Perspective, Int J Ophthalmic Pathol Vol: 11 Issue: 2
Review of Patients with Various Types of Uveitis Showed that Abnormal Values of Blood Counts
Manthena Sravani*
Department of Ophthalmology, Osmania University, Hyderabad, India
*Corresponding author: Aruna Krupa, Department of Chemistry, Osmania University, Hyderabad, India, E-mail: sharat_r@gmail.com
Received date: 07 January, 2021, Manuscript No. IOPJ-22-60540;
Editor assigned date: 09 January, 2021, Pre QC No. IOPJ-22-60540 (PQ);
Reviewed date: 23 January, 2021, QC No IOPJ-22-60540;
Revised date: 28 January, 2021, Manuscript No. IOPJ-22-60540 (R);
Published date: 07 February, 2021, DOI: 10.4172/2324-8599.11.2.8
Abstract
Description
In practice, determination of an underlying aetiology is a routine and important step in the assessment and evaluation of a uveitic patient. 40-86% of patients have an underlying cause ranging from infectious to autoimmune causes, whilst the rest remains classified as idiopathic when no apparent cause can be identified, but the condition responds to standard anti-inflammatory therapy. Whilst anti-infective agents do not alter the course or outcome of autoimmune or non-infective uveitis, such therapy has no deleterious effects per se on the condition except that of prolonged and untreated non-infectious inflammation.
Conversely, the use of anti-inflammatory and immunosuppressive agents in infective uveitides is potentially devastating. As such, differentiation is crucial and defining infectious versus non-infectious causes is vital from the outset. Given the advances in molecular and cellular pathology and diagnostic ability ranging from laboratory to radiological tests (including X-rays, Computed Tomography (CT) scans, Magnetic Resonance Imaging (MRI) scans, Positron Emission Tomography (PET) scans and nuclear imaging), we are more enabled to make such diagnoses. In this review, we will focus on the laboratory, blood and immunological tests, and these will be further discussed.
Infective uveitides vary in prevalence according to geographic regions. Uveitides that were previously ‘undiagnosed’, labeled and treated as ‘idiopathic’ are increasingly recognized as related to, or directly caused by an infective cause as a result of progress in diagnostic techniques. For example, cytomegalovirus detection in aqueous with resultant therapeutic responses to antiviral agents have led to improved therapeutic outcomes in hypertensive uveitic entities such as related syndromes for example, Posner-Schlossman syndrome. Fuchs’ heterochromic iridocyclitis has also been linked to some herpes viruses and Rubella, and Tuberculosis-related intraocular inflammation has seen resurgence in diagnosis following the development of newer diagnostic techniques.
Role of Diagnostic Tests
Diagnostic tests in search for aetiology in intraocular inflammatory diseases have always been controversial, mainly due to its history of suspected lack of specificity and sensitivity of assays. Such views have therefore led to the concept that the need for detecting infectious agents or underlying inflammatory disease, whether for clinical or research purposes, to deliver improved and more tailored diagnosis or understanding of mechanisms of inflammatory disease must be balanced against the cost of the investigations, the available resources of the treating center, the utility of the tests employed (given potential lack of sensitivity of assays) and finally, and particularly so in acute circumstances, the time taken to obtain results. This is in contrast to performing tests for the overall systemic health of the individual prior to commencement of immunosuppression that can further compromise health. In a wider perspective, traditionally a “textbook” list of relatively untailored investigations remains costly and may not until recently, contribute to either diagnosis or change in management.
According to the classification criteria from the European-American collaboration, secondary SS (sSS) consists of features of primary SS (pSS) together with features of an overt autoimmune connective tissue disease, the most common of which is rheumatoid arthritis. There is a well-known association of several systemic diseases with dry eye syndrome such as SS, rheumatoid arthritis, scleroderma, polymyositis, lymphoma, amyloidosis, hemochromatosis, sarcoidosis, and systemic lupus erythematous. Although the rate of dry eye in various inflammatory diseases is known, the frequency of associated systemic rheumatic conditions in patients with dry eye is currently unknown. A previous retrospective study from a single tertiary eye care center determined that pSS is underdiagnosed and should be the focus of diagnostic evaluations in individuals with clinically significant aqueous deficient dry eye. Only 33.3% of patients with pSS carried the diagnosis at the time of presentation and 50% were diagnosed as a result of the initial evaluation. A more recent multicenter prospective study confirmed these findings in a group of more than 300 patients with clinically significant dry eye and found the rate of SS to be 11.6%. The difference in the rate of SS between these two studies could perhaps be attributed to the fact that the prospective study was limited in regards to the diagnostic tests performed: minor salivary gland biopsy or tests for objective dry mouth findings were not utilized. Nonetheless, both studies concluded that ophthalmologists managing patients with clinically significant dry eye should have a high index of suspicion for underlying SS and a low threshold for diagnostic work-up.
Previously unrecognized autoimmune thyroid disease has also been shown to be a cause of inflammatory ocular surface disease with dry eye symptomatology and should be considered when evaluating patients with dry eye. A retrospective, observational case series of 539 patients referred for dry eye evaluation has confirmed this correlation; of the 32 patients who underwent standardized orbital echography with a clinical suspicion, 21 (66%) were diagnosed with occult thyroid eye disease.
Review of Patients
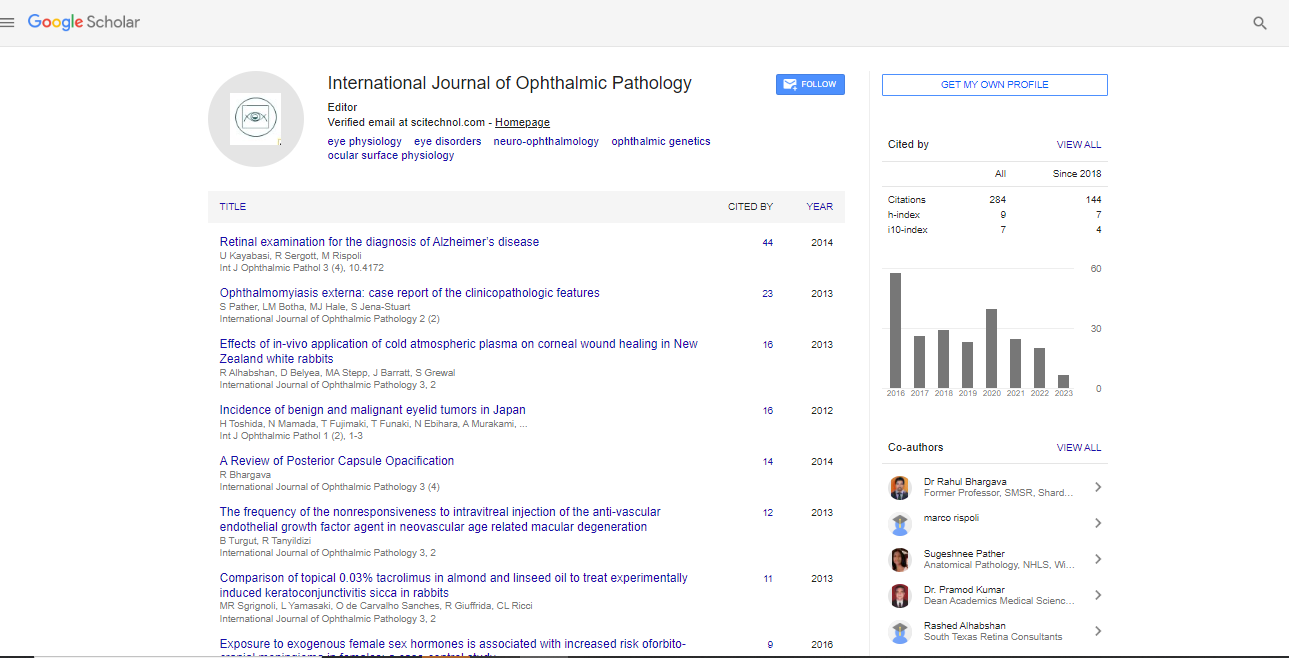
A retrospective review of patients with various types of uveitis showed that abnormal values of complete blood counts, plasma viscosity/Erythrocyte Sedimentation Rate (ESR) and VDRL/TPHA did not contribute to establishing an underlying cause of the uveitis. Canadian surveys demonstrated that most routine tests performed for the investigation of anterior uveitis lack sensitivity and specificity and have low diagnostic yields. In general, investigations are uncommonly performed for anterior uveitides alone except in specific circumstances e.g. chronic or recurrent disease, unresponsive or worsening with anti-inflammatory treatment or in hypertensive anterior uveitides. On the other hand, patients with intermediate and posterior uveitides, or those patients that present with systemic symptoms and manifestations are usually investigated with a panel of screening tests that comprise an autoimmune and infective screen that typically include syphilis and tuberculosis- two infections that have protean as well as overlapping ocular manifestations. Further investigations with blood tests, imaging, molecular diagnosis of aqueous or vitreous samples, or biopsy depend on the clinical presentation of the disease.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi