Short Communication, J Regen Med Vol: 10 Issue: 5
Sense the Smell of Beginning of Cytokine Storm: A Report on Study of Early Markers of the Complications
Vijay Bakhtar*
Department of Cardiology, Bakhtar Hospital, Amravati, Maharashtra, India
Corresponding Author: Vijay Bakhtar
Director of Bakhtar Hospital, Department of Cardiology, Amravati,, India
Tel: 08668324946
E-mail: ashwini2niar@gmail.com
Received: September 06, 2021 Accepted: September 20, 2021 Published: September 27, 2021
Citation: Bakhtar V (2021) Sense the Smell of Beginning of Cytokine Storm: A Report on Study of Early Markers of the Complications. J Regen Med 10:5.
Abstract
Coronavirus disease (COVID-19) is a new strain of coronavirus which is not ceasing to emerge its newer and newer variants with time. The virus has shown mutations which have been not witnessed by the globe before. The more we are encountering the, virus the more complications are coming forward. The example of which is COVID-19 second wave which was more devastating than the first wave; the Indian scenario during even worst. The mortality rates a level checked hospitalized patients was 10.5% which was about 40% higher than 7.2% mortality rate among the patients hospitalized during the pandemic first wave which was a situation of mourn in the country. The major contributing factor for this was the occurrence of cytokine storm. However, the association between factors and parameters that lead to the production of cytokine storm have not been studied in depth. Cytokine storm was not easily handleable in many parts of world which contributed to the mortality and morbidity in patients. The lesson learnt from second wave will help us to deal with this panic of the 3rd wave pandemic situation across the world. The present study is the first Indian study to highlights the impact of simple clinical which include fever and Lymphocyte count on cytokine storm diagnosis. To the best of our knowledge, present study is the first which establishes the role of fever and Lymphopenia as earliest biomarkers of cytokine storm. This study is of significance because if early intervention of cytokine storm is done effectively then we can overcome the complications of COVID-19 infection. A cheap, easily acquired biomarker is needed to identify severe disease among hospitalized patients at early stages. According to our results, recurrent fever/prolonged fever more than 7 days and low count of Lymphocyte are earliest markers for the forthcoming cytokine storm. Hence, recommends the study the use of fever and Lymphocyte count to start the interventions and not wait for the upregulations of IL-6 and down regulation of SpO2 which occurs in late stage.
Keywords: Cytokine Storm IL-6, Recurrent fever, Covid-19, SpO2, HRCT
Introduction
COVID-19 which is evolved as major health crises all over the world has led to major loss, be in terms of morbidity, mortality as well as GDP’s all over and is expected to on time to do so with the latest Delta plus variant. The mutant strains and their related signs and complications that are emerging in COVID-19 is a continuing challenge to medical health systems. However, the host cell immune response to the coronavirus is more or less the same which is in both the variants is an extreme inflammatory reaction, with fever and release of large amount of pro-inflammatory cytokines in an event known as “cytokine storm [1]. Some studies evaluating cytokine profiles from COVID-19 patients have shown that the cytokine storm is directly related with lung injury which ultimately results in multi-organ failure or tissue damage [2]. The findings of this short communication show the characteristics of patients who developed recurrent or prolonged fever and its association to cytokine levels and Lymphocyte count along with lung infection. The continuous high levels of cytokine and chemokine causes depletion in SpO2 and higher HRCT chest score which leads to poor prognosis in the patients.
Therefore, the aim of this study is to establish the basic clinical parameter of fever and reduced Lymphocytes count as an early marker to sense the risk of forthcoming cytokine storm, which if controlled at the inception itself, can reduce the COVID-19 associated complications and will increase the chances of patient’s recovery. To the best of our knowledge the present study is first on Indian population to examine the cytokine levels and prognosis of disease with Lymphopenia and fever so we can reduce the forthcoming complications. The study has evaluated the IL-6, SpO2, HRCT counts and their correlation with fever pattern and Lymphopenia.
Cascades of Events
The natural immune response of human body
The key players of human’s immune system are WBCs, which travel throughout the body via blood vessels. For acting against invading microbes, the body exchanges cells and fluids between blood and lymphatic system [3]. Each lymph node contains specific compartments where they encounter antigens. Thus, the incoming lymphatic vessels, immune cells and foreign particles enter the lymph nodes [3]. In the bloodstream, microbes and WBCs continue the cycle of immune responses and then regularly drift back into the lymphatic system. The immune cells gather, work, and serve to confront antigens in lymph nodes and the spleen [4].
Immune response against covid-19
In patients with COVID-19 infection, abnormal host response or overproduction of inflammatory markers are observed. SARS-CoV-2 virus is known to attack directly on T cells to cause their destruction [5]. In addition, WBCs count can differ especially the T cell count which causes Lymphocytopenia or Lymphopenia in COVID-19 disease. This results in the local production of extremely high levels of inflammatory markers including cytokines, chemokines and free radicals that cause severe damage to patient the lungs and other organs of human body [6].
When virus infect the lung cells through (angiotensin converting enzyme-2) receptor host’s natural immune response tries to suppress the infection in initial stage of fever which is up to 7 days [3]. Here host’s immune system, pro-inflammatory cytokines and antiinflammatory cytokines works together to kill off an invader and then settle down [3]. In cases of the prolonged fever or recurrence i.e. fever > 7 days or fever relapse in the second week of illness, the expression of inflammatory markers gets over excited and causes cytokine storm in patients via increase in IL-6, LDH, Ferritin, CRP counts etc. Which in extreme stages leads to organ failure.
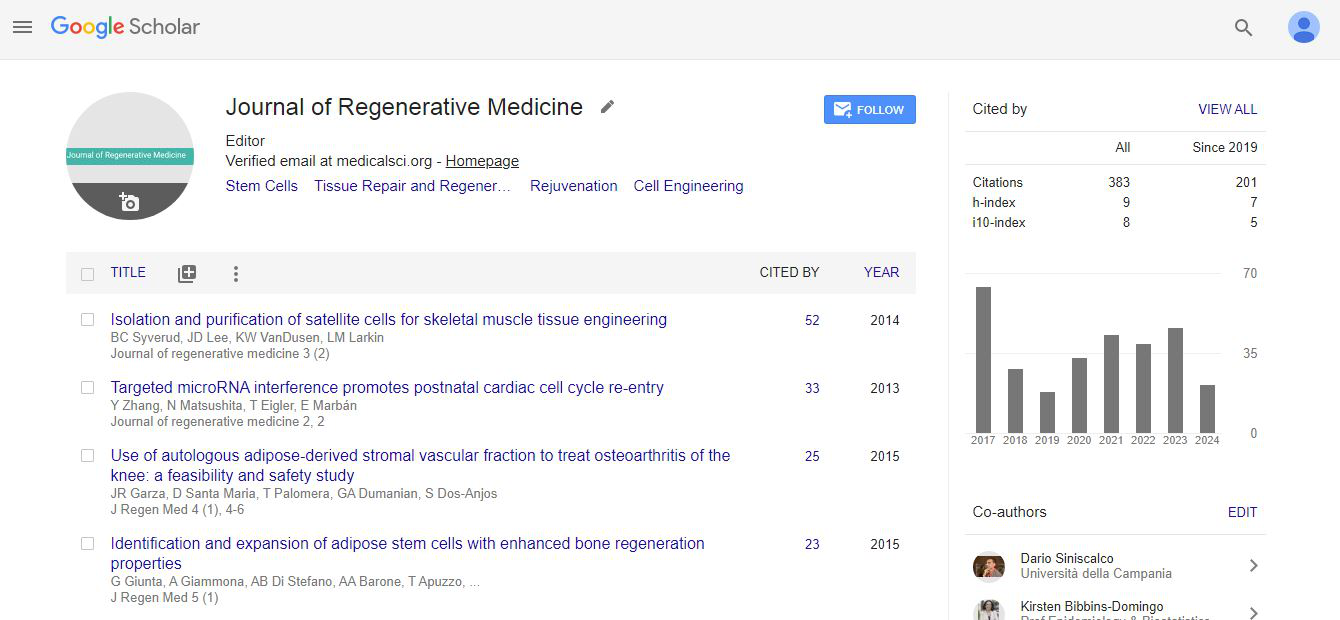
Clinically, the patient in the storm display marked reduction in SpO2 and increase in lung HRCT score. The SpO2 desaturation can also be explained by the fact that, in severe disease the patency of blood vessels gets thinner and thinner due to fluid escape and also due to the vigorous cellular migration (T cell) at the site of injury (Figure 1). Thus, only RBCs with increase amount of Ferritin, platelets and other components of blood remain in the blood vessel which leads to increased clotting of blood inside the vessel. Blood clotting impact on blood flow in the different regions of the lung and other tissues of body leading severe hypoxia [7]. Hence, the patients suffer from low oxygen saturation i.e. decreased SpO2 less than 90%. COVID-19 infection causes pneumonia which is characterized mainly by fever, cough, dyspnea, and bilateral infiltrates on chest imaging which is measured via HRCT chest [8]. High HRCT chest count indicates high viral load in patients (Figure 2). The SARS CoV-2 can block the host immune defence response by conquering T cell functions by inducing their programmed cell death i.e. apoptosis [6]. As its mention earlier in the article, the low count of Lymphocytes which causes Lymphopenia in COVID-19 (Figure 1). The low Lymphocyte count in COVID-19 infection is related with increased disease severity.
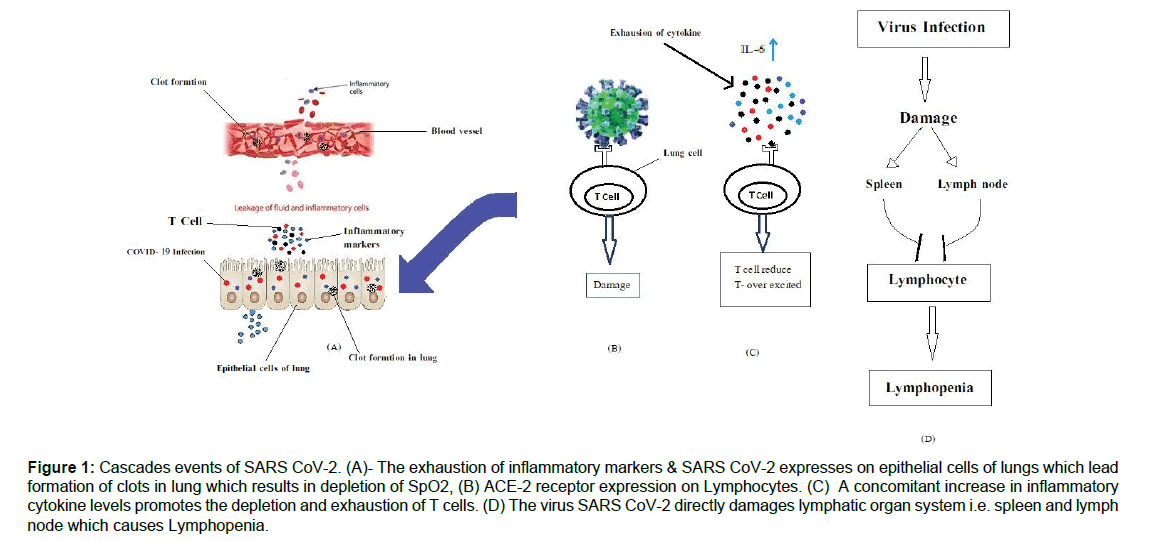
Figure 1: Cascades events of SARS CoV-2. (A)- The exhaustion of inflammatory markers & SARS CoV-2 expresses on epithelial cells of lungs which lead formation of clots in lung which results in depletion of SpO2, (B) ACE-2 receptor expression on Lymphocytes. (C) A concomitant increase in inflammatory cytokine levels promotes the depletion and exhaustion of T cells. (D) The virus SARS CoV-2 directly damages lymphatic organ system i.e. spleen and lymph node which causes Lymphopenia.
Figure 2: The graphical representation shows the, severity of patients depending on low SpO2 and Lymphocytes.
Methodology
Data collection and clinical management
We conducted a hospital-based case–control study of patients, who were admitted to tertiary health care center, Amravati, Maharashtra, (India). With a positive SARS-CoV-2 reverse transcriptase polymerase chain reaction (RT-PCR) assays from date 01-August-2020 to 03-July-2021.
Upon admission, all patients underwent a High-resolution computed tomography chest (HRCT-chest), Complete Blood Count (CBC). Renal and liver panel, C- Reactive Protein (CRP), Lactate dehydrogenase (LDH), Interleukin -6 (IL-6), Ferritin, through clinical laboratory findings at regular intervals till discharge.
SARS-CoV-2 PCR, patients who tested positive were not discharged until they had 2 negative RT-PCR test, 24 hours apart. Standardized template was used for recording daily signs and symptoms, vital signs and treatment offered. Serial CBCs and HRCT chest was done for those with prolong/recurrent fever and the records were collected. For cases with prolonged fever, examinations were repeated at a point of fever recurrence.
Results
We screened total 1324 patients who were admitted to Tertiary health care center Amravati, Maharashtra (India), from 01 Aug 2020 to 03 July 2021. Out of these 156 patients were excluded from the primary analysis as they had no symptoms. Data was collected from the remaining 1168 (88.21%) patients as control and they divided in two groups i.e. patients with prolonged/recurrent fever (Group-A) 23.79% (315/1324) and patients with short duration of fever (Group-B) and 64.27% (853/1324). All the Group-A patients showed significantly higher levels of the inflammatory parameters tested. These include C-Reactive Protein, Lactate dehydrogenase, Interleukin-6, and Ferritin, on the other hand the Lymphocyte count was significantly lower in the patients with prolonged/recurrent fever compared those with control and the short duration of fever (Table 1).
Table 1: Demographic and Clinical laboratory features of Prolonged/recurrent and short duration of fever in COVID-19.
The Figure 2 represented, the cases with group-A i.e. recurrent/ prolonged fever were more likely to have hypoxia 90% as compared with short duration of fever and control. The higher HRCT chest indicates the viral load in COVID-19 and severe pneumonia in patients. The cytokine and chemokines which are LDH, CRP, Ferritin, and IL-6 were found significantly high in prolonged/recurrent fever. Moreover, the average Lymphocyte count was observed to be 16% in Group-A patients and 21% in Group-B patients which denotes significant low levels in patients with prolonged/recurrent fever compared to control. Thus, the study establishes oxygen saturation, HRCT chest score, inflammatory cytokines levels are significantly associated with recurrent/prolonged fever.
Conclusion
With the evolving fear of delta plus variant which is spreading it using’s throughout the world; the experiences from the first and second wave in diagnosis, prognosis and treatment of COVID-19 will help us to increase our preparedness for the forthcoming complications.
The present study recommends to consider prolonged fever >7 days or recurrent i.e. fever in the second week of disease as well, dropping Lymphocyte counts as the warning signals for cytokine upregulation and treatment should be given accordingly. One must not wait for actual cytokine levels to increase which can further lead to undesired disease outcome.
The above recommendation is of significance because, if the treatment with steroids and immunomodulators including Tocilizumab is offered at the advent of recurrent fever itself then, the further complications of cytokine storm can be avoided and thus mortality rate will be controlled.
References
- Ragab D, Eldin HS, Taeimah M (2020) The Covid-19 cytokine storm; What we know so far. Front Immunol 11:1446.
- Huong C, Wang Y, Li X (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497-506.
- Chowdhury MA, Hossain N, Kashem MA (2020) Immune response in Covid-19: A review. J Infect Public Health 13: 1619-1629.
- Marie-Paule Lefranc (2020) IMGT teaching resources for immunology and immunogenetics
- Yang Li, Liu S, Liu J (2020) Covid-19: Immunopathogenesis and Immunotherapeutics. Springer Nature 5:128.
- Mortaz E, Tabarsi P, Varahram M (2020) The Immune Response and Immunology of Covid-19. Front Immunol 11: 1-9.
- Colarossi J (2020) Three Reasons Why COVID-19 Can Cause Silent Hypoxia. Bostern University.
- Jacob H, Vitor M, Jason H. Modeling lung perfusion abnormalities to explain early Covid-19 hypoxia. Nature Communication 11(1): 4883.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi