Research Article, Int J Ment Health Psychiatry Vol: 4 Issue: 1
Psycho-emotional Factors and Their Role in Craniomandibular Disorders
Lumini�?�?a Albert1*, Camelia Stanciu2, Cristian Delcea3, Adriana Mihai1 and Sorin Pop�?�?or1
1University of Medicine and Pharmacy Târgu Mure�?�?, Romania
2Dimitrie Cantemir University of Târgu Mure�?�?, Romania
3Victor Babe�?�? University of Medicine and Pharmacy, Timi�?�?oara
*Corresponding Author : Lumini�?�?a Albert
B-ul 1 Dec 1918, No. 186, Ap 5, Târgu Mure�?�?, Mure�?�?, Romania
Tel: +0040751351922
E-mail: albertluminita04@gmail.com
Received: December 07, 2017 Accepted: January 15, 2018 Published: January 22, 2018
Citation: Albert L, Stanciu C, Delcea C, Mihai A, Pop�?�?or S (2018) Psycho-emotional Factors and Their Role in Craniomandibular Disorders. Int J Ment Health Psychiatry 4:1. doi: 10.4172/2471-4372.1000156
Abstract
Introduction: The present study emphasizes the importance of psycho-emotional factors as predisposing factors in craniomandibular disorders. The actual etiology of craniomandibular disorders remains relatively obscure, factors that contribute to the development of dysfunction in its various stages are not well-defined. Their systematization into predisposing etiological factors, initiators and perpetuates actually supports the pluricausal and often idiopathic character of this condition.
Material and method: The study included an experimental group of 30 subjects diagnosed with major depressive episode, women aged 41 to 71 and 30 subjects, women of the same age range who did not qualify for this diagnosis, based on DSM V criteria and the results obtained in the BDI-2 questionnaire (Beck Depression Inventory - 2). The two groups were given the Craniomandibular Dysfunction Screening Questionnaire.
Results: Between the two lots there is a statistically significant difference in the over all score of the scale, which determines the tendency or predisposition for the development of the craniomandibular dysfunction. To analyze the relationship between the presence of a psychiatric diagnosis and the level of somatic pain experienced, we used the calculation of the Pearson correlation coefficient between the values obtained by subjects at BDI-II and the Somatic Pain Scale. The obtained results indicated the existence of a statistically significant positive correlation. The calculation of the Pearson correlation coefficient between the values obtained by subjects at BDI-II and the Psychoemotional Suffering Scale indicates the existence of a statistically significant positive correlation.
Conclusion: By analyzing comparatively two batches (one clinical and one nonclinical) in terms of risk of this disorder, the results indicated that a psychiatric diagnosis - in this case the major depressive episode may be a predisposing factor for this disorder. This risk did not occur in the nonclinical group.
Keywords: Craniomandibular disorder; Pain; Major depressive episode; Psychological distress
Introduction
Conceptual delimitations
Craniomandibular Disorder or Dysfunction (CMD) is briefly described as a «collective term that includes a number of clinical problems in masticatory muscles, temporomandibular joints and associated structures» [1]. This is a pathophysiological entity characterized by pain in the cheek muscles and temporomandibular joints, articular noises, limitations or atypical traces of mandibular kinematics at the opening of the mouth.
Symptomatically characterized by the triad of pain in the temporomandibular joints region and the masticatory muscles, the limitation of mandibular kinematics and noises in the temporomandibular joints in their mobilization, this pathophysiological state is approached in the literature under different names, all reflecting essentially the same pathology.
Prevalence
The literature on the prevalence of CMD varies and is addressed in different ways. Some studies consider that 75% of the population has at least one sign of craniomandibular dysfunction and about 33% have at least one characteristic symptom of dysfunction [2]. However, despite the significant percentages of the general population showing signs and symptoms of CMD, it is estimated that only 2-16% of them required treatment [3]. Linda Le Resche presented the results of an epidemiological reference study on the subject from which it appears that 50-60% of the population show a sign and / or significant damage to the masticatory system and 8-15% of women and 3-10% of men experience symptoms that are severe enough to require treatment [4].
Predisposing factors
The predisposing factors for CMD is on the one hand pathophysiological changes in systemic neurological, rheumatologic, vascular, metabolic, hormonal, digestive, infectious and neoplastic diseases.
On the other hand, it is predisposing to craniomandibular dysfunction psychological factors represented by emotional, personality and behavioral attitudes (stress, anxiety, depression), factors that also contribute to the evolution of the disease.
Finally, in the category of predisposing factors an important role is attributed to the structural elements (genetic, developmental and iatrogenic). The ligament hyperlaxity, biochemical changes of synovial fluid and joint lubrication, irregularities of the temporomandibular joint joint surfaces are frequently recalled as predisposing factors for arthrogenic dysfunctions such as reductible and irreducible meniscal dislocations.
Psychological stress and the psychosocial adaptation of the patient are incriminated conditions in determining the installation of a myogenic craniomandibular dysfunction [5].
A number of authors, such as Velly, consider depression and chronic pain as a widespread (generalized) risk factor in triggering CMD [6].
A series of topical studies in literature emphasizes the role of psychological stress in triggering and maintaining the myogenic craniomandibular disorder.
Research by Kindler S, Samietz S, Houshmand M has shown that depressive and anxious symptoms are risk factors for triggering temporomandibular pain [7].
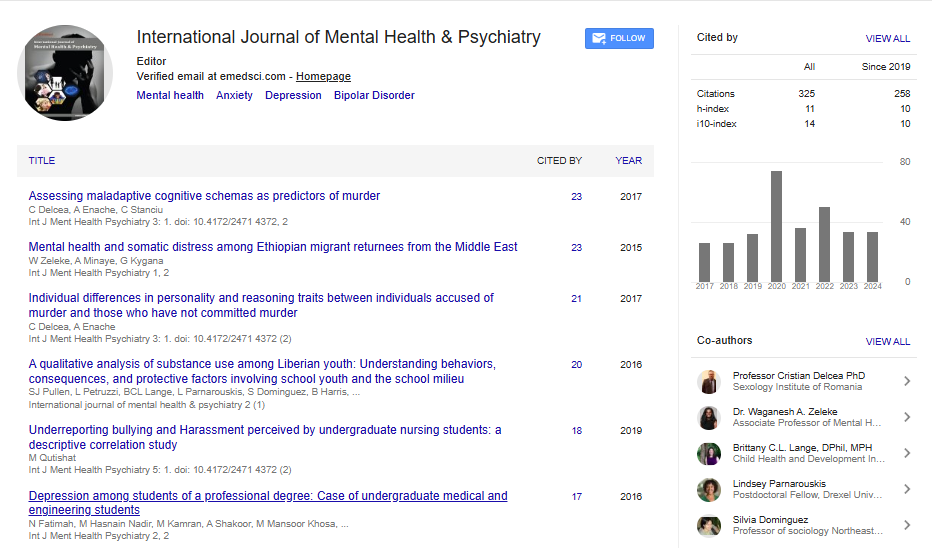
The following (Figure 1) shows CMD as a result of the interaction of physical and genetic factors with the environment.
Treatment should be directed early on, not only on the dysfunction and pain associated with it, but also on the psychosocial factors that contribute to and perpetuate the disorder. The combined role of physical and psychosocial factors in the development of craniomandibular dysfunctional syndrome, especially its myogenic variant, is currently unanimously accepted by specialists [8].
Objective of the Research
The present study aims at analyzing the correlation between the level of depression and the risk of craniomandibular disorder.
Sample and Evaluation Tools
The study included an experimental group of 30 subjects diagnosed with major depressive episode, women aged 41 to 71 and 30 subjects, women of the same age range who did not qualify for this diagnosis, based on criteria DSM V and the results obtained in the BDI-2 questionnaire (Beck Depression Inventory - 2).
The following histograms shows the age distribution of the two batches (Figures 2 and 3).
The two groups were given the Craniomandibular Dysfunction Screening Questionnaire, which included 20 items evaluating pain, dysfunction, parafunction, emotion, trauma / irritation.
The results of the subjects were interpreted using the statistical SPSS version 16.1.
Result and Discussion
We compared the results obtained in the Screening Questionnaire for the mandibular dysfunction of the two batches that were compared with the t test for independent samples (Table 1).
| Group Statistics | |||||
|---|---|---|---|---|---|
| DG1 | N | Mean | Std. Deviation | Std. Error Mean | |
| scorglob1 | 1,00 | 30 | 8,8000 | 2,45511 | ,44824 |
| 2,00 | 30 | 2,0333 | 1,03335 | ,18866 | |
Table 1 : The statistical data of the investigated groups and their comparation.
Between the two lots there is a statistically significant difference in the overall score of the scale, which determined the tendency or predisposition for the development of the craniomandibular dysfunction. The value t (13.9) is significant at p<0.01.
The histogram below shows the averages of the two lots at the Global Scale Score (Figure 4).
To analyze the relationship between the presence of a psychiatric diagnosis and the level of somatic pain experienced, we used the calculation of the Pearson correlation coefficient between the values obtained by subjects at BDI-II and the Somatic Pain Scale. The obtained results indicated the existence of a statistically significant positive correlation at p = 0.01 (Table 2).
| Independent Samples Test | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Levene's Test for Equality of Variances | t-test for Equality of Means | |||||||||
| F | Sig. | t | df | Sig. (2-tailed) | Mean Difference | Std. Error Difference | 95% Confidence Interval of the Difference | |||
| Lower | Upper | |||||||||
| scorglob1 | Equal variances assumed | 20,079 | ,000 | 13,914 | 58 | ,000 | 6,76667 | ,48633 | 5,79318 | 7,74015 |
| Equal variances not assumed | 13,914 | 38,962 | ,000 | 6,76667 | ,48633 | 5,78295 | 7,75039 | |||
Table 2: Correlations between the Depression Scale score and the perceived somatic pain.
In other words, the higher the score on the Depression Scale, the higher the perceived somatic pain.
The calculation of the Pearson correlation coefficient between the values obtained by subjects at BDI-II and the Psychoemotional Suffering Scale indicated the existence of a statistically significant positive correlation at p = 0.01 (Table 3). The higher the score on the Depression Scale, the higher the perceived emotional distress at the subjective level.
| BDI1 | PSIHOEMOT | ||
|---|---|---|---|
| BDI1 | Pearson Correlation | 1,000 | ,812** |
| Sig. (2-tailed) | ,000 | ||
| N | 60,000 | 60 | |
| PSIHOEMOT | Pearson Correlation | ,812** | 1,000 |
| Sig. (2-tailed) | ,000 | ||
| N | 60 | 60,000 |
Table 3: Correlations between the Depression Scale score and the perceived emotional distress.
The literature suggests that there is a multifactorial etiology for CMD, as well as predisposing factors. A number of authors have turned to prospective studies and have shown the importance of risk factors such as psychological profile and the presence of pain with localizations other than the orofacial region [9].
The present study seeks a plea for the importance of psychoemotional factors as predisposing ones to CMD.
Conclusion
By analyzing comparatively two batches (one clinical and one nonclinical) in terms of risk of this disorder, the results indicated that a psychiatric diagnosis - in this case the major depressive episode may be a predisposing factor for this disorder. This risk did not occur in the nonclinical group.
We recommend the introduction into the psychotherapeutic program addressed to patients diagnosed with major depressive episode and progressive muscle relaxation training or electromyographic biofeedback.
Acknowledgement
In this article, all the authors have equal contributions.
References
- De Leeuw R (2008) Orofacial pain: Guidelines for assessment, diagnosis and management. Chicago: Quintessence Publishing Co, United States.
- Rinchuse DJ, McMinn JT (2006) Summary of evidence –based systematic reviews of temporomandibular disorders. Am J Orthod Dentofacial Orthop130: 715-720.
- Kuttila M, Niemi PM, Kutilla S, Alanen P, Le Bell Y (1998) TMD treatment need in relation to age, gender, stress and diagnostic subgroups. J Orofac Pain 12: 67-74.
- Le Resche L (1997) Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med 8: 291-305.
- Epker J, Gatchel RJ, Ellis E (1999) A model for predicting chronic TMD: Practical application in clinical settings. J Am Dent Assoc 130: 1470-1475.
- Velly AM, Look JO, Schiffman E, Lenton PA, Kang W et al (2010) The effect of fibromyalgia and widespread pain on the clinically significant temporomandibular muscle and joint pain disorders- A prospective 18-month cohort study. J Pain 11: 1155-1164.
- Kindler S, Samietz S, Houshmand M, Grabe HJ, Bernhardt O et al (2012) Depressive and Anxiety Symptoms as Risk Factors for Temporomandibular Joint Pain: A Prospective Cohort Study in the General Population. J Pain 13: 1188-1197.
- Pop�?�?or S, Coman Lia, Szasz O (2002) Orient�?�?ri diagnostice �?�?i terapeutice în disfunc�?�?ia craniomandibular�?�?. Ed. University Press Tîrgu Mure�?�?, Romania.
- Garofalo JP, Gatchel RJ, Wesley AL, Ellis E 3rd (1998) Predicting chronicity in acute temporomandibular joint disorder using the research diagnostic criteria. J Am Dent Assoc 129: 438-447.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi