Research Article, J Regen Med Vol: 12 Issue: 1
Prospective Randomised Study Comparing Outcome Case of Hemorrhoids After LigaSure and Stapler
Hassan A Saad1*, Adel Mahmoud Moursi1, Kamal Rabie2, Hassan Ashour1, Mohamed E Eraky1, Ahmed M Yehia1
1Department of General Surgery, Zagazig university, Zagazig, Egypt
2Faculty of Medicine, Al-Azhar University, Nasr City, Egypt
*Corresponding Author: Hassan A Saad
Department of General
Surgery, Zagazig university, Zagazig, Egypt
Tel: 01221025689
E-mail: ebramos_2010@yahoo.com
Received: 05-January-2023, Manuscript No. JRGM-23-85487;
Editor assigned: 07-January-2023, PreQC No. JRGM-23-85487
(PQ);
Reviewed: 21-January-2023, QC No. JRGM-23-85487;
Revised: 23-January-2023, Manuscript No. JRGM-23-85487 (R);
Published: 27-January-2023, DOI:10.4172/2325-9620.1000236
Citation: Saad HA, Moursi AM, Rabie K, Ashour H, Eraky ME, et al. (2023) Prospective Randomised Study Comparing Outcome Case of Hemorrhoids After LigaSure and Stapler. J Regen Med 12:1.
Abstract
Aim: It has been shown that for the diathermy and scissor have harmful effect and complicated of pain that little with Harmonica and Ligasure in anal surgery especially hemorrhoidectomy ,so in this study we compare the LigaSure with this stapling debate.
Methods: 50 patients had 3rd to 4th degree piles were grouped to undergo LigaSure™ or stapling hemorrhoidopexy for piles hemorrhoidectomy. In zagazig university surgical department. Parameters investigated pain, satisfaction or residual and recurrence, also post operative course and analgesia
Results: Equal results in all most analyzed of both groups. Patient satisfaction (P value = 1), Postoperative pain scores (P value=0.99), and self activity satisfaction (P value = 0.99). No major difference except in investigations.
Conclusion: Two methods cane be used safely in two groups.
Keywords: Technical handling; Hemorrhoidectomy; Patient work recovery.
Keywords
Technical handling; Hemorrhoidectomy; Patient work recovery
Introduction
Using the diathermy and dissector may be the cause of pain and harmful effect on the tissue henceforth the operation can be very painful [1-2] and take long time for healing and suffering upto more than 6 weeks [3]. This has initiated the surgeons to create or develop new techniques and modifications to decrease the pain and rapid recovery.
Operations with stapler has advantage of less operative pain and rapid recovery than the diathermy and scissor cutting hemorrhoidectomy or scissors cutting methods [4-11], but it is difficult to be used in fourth degree piles, and/or more skin appendages so, diathermy suitable for cutting without pain limitation [12]. and one of its disadvantage is recurrence.
Diathermy or LigaSur are not limited by amount of tissue so, both were used in patients with 4th degree piles or excess skin tag and little pain resuting both stapler and Ligasure than ordinary methods, the aim of this work is to determine ideal methods with little pain, easy techniquic application with advanced cases of piles.
Materials and Methods
We had 50 patients suffering from symptomatic 3rd and 4th degree piles in zagazig university surgical department. According to ethics in our study all patients were signed on ethics approval. Patients were divided to group 1 randomised to be operated by stapler for piles excision(hemorrhoidectomy) (group 1, n = 25) or group 2 by LigaSure™ technique for piles excision( hemorrhoidectomy) (group 2, n = 25). All subjected to the power test; standard deviation (SD) done in 20 patients of each group in mean pain score, with 80 % power at 5 % of the level were noticed differences.
For patient characteristics, refer to Table 1. 5 cases 4 of group (1), 1 of group (2) were removed as the follow up examinations couldn’t be done as their accomodations are far from the hospital which is more than 30 km, remaining 5 were recruited.
| LigaSure | Stapler | |
|---|---|---|
| No. | 25 | 25 |
| Mean age | 48(28-82) | 11 |
| Female | 12 | 58 (40–71) |
Table 1. Patient characteristics.
Preoperative assessment
1.Full history
2.Examination including proctosigmoidoscopy.
3.Routine laboratory examination
According to finding proctosegmoidoscopy the procedure were done on a patients study from,
4.Unsuspected malignant mass or malignant ulcer, no differences in the distribution the hemorrhoid staging.
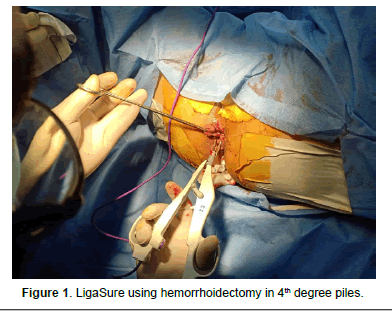
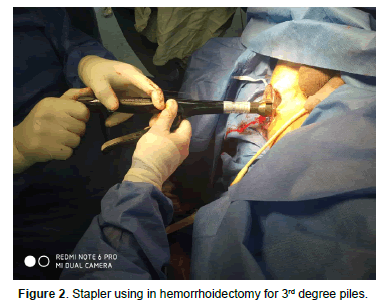
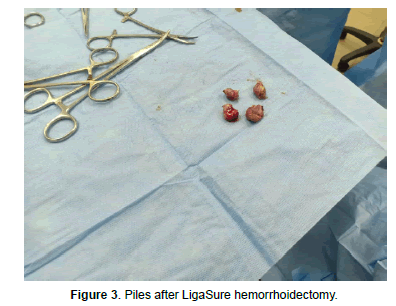
We used the Stapling as described before with the Proximate® PPH stapler, for residual prolapsing tissue or skin appendages. In 9 patients (36 %) the diathermy was used with stapler (Table 2,3). By Milligan- Morgan technique LigaSure™ hemorrhoidectomy was used. A small incision 2 cm was made at mucocutanous junction ;along the dermocutanous junction planes by LigaSure™ using the smaller instrument about (18cm). Six patients (24%) operated through this procedure and were proceeded to segmental plastic reconstruction if associated with prolapse piles (Fansler-Arnold). This procedure depending on skin and subcutaneous full thickness flab moving, to cover the defect with associated anal structure (rhomboid, trapezoid , con shape).
| LigaSure | Stapler | |
|---|---|---|
| Piles | 9 | 10 |
| 2nd to 3rd degree | 13 | 14 |
| 3rd degree only | 1 | 1 |
| 3rd to 4th. degree | 2 | 1 |
| 4th. degree only | ||
| Progress prolapse | ||
| partial prolapse | 15 | 10 |
| complete prolapse | 5 | 8 |
| Skin appendage | 7 | 10 |
| Fissure | 3 | 0 |
| Itching | 1 | 1 |
Table 2. Hemorrhoidal staging and associated finding.
| LigaSure | |
|---|---|
| Classic Milligan–Morgan | 19 |
| Additional procedure | |
| Plastic flab | 6 |
| Stapler | |
| Stapler | 16 |
| Another procedure | |
| Segmental Milligan–Morgan, or skin tags | 9 |
Table 3. Surgical procedures.
Operation time and intraoperative steps were detected on a questionnaire.
Routine postoperative analgesia eg. Diclofenac acid (3×50 mg) or ibuprofen (tid 400 mg) or Opiates in severe pain. Metronidazole 500mg tid tab were given. Patients were given routine laxative, during the hospital time and after discharge. Duration of pain and analgesic therapy were recorded during hospital time, from postoperative day 1 to 3weeks, the intentsity of pain is monitored ,their intake of analgesia, the recovery to personal activity percent, were recorded (0-100%), by visual analog scales from 0 to 10.
A follow-up was made up to six weeks including all history of pain (visual analog scale, 0-10) and level of personal activity (0-100%) all detected on a separate sheet patients, with a self good recovery.
At the end results, the duration of operating time was subjected to T-test , Pearson’s chi- squared test, statistical software R1.9.1 (ISBN 3-900051-05-4) are expressed by mean, median, and range near, in all groups. Wil- coxon two-sample test used for Statistical significance done on every day basis, then the P values were recorded.
Results
No significant differences was detected after operation (P = 0.19). Significance in duration of operation found in the the six cases with combined anodermal flap plasty and LigaSure™ hemorrhoidectomy, as technical handling was little complicated in 12 % , 24 %, respectively (P = 0.55) (Table 4). In post- operative assessment, results (Table 5) were controlled by the releive satisfaction in 96 % of the cases in the LigaSure™ of which 88 % was in the stapler group (P = 0.44), take attention without favourable level of significant advantage.
| LigaSure™ | Stapler | |
|---|---|---|
| Simple | 22 (88%) | 19 (76%) |
| Slightly -awkward | 2 (8%) | 4 (16%) |
| Associated complication | 1 (4%) | 2 (8%) |
P value = 0.5535.
Table 4. Immediate postoperative assessment of ease of handling by the surgeon.
| LigaSure | Stapler | |
|---|---|---|
| 23/26 (10–80) | 20/21 (6–54) | |
| Procedure | 18/20 (10–37) | 15/18 (6–40) |
| Combined procedure | 40/44 (20–80) | 25/25 (15–54) |
Values are median/mean (range). P value = 0.1858.
Table 5. Operative time.
In (Table 6) the course after all techniques were recorded, in terms of manner and timing of the first defecation. No significant differences in early operation l, complications, hospital duration time and analgesia was observed (Table 7). Median pain level scoring (Figure 1) and their near relationship between two groups and P value for two group after complete analyses is equal to 0.99. There was a tendency of the LigaSure™ patients preference. Mean patient satisfaction during the first 7 days (P = 1, Figure 2) and mean gain of personal recovery, activity and satisfaction (P = 0.99, Figure 3) were nearly the same in two groups.
| LigaSure | Stapler | |
|---|---|---|
| Early complication | ||
| Urine retened | 2(8%) | 4(16%) |
| Ozzing blood | 1(4%) | |
| All | 3 (12%) | 4 (16%) |
| Days: (mean range) | 2/3 (1–5) | |
| First defecation | ||
| Suppository/enema | 6(24%) | 8(42%) |
| Spontaneous | 19 (76%) | 17 (68%) |
| Hospital time | ||
| Days: median | 5/5 (2–10) | 4/4 (2–10) |
Table 6. Postoperative course.
| Opiate | 6 (24%) | 8 (32%) |
| Morphia | 1 (4%) | |
| After discharge analgesia | ||
| No | 3 (12%) | 2 (8%) |
| Panadol | 1 (4%) | 1 (4%) |
| Diclofenic A. | 6 (24%) | 5 (20%) |
| Tramadolic acid | 2 (8%) | 0 |
| Mean time range | 14 days | 16 days |
| Metroametazole, ibrufen and tramadol taken for all patients during hospital stay | ||
Table 7. Analgesic requirement.
Overall, the level of self recovery with treatment had no relation to the type of operative technique. The level of recover activity was clearly seen decreasing during the first few dayes up to 14 days, but the mean values increased gradually from 40 to 60 %. Mean of activity satisfaction levels of 80 % and above attained by the third week in the two groups, but at the six-week, no differences were found after follw up. In both groups, 84 % of patients had no complaints and any findings in examination. In 92% self recovery, with treatment still higher, and the level of recover activity was completely gained in most patients.
Discussion
Painful dissection, postoperative by diathermy or scissor by both LigaSure™ and stapler and alternatives proves in unselected patients with hemorrhoidal disease and postoperative good handling, less pain and good patients satisfaction [4-11, 13-16].
In fact, we found nearly postoperative pain level and patient self activity were same in two groups, but the investigations found that factors had no significant differences.
LigaSure™ is preferred in handling than stapler with respect to surgical equal of immediate postoperative result. The stapler apparent favorable in advanced cases (advanced fourth-degree piles). But LigaSure™ had favorable immediate relief than technical advantages of stapler and used only if more excision or skin or mucous tissue reconstruction, instead of painful diathermy (4th -degree piles).
So, Stapling is not eliminated and the main studies about stapler deal with these points. Some studies suspect that there are patients who are not suitable for stapling towards hemorrhoidal cases,but usually proved suitable coloproc- tologic service but are not suitable for daily using for these patients even for good easy grasping in 4th degree piles. By stapler remains difficult definition that fixed externally, so some prove the using of both stapler and surgry show good results and also used in the prolapsing and reducible piles(3rd degree) without any complications.
Both the methods are safe having their own advantages and disadvantages wuth good results and satisfaction in both treatment types (Figure 2). Irrespective of the operative method ther are manipulation in painful site. Nearly most patients recur activity without pain after inspection, 3 weeks later following the classic Milligan-Morgan-type technique which had 6 weeks compared to others methods of improvement median ranged degree of pain and personal self activity.
References
- Brisinda G, Civello IM, Maria G (2000) Hemorrhoidectomy: painful choice. Lancet, 355:2253.
- Engel AF, Eijsbouts QA (2000) Haemorrhoidectomy: painful choice. Lancet, 355:2253-2254.
- MacRae HM, McLeod RS (1995) Comparison of hemorrhoidal treatment modalities. A meta-analysis. Dis Colon Rectum, 38:687-694.
- Ganio E, Altomare DF, Gabrielli F, Milito G, Canuti S (2001) Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg, 88:669-674.
- Hasse C, Sitter H, Brune M, Wollenteit I, Lorenz W, et al. (2004) Haemorrhoidectomy: conventional exci- sion versus resection with the circular stapler. Prospec- tive, randomized study. Dtsch Med Wochenschr, 129:1611-1617.
- Ho YH, Cheong WK, Tsang C (2000) Stapled hemor- rhoidectomy–cost and effectiveness. Randomized, controlled trial including incontinence scoring, anorec- tal manometry, and endoanal ultrasound assessments at up to three months. Dis Colon Rectum, 43:1666-1675.
- Khalil KH, O’Bichere A, Sellu D (2000) Randomized clinical trial of sutured versus stapled closed haemorrhoidec- tomy. Br J Surg, 87:1352-1355.
- Kirsch JJ, Staude G, Herold A (2000) Longo and Milligan-Morgan hemorrhoidectomies. Surgeon, 72:180-185.
- Schmidt MP, Fischbein J, Shatavi H (2002) Stapler hemorrhoid-ectopy versus conventional procedures-a clinical study. Zentralbl Chir, 127(1):15-18.
- Shalaby R, Desoky A (2001) Randomized clinical trial of stapled versus Milligan-Morgan haemorrhoidectomy. Br J Surg, 88:1049-1053.
- Seow-Choen F (2001) Stapled haemorrhoidectomy: pain or gain. Br J Surg, 88:1-3.
- Chung YC, Wu HJ (2003) Clinical experience of sutureless closed hemorrhoidectomy with LigaSure. Dis Colon Rectum, 46:87-92.
- Franklin EJ, Seetharam S, Lowney J, Horgan PG (2003) Ran- domized, clinical trial of Ligasure vs. conventional diathermy in hemorrhoidectomy. Dis Colon Rectum, 46:1380-1383.
- Milito G, Gargiani M, Cortese F (2002) Randomised trial com- paring LigaSure haemorrhoidectomy with the diathermy dissection operation. Tech Coloproctol, 6:171-175.
- Thorbeck CV, Montes MF (2002) Haemorrhoidectomy: randomised controlled clinical trial of Ligasure compared with Milligan-Morgan operation. Eur J Surg, 168: 482-484.
- Rowsell M, Bello M, Hemingway DM (2000) Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled trial. Lancet, 355(9206):779-781.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi