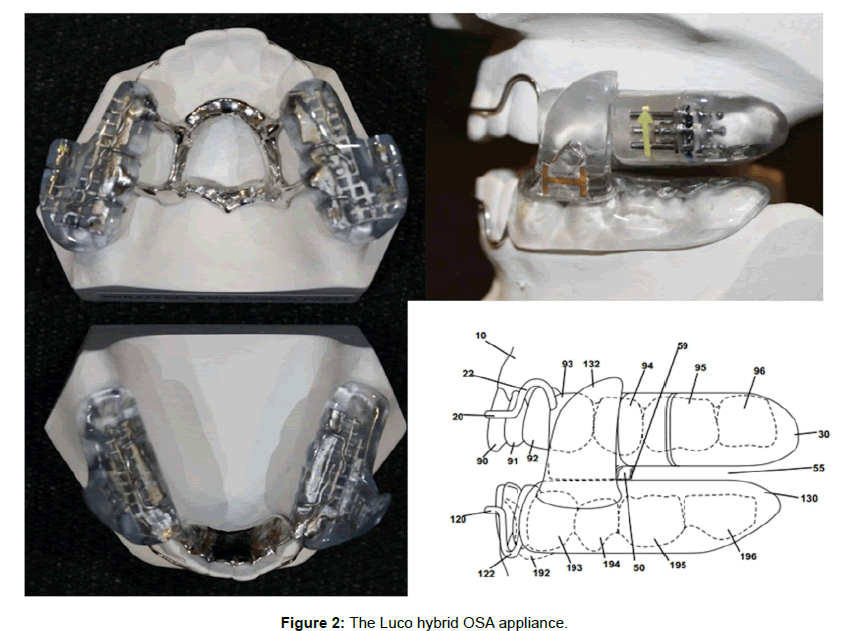
Until recently, there has been no effective treatment for SB [39,40]. July 29, 2016, the FDA cleared the Luco Hybrid OSA Appliance® (LHOA) (Figure 2) as the first treatment of SB and to aid in the treatment of associated tension/migraine type headaches in adults [41,42]. The device is based upon research that has shown that by directing bite force though the cuspid region (Figure 3) there is activating the periodontal- masseteric ligament-masseter (PLM) reflex of the cuspids, reducing muscle contraction in the masseter and temporalis muscles. The PLM reflex in the cuspid region is greater than the incisor, bicuspid and molar regions implying that the cuspids play a key role in mediation of bite force. This reflex is also located in the mesencephalic nucleus like the MIR. It is proposed that this reflex is not affected by HTR2A polymorphism like the MIR, and acts in re-establishment of masseter inhibition, and a reduction in the biting force, through a different pathway [43-45].
The aim of this interventional study was to assess the effectiveness of the LHOA in the treatment of primary SB and associated tension/ migraine type headaches in adult patients suffering from primary SB.
Materials and Methods
The study was designed to address the most common signs and symptoms of sleep bruxism and broken down into three areas of study:
Clinical:
• Clinical Examination:
1. Musculature
• Temporalis
• Masseter
• Medial pterygoid
• Lateral pterygoid
• Sphenomandibularus
• Posterior digastric
• Anterior digastric
• Sternocleidomastoid
• Trapezius
2. TMJ examination
• Lateral poles
• Posterior joint space
3. Mandibular range of motion
• Wide opening
• Left lateral
• Right lateral
• Protrusive
Home sleep study:
• Number of sleep bruxism events
1. Phasic
2. Tonic
3. Mixed
• Maximum duration of each type of sleep bruxism event
• Bruxism index
• Maximum heart rate
Visual analog scale
• TMJ pain on waking and later in the day
• Jaw muscle pain on waking and later in the day
• Tooth sensitivity to temperatures
• Tension/migraine type headaches on waking and later in the day
• Neck and shoulder pain on waking and later in the day
Pain in the neck and shoulder regions on waking (and later in the day) was included based upon research demonstrating the relationship of the anterior and posterior neck muscles co-activation with the masseter and temporalis muscles when biting with maximal forces (as are seen during SB events) [46-49].
79 subjects were recruited from patients referred for management of TMD or chronic facial pain to the clinic. Inclusion criteria for the subjects were based upon the clinical criteria for sleep bruxism as outlined by the American Academy of Sleep Medicine (AASM) [1]. All subjects were identified as probable sleep bruxism patients. All gave a history of nocturnal bruxism for at least 3 nights per week for the previous 6 months. All subjects demonstrated signs and symptoms consistent with probable sleep bruxism (including the presence of tooth grinding sounds while sleeping, as reported by a family member or spouse, hypersensitivity of the teeth to temperatures, TMJ and/or jaw muscle pain on waking and waking at least 3 nights per week with a tension/migraine type headache or having one develop later in the day).
All subjects were assigned a code that was used on all forms and documents. All subjects completed a detailed medical history form including prescribed and Over the Counter medications (to screen for medications that can affect sleep behavior or affect the dopaminergic, serotonergic or adrenergic systems), and were examined for the signs of sleep bruxism as outlined by the AASM including abnormal or excessive tooth wear, jaw muscle pain on palpation, jaw muscle hypertrophy (masseter and temporalis), mandibular or palatal tori, antigonial notching of the mandible and a tremor of the mandible when in an end-to-end biting position.
All subjects underwent a clinical examination (jaw/neck muscles, mandibular range of motion and TMJ examination), a home sleep study (Medibyte event 12 channel sleep recorder with EMG module (HSS) to record muscle activity, microphone for audio recording), and completed a visual analog scale (VAS) relating to symptoms of sleep bruxism. All subjects were fitted with a Luco Hybrid OSA Appliance set at 75% advancement [46]. At 7 days they were reassessed and the device adjusted for comfort as needed. At 14 days they were recalled and the initial protocol repeated (clinical examination, HSS, VAS scale). There were recalled again at 60 days and this protocol again repeated (clinical examination, HSS, VAS). The sleep recording was analyzed following the AASM guidelines for sleep bruxism [47]. Real time audio recordings were used with the HSS to reduced false positives [47].
Statistical analysis
Repeated measures Anova analysis followed by Tukey's multiple comparisons test (mean differences) was performed using GraphPad Prism version 7.03 for Windows, GraphPad Software, La Jolla California USA, www.graphpad.com.
Results
Of the 79 subjects considered, 62 demonstrated a majority of these signs and symptoms of SB and were considered for the study. 11 of the subjects dropped out before completion or were excluded due to incomplete documentation, demonstrated an inability to manage the treatment device or home sleep recorder or were found to suffer from concurrent sleep disordered breathing (obstructive/central sleep apnea, upper airway resistance syndrome) and were excluded from the study. 51 subjects were selected from this cohort that met the inclusion criteria (mean age ± SD, 45.7 ± 13.4 years, median 42.4 years, 26 male and 25 female) and were included in the study (Table 1).
| Variables | Onset | 14 Days | % | P< | 60 Days | % | P< | ||
|---|---|---|---|---|---|---|---|---|---|
| Clinical | Jaw Muscles | Temporalis | 15 | 6.9 | 54.1% | 0.0001 | 3.8 | 75.1% | 0.0001 |
| Masseter | 16.9 | 5.0 | 70.6% | 0.0001 | 1.9 | 88.5% | 0.0001 | ||
| Medial Pterygoid | 33.6 | 4.2 | 87.3% | 0.0001 | 1.1 | 99.9% | 0.0001 | ||
| Lateral Pterygoid | 35.5 | 2.3 | 93.5% | 0.0001 | 0.9 | 97.4% | 0.0001 | ||
| Sphenomandibularus | 15.7 | 4.1 | 74.1% | 0.0001 | 2.1 | 86.8% | 0.0001 | ||
| Posterior Digastric | 29.8 | 6.0 | 80.0% | 0.0001 | 3.0 | 90.0% | 0.0001 | ||
| Anterior Digastric | 20.2 | 3.3 | 82.4% | 0.0001 | 1.4 | 93.2% | 0.0001 | ||
| Neck Muscles | Sternocleidomastoid | 30.9 | 9.4 | 69.6% | 0.0001 | 5.1 | 83.4% | 0.0001 | |
| Trapezius | 27.3 | 9.8 | 64.0% | 0.0001 | 6.6 | 75.7% | 0.0001 | ||
| TMJ | Lateral Poles | 13.4 | 1.4 | 89.9% | 0.0001 | 0.3 | 97.5% | 0.0001 | |
| Posterior Joint Space | 15.3 | 1.5 | 90.4% | 0.0001 | 0.4 | 97.4% | 0.0001 | ||
| Range of Motion | Wide opening | 43.2 | 46.8 | +8.3% | 0.0001 | 48.1 | +11.2% | 0.0001 | |
| Left Lateral | 7.8 | 10.2 | +31.6% | 0.0001 | 10.8 | +39.6% | 0.0001 | ||
| Right Lateral | 8.8 | 11.2 | +27.5% | 0.0001 | 12.1 | +38.2% | 0.0001 | ||
| Protrusive | 8.5 | 11.3 | +32.8% | 0.0001 | 12.3 | +44.3% | 0.0001 | ||
| Home Sleep Study | Sleep Bruxism Heart Rate | Phasic Sleep Bruxism | 166.9 | 30.5 | 81.7% | 0.0001 | 16.5 | 90.1% | 0.0001 |
| Max Duration Phasic SB | 303.2 | 53.4 | 82.4% | 0.0001 | 31.3 | 89.7% | 0.0001 | ||
| Tonic Sleep Bruxism | 86.3 | 10.1 | 88.3% | 0.0001 | 6.6 | 92.3% | 0.0001 | ||
| Max Duration Tonic SB | 174.2 | 22.1 | 87.3% | 0.0001 | 15.2 | 91.3% | 0.0001 | ||
| Mixed Sleep Bruxism | 93.9 | 15.1 | 83.9% | 0.0001 | 11.7 | 87.6% | 0.0001 | ||
| Max Duration Mixed SB | 189.6 | 32.1 | 83.1% | 0.0001 | 26.3 | 86.7% | 0.0001 | ||
| Bruxism Index | 91.7 | 19.1 | 79.2% | 0.0001 | 14.1 | 86.4% | 0.0001 | ||
| Maximum Heart Rate | 118.7 | 68.7 | 42.1% | 0.0001 | 62.3 | 47.5% | 0.0001 | ||
| Visual Analog Scale | Jaw pain on waking / later in the day | 8.0 | 2.1 | 73.3% | 0.00001 | 1.0 | 87.8% | 0.0001 | |
| TMJ pain on waking / later in the day | 8.4 | 0.6 | 93.0% | 0.00001 | 0.3 | 97.0% | 0.0001 | ||
| Tooth Sensitivity to Temperatures | 8.5 | 1.0 | 88.7% | 0.00001 | 0.1 | 98.4% | 0.0001 | ||
| Tension/migraine headache on waking / later in the day | 8.2 | 2.2 | 73.1% | 0.00001 | 0.4 | 94.7% | 0.0001 | ||
| Neck and shoulder pain on waking / later in the day | 6.7 | 1.4 | 78.5% | 0.00001 | 0.6 | 91.5% | 0.0001 | ||
Range of motion measured in mm
VAS scale scored 0-10
Table 1: Summary of findings.
The data statistical analysis demonstrated a significant improvement in all of the studied metrics (P<0.00001) (Table 1). The clinical examination findings correlated well with the VAS completed by the subjects as well as the HSS recordings. There was a significant reduction in mean pain on palpation of the jaw musculature of 77.9% at 14 days, 90.0% at 60 days and of the neck musculature of 37.9% at 14 days and 62.0% at 60 days. TMJ palpation mean pain similarly was reduced by 89.9% at 14 days, 97.5% at 60 days on lateral pole palpation, and 90.4% at 14 days, 97.4% at 60 days for posterior joint space palpation. Mandibular range of motion increased by 8.3% at 14 days, 11.2% at 60 days for wide opening, 31.6% /39.6% for left lateral movement, 27.5%/38.2% for right lateral movement and 32,8%/44.3% for protrusive movement.
The HSS analysis demonstrated a reduction of 81.7% of phasic sleep bruxism events and 82.4% reduction on maximum duration of event at 14 days increasing to 90.1% reduction and 89.7% reduction in maximum duration of event at 60 days. Tonic sleep bruxism events were reduced 88.3% with an 87.3% reduction in maximum duration at 14 days, increasing to a reduction of 89.7% of SB events with a 91.3% reduction in duration of SB events at 60 days. Mixed sleep bruxism events were reduced 83.9% with a reduction of 83.1% in maximum duration of SB event at 14 days, 87.6% with a reduction of 86.4% in maximum duration of SB event at 60 days. Most importantly, the maximum heart rate was reduced by 42.1% at 14 days and 47.4% at 60 days. This strongly suggested that not only were the sleep bruxism events well controlled, by the trigemino-cardiac effect of sleep bruxism was also well controlled.
The VAS completed by the subjects at the three assessment stages demonstrated a similar reduction in symptoms. TMJ pain on waking and later in the day was reduced by 73.3% at 14 days, 87.8% at 60 days. Jaw muscle pain on waking and later in the day was reduced by 93.0% at 14 days, 97.0 at 60 days. Tooth sensitivity was reduced by 88.7% at 14 days, 98.4% at 60 days. Tension/migraine headaches on waking and later in the day were reduced 73.1% at 14 days, 94.7% at 60 days. Neck and shoulder pain on waking and later in the day was reduced by 78.5% at 14 days, increasing to 91.5% at 60 days.
Limitations of the Study
An obvious limitation of this study is that it was interventional and no controls were used and that the lead reviewer is the specification designer of the device. To reduce the first night effect of the device, it was decided upon early on to reassess at 60 days. Studies have shown that TMJ pain with mandibular advancement appliance can occur at 30 days in SB patients. It was not possible to directly measure blood pressure changes in real time in this study only heart rate relating the TCR. To verify a reduction in the TCR effect, this would have been ideal. To verify a re-activation of the masseter inhibitory reflex, it was not possible to place electric/magnetic peripheral stimuli as used in other studies, during sleep as subjects must be awake for this. As a result, only assumptions could be made from the results regarding a reactivation/normalization of the MIR. The study ended at 60 days; however it would be valuable to assess at a later time such as 6 or 12 months to determine if the results would remain or diminish.
Discussion
This study used multichannel home sleep recording to record in real time changes in the number and duration of sleep bruxism events, as well as the associated heart rate at three different times: at the onset before treatment, 14 days after treatment initiation and finally, at 60 days after treatment initiation. The results all significantly demonstrated a decrease in sleep bruxism and associated signs and symptoms (p<0.0001).
The Luco Hybrid OSA Appliance was FDA cleared in 2016 as the first treatment of sleep bruxism and to aid in the treatment of associated tension/migraine type headaches in adults [41]. This study supported this and demonstrated the effectiveness of the device in the treatment of sleep bruxism and tension/migraine headaches.
Conclusion
Despite the limitations of this study, it was observed that, in the short-term, the Luco Hybrid OSA Appliance was an effective treatment of sleep bruxism and associated tension/migraine type headaches in adult patients and was effective at reducing the associated TCR increases heart rate seen in SB. This suggested that by activating the PLM reflex with the forward cuspid bite of the LHOA, there was a decrease in SB activity and duration, and decrease in associated signs and symptoms. The reduction in the muscle pain on palpation of the cervical musculature (sternocleidomastoid and upper trapezius) was not expected and likely related to the decrease in ETTH seen. The reduction in maximum heart rate strongly suggested that the TCR effect on heart rate had been stabilized.
From a clinical standpoint, in spite of the subjects demonstrating a wide array of signs and symptoms, variations in occlusal schemes, variations in number of missing unreplaced teeth, variations in skeletal facial forms, all responded similarly, supporting a central mechanism for SB.
References
- American Academy of Sleep Medicine (2005) International classification of sleep disorders. Diagnostic and coding manual 2005:148-52.
- Mayer P, Heinzer R, Lavigne G (2016) Sleep bruxism in respiratory medicine practice. Chest 149: 262-271.
- Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, et al. (2013) Bruxism defined and graded: An international consensus. J Oral Rehab 40: 2-4.
- Guertin PA, Steuer I (2009) Key central pattern generators of the spinal cord, J Neurosci Res 87: 2399-2405.
- Arshavsky I, Deliagina TG, Orlovsky GN (2015) Central pattern generators: Mechanisms of the activity and their role in the control of "automatic" movements. Zh Vyssh Nerv Deiat Im I P Pavlova 65: 156-187.
- Suzuki Y, Arbour C, Khoury S, Giguère JF, Denis R, et al. Mild traumatic brain injury? A case-control study. Journal of Oral & Facial Pain and Headache 2017 October 3
- Luco K (2017) How sleep bruxism and tension headaches affect the masseter inhibitory reflex. J Sleep Disor: Treat Care 6:3.
- Schoenen J, Jamart B, Gerad P, Lenarduzzi P, Delwaide PJ (1987) Exteroceptive suppression of temporalis muscle activity in chronic headache. Neurology 37: 1834-1836.
- Cruccu G, Agostino R, Fornarelli M, Inghilleri M, Manfredi M (1984) Recovery cycle of the masseter inhibitory reflex in man. Neurosci Lett 49: 63-68.
- Godaux E, Desmedt JE (1975) Exteroceptive suppression and motor control of the masseter and temporalis muscles in normal man. Brain Res 85: 447-458.
- Aktekin B, Yaltkaya K, Ozkaynak S, Oguz Y (2001) Recovery cycle of the blink reflex and exteroceptive suppression of temporalis muscle activity in migraine and tension-type headache. Headache 41: 142-149.
- Oporto GH, Bornhardt T, Iturriaga V, Salazar LA (2016) Genetic polymorphisms in the serotonergic system are associated with circadian manifestations of bruxism. J Oral Rehabil. 43: 805-812.
- Wu W, Li Z, Tang T, Wu J, Liu F, et al. (2016) 5-HTR2A and IL-6 polymorphisms and obstructive sleep apnea-hypopnea syndrome. Biomed Rep 4: 203-208.
- Xu H, Guan J, Yi H, Yin S (2014) A systematic review and meta-analysis of the association between serotonergic gene polymorphisms and obstructive sleep apnea syndrome. PLoS One 9: e86460.
- Piatto VB, Carvalho TB, De Marchi NS, Molina FD, Maniglia JV (2011) Polymorphisms in the 5-HTR2A gene related to obstructive sleep apnea syndrome. Braz J Otorhinolaryngol 77: 348-355.
- Yücel Y, Co√?¬?kun S, Cengiz B, Özdemir HH, Uzar E, et al. (2016) Association of Polymorphisms within the Serotonin Receptor Genes 5-HTR1A, 5-HTR1B, 5-HTR2A and 5-HTR2C and Migraine Susceptibility in a Turkish Population. Clin Psychopharmacol Neurosci 14: 250-255.
- Nyholt DR, Curtain RP, Gaffney PT, Brimage P, Goadsby PJ, et al. (1996) Migraine association and linkage analyses of the human 5-hydroxytryptamine (5HT2A) receptor gene. Cephalalgia 16: 463-467.
- Gasparini CF, Smith RA, Griffiths LR (2017) Genetic and biochemical changes of the serotonergic system in migraine pathobiology. J Headache Pain 18: 20.
- Laine C, Yavuz U, D'Amico J, Gorassini M, Türker K, et al. (2015) Jaw tremor as a physiological biomarker of bruxism. Clin Neurophysiol 126: 1746-1753.
- Wallasch T, Reinecke M, Langohr H (1991) EMG analysis of the late exteroceptive suppression period of temporal muscle activity in episodic and chronic tension-type headaches. Cephalalgia 11: 109-112.
- Göbel H, Dworschak M (1996) Exteroceptive suppression of activity of the temporal muscle. Principles and applications. Der Nervenarzt 67: 846-859.
- Yücel Y, Co√?¬?kun S, Cengiz B, Özdemir HH, Uzar E, et al. (2016) Association of Polymorphisms within the Serotonin Receptor Genes 5-HTR1A, 5-HTR1B, 5-HTR2A and 5-HTR2C and Migraine Susceptibility in a Turkish Population. Clin Psychopharmacol Neurosci 14: 250-255.
- Young D, Nagarajan L, De Klerk N, Jacoby P, Ellaway C, et al. (2007) Sleep problems in Rett syndrome. Brain Dev 29: 609-616.
- Saeves R, Espelid I, Storhaug K, Sandvik L, Nordgarden H (2012) Severe tooth wear in Prader-Willi syndrome. A case–control study. BMC Oral Health 12: 12.
- Goldman SE, Bichell TJ, Surdyka K, Malow BA (2012) Sleep in children and adolescents with Angelman syndrome: association with parent sleep and stress. J Intellect Disabil Res 56: 600-608.
- Carra MC, Macaluso GM, Rompré PH, Huynh N, Parrino L, et al. (2010) Clonidine has a paradoxical effect on cyclic arousal and sleep bruxism during NREM sleep. Sleep 33: 1711-1716.
- Lobbezoo F, Lavigne GJ, Tanguay R, Montplaisir JY (1997) The effect of catecholamine precursor L-dopa on sleep bruxism: a controlled clinical trial. Mov Disord 12: 73-78.
- Cahlin BJ, Hedner J, Dahlström L (2017) A randomised, open√ʬ?¬źlabel, crossover study of the dopamine agonist, pramipexole, in patients with sleep bruxism. J Sleep Res 26: 64-72.
- Raigrodski AJ, Mohamed SE, Gardiner DM (2001) The effect of amitriptyline on pain intensity and perception of stress in bruxers. J Prosthodont 10: 73-77.
- Malcmacher L (2015) Bruxism-Are you helping or hurting your patients? J N J Dent Assoc 86: 14-16.
- Guaita M, Högl B (2016) Current treatments of bruxism. Curr Treat Options Neurol 18:10.
- Kostrzewa-Janicka J, Jurkowski P, Zycinska K, Przyby√?¬?owska D, Mierzwi√?¬?ska-Nastalska E (2015) Sleep-Related Breathing Disorders and Bruxism. Adv Exp Med Biol 873: 9-14.
- Sjöholm TT, Lowe AA, Miyamoto K, Fleetham JA, Ryan CF (2000) Sleep bruxism in patients with sleep-disordered breathing. Arch Oral Biol 45: 889-896.
- Saito M, Yamaguchi T, Mikami S, Watanabe K, Gotouda A, et al. (2014) Temporal association between sleep apnea–hypopnea and sleep bruxism events. J Sleep Res 23: 196-203.
- Nashed A, Lanfranchi P, Rompré P, Carra MC, Mayer P, et al. (2012) Sleep bruxism is associated with a rise in arterial blood pressure. Sleep 35: 529-536.
- Chowdhury T, Bindu B, Singh GP, Schaller B (2017) Sleep disorders: Is the trigemino-cardiac reflex a missing link? Front Neurol 8: 63.
- Schaller B (2004) Trigeminocardiac reflex. A clinical phenomenon or a new physiological entity? J Neurol 251: 658-665.
- Chowdhury T, Sandu N, Meuwly C, Cappellani RB, Schaller B (2014) Trigeminocardiac reflex: differential behavior and risk factors in the course of the trigeminal nerve. Future Neurol 9: 41-47.
- Yap AU, Chua AP (2016) Sleep bruxism: Current knowledge and contemporary management. J Conserv Dent 19: 383-389.
- Tuna SH, Celik OE, Ozturk O, Golpinar M, Aktas A, et al. (2017) The effects of stabilization splint treatment on the volume of masseter muscle in sleep bruxism patients. Cranio 18: 1-8.
- FDA Form 3881(2016) Department of Health and Human Services, USA.
- FDA Form 3881(2013) Department of Health and Human Services, USA.
- Ohmori H, Kirimoto H, Ono T (2012) Comparison of the physiological properties of human periodontal-masseteric reflex evoked by incisor and canine stimulation. Front Physiol 3: 233.
- Louca C, Cadden SW, Linden RW (1996) The roles of periodontal ligament mechanoreceptors in the reflex control of human jaw-closing muscles. Brain Res 731: 63-71.
- Brodin P, Türker KS, Miles TS (1993) Mechanoreceptors around the tooth evoke inhibitory and excitatory reflexes in the human masseter muscle. J Physiol 464: 711-723.
- Landry-Schönbeck A, de Grandmont P, Rompré PH, Lavigne GJ (2009) Effect of an adjustable mandibular advancement appliance on sleep bruxism: a crossover sleep laboratory study. Int J Prosthodont 22: 3.
- Berry RB, Brooks R, Gamaldo CE, Harding SM, Lloyd RM, et al. (2016) The AASM manual for the scoring of sleep and associated events: Rules, terminology and technical specifications, Version 2.3. American Academy of Sleep Medicine, Darien, Illinois, USA.
- Giannakopoulos NN, Schindler HJ, Rammelsberg P, Eberhard L, Schmitter M, et al. (2013) Co-activation of jaw and neck muscles during submaximum clenching in the supine position. Arch Oral Biol 58: 1751-1760.
- Hellmann D, Giannakopoulos NN, Schmitter M, Lenz J, Schindler HJ (2012) Anterior and posterior neck muscle activation during a variety of biting tasks. Eur J Oral Sci 120: 326-334.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi