Research Article, J Pharm Sci Emerg Drugs Vol: 11 Issue: 1
Preparation and Evaluation of Rosmarinic Acid Liposomes as an Ocular Delivery System
Ali Rahmani1* and Maedeh Dahaghin2
1Department of Pharmaceutical Biomaterials, Tehran University of Medical Sciences, Tehran, Iran
2Department of Medicinal Chemistry, Tehran University of Medical Sciences, Tehran, Iran
*Corresponding Author: Ali Rahmani
Department of Pharmaceutical
Biomaterials, Tehran University of Medical Sciences, Tehran, Iran
E-mail: rhmn.ali1996@gmial.com
Received date: 21 February, 2023, Manuscript No. JPSED-23-93841;
Editor assigned date: 23 February, 2023, Pre QC No. JPSED-23-93841(PQ);
Reviewed date: 07 March, 2023, QC No. JPSED-23-93841;
Revised date: 14 March, 2023, Manuscript No. JPSED-23-93841(R);
Published date: 24 March, 2023, DOI: 10.4172/2324-8955.1000126.
Citation: Rahmani A, Dahaghin M (2023) Preparation and Evaluation of Rosmarinic Acid Liposomes as an Ocular Delivery System. J Pharm Sci Emerg Drugs 11:1.
Abstract
Background: Cataract is considered the leading cause of visual impairment. Recently, Rosmarinic Acid (RA) shows potential benefits for pharmacologic treatment of cataract. Unfortunately, due to its low permeation to the lens, liposomes have been used to overcome of its solubility and improve efficiency.
Methods: In the current study, different formulations of liposome incorporating Sodium Deoxy Cholate (SDC) were prepared by ethanol-injection method. Liposomes were characterized by Dynamic Light Scattering (DLS), Scanning Electron Microscopy (SEM), UV-visible spectroscopy, encapsulation efficiency, in vitro drug release, and release kinetics. Finally, stability of liposomes was performed.
Results and discussion: RA liposome showed variable Nano metric size distribution from 136 nm to 44 nm and demonstrates spherical morphology. The highest loading efficiency of liposomal RA was 52% and illustrated 73% release its payload after 9 hours. Liposomes show good stability at 5, and 25°C following 6 months.
Conclusion: The results illustrated that RA liposome would be a great tool to enhance the penetration of hydrophobic agent through the cornea and improve therapeutic outcomes. In vivo experiments should be confirmed our current in vitro results.
Keywords: Rosmarinic acid; Sodium deoxycholate; Liposome; Cataract
Introduction
The opacification of the lens, called cataracts, is responsible for degrading visual acuity as a consequence of scattering the light as it passes through the lens. The ocular lens plays a pivotal part in focusing the light on to the retina, and its clarity is essential for visual acuity. In 2020, the prevalence of cataracts had been 15.2 million cases among over 50 years globally. It has been estimated by the year 2050; approximately 50 million people in the United States will suffer from cataracts. According to statistics, cataracts will increase with passing years. Cataracts are considered the underlying cause of blindness globally. When the average age of the earth's population is on the rise, cataract-induced blindness and visual dysfunction will increase dramatically [1]. Currently, the only viable treatment for cataracts is surgery, including removing the opaque lens and replacing it with an artificial one which has a huge impact on improving the patient's quality of life. Undoubtedly, cataracts have far-reaching repercussions for countries in terms of social and economic burdens, for example, the increasing rate of automobile accidents due to reduced visual acuity [2]. Nonetheless, surgery is not a choice in developing countries due to the lack of facilities, ophthalmologists, and funds [3]. It should be noted that posterior capsular opacification is a common complication of cataracts, and sometimes, a second intervention is necessary [4].
A study conducted by Chemerovski-Glikman, et al. suggested that Rosmarinic acid can restore the transparency of the lens due to its amyloid destabilization effect and remolding lentic protein aggregate. They have developed an ex vivo assay for screening anti-cataract medications. They found that Rosmarinic acid completely restores the clarity of the human cataractous lens in ex vivo and delays cataract formation in selenite-induced cataracts in the newborn rat model [5]. Previous studies have reported that Rosmarinic acid also able to bind to oligomers of Aβ and alpha-synuclein by interfering with protein aggregates in neurodegenerative disease [6]. Tsai and colleagues carried out a study to assess the protective effect of Rosmarinic acid on selenite-induced cataracts in Sprague-Dawley rat pups. They administered RA intraperitoneally to different groups of animals. They measured antioxidant parameters (NQO1, SOD, HO-1, and Nrf2), the GSH levels, and antioxidant enzymes activities (GSH-Rd, catalase, and GSH-Px) and observed that they were downregulated. Moreover, they illustrated that injection of RA could reduce the severity of the opaque lens and decrease the oxidative damage in the lens [7]. Rosmarinic Acid (RA) is composed of caffeic acid and 3,4-dihydroxyphenylacetic acid esterification is derived from Lamiaceae family. It is isolated from Rosmary (Rosmarinus officinalis) and other plants. It is widely used as radical scavenger that acts as antioxidant to prevent formation of lipid peroxidase [8]. The antioxidant activity of RA depends on polyphenolic groups that are free radical scavengers. Kuo and colleagues investigate the antioxidant and anti-apoptotic activity of RA by decreasing the level of ROS and Malondial-Dehydrate (MDA) as well. They illustrated that the potential glioprotective effect of RA on H2O2 induced oxidative stress in astrocytes [9]. The role of oxidant activity in the onset of cataract has been published in the literature. Furthermore, antioxidants serve potential treatment for cataract treatment [10].
Liposomal formulation was used significantly for the ophthalmic drug delivery. They mainly composed of phosphatidylcholine and other component such as sodium deoxycholate to make them unique for their usage. Liposomes can reduce the total amount of drug required. They are considered biodegradable and more compatible to the body [11]. Sodium deoxycholate has been widely used as a penetration enhancer for many delivery routes and protects drug from degradation [12] Dai, et al. show that liposomes containing Sodium deoxycholate improve the transport of tacrolimus through the cornea by 3-4 fold [13]. Shen and Tu prepared liposomes containing sodium deoxycholate by reverse phase evaporation model. They illustrated that delivery of ganciclovir to the transcorneal was 3-9 fold as compared to free ganciclovir [14].
On account of above consideration, first, we prepared RA liposome incorporating sodium deoxycholate by ethanol injection method which possesses safety, simplicity, and repeatability. Then, formulations were characterized in terms of particle size, zeta potential, PDI, encapsulation efficiency. In vitro release study was evaluated by dialysis bag and UV-visible spectroscopy.
Materials and Methods
Rosmarinic Acid (RA), Soy Phosphatidyl Choline (SPC), and Sodium deoxy Cholate (SDC) were purchased from Sigma Aldrich (St. Louis, Missouri, USA). All other chemicals used were of analytical grade.
Preparation of formulations
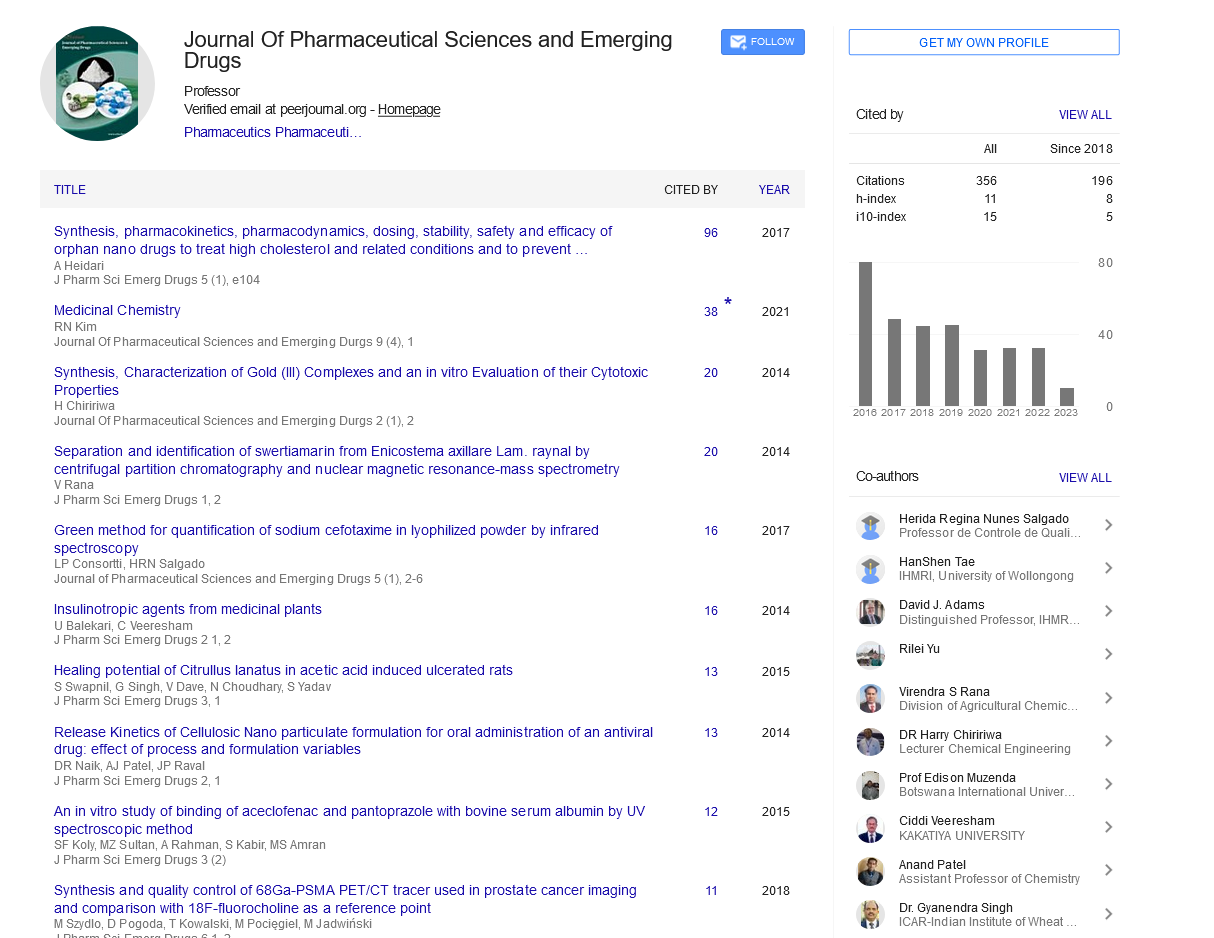
The composition of different liposome formulations are displayed in table 1. RA liposomes were prepared by ethanol-injection method. Briefly, 100 μg/ml of soy phosphatidylcholine, 2.5 μg/ml of Rosmarinic acid and sodium deoxycholate were dissolved in 1 ml absolute ethanol at 80°C, and then ethanolic solutions were rapidly injected into 20 ml of distilled water under heating to 80°C, resulting the formation of multivesicular vesicle dispersion. The solutions were stirred for 20 minutes at 80°C to evaporate ethanol from the solutions [15]. Afterwards, 20 ml of the prepared liposome were sonicated by a probe Sonicator (Heidolph, Germany) for obtaining optimized time and amplitude using a 19 mm needle probe titanium tip as shown in figure 1. Centrifugation for 15 min at the speed of 15,000 rpm (MPW, MED INSTRUMENTS-150R, and Germany) was applied for liposome purification. Finally, liposomes were filtered with a 0.22 μm membrane filter.
| Amplitude (%) | Sonication time (min) | Vesicle size (nm) | PDI | Zeta Potential |
|---|---|---|---|---|
| 0 | 0 | 768.2 ± 12.4 | 0.245 ± 0.032 | -47.1 ± 1.4 |
| 15 | 5 | 212.1 ± 0.4 | 0.323 ± 0.30 | -45.2 ± 0.5 |
| 10 | 1934 ± 1.7 | 0.214 ± 0.019 | -45.3 ± 0.4 | |
| 15 | 186.1 ± 1.5 | 0.288 ± 0.008 | -52.1 ± 0.7 | |
| 20 | 138.3 ± 0.8 | 0.331 ± 0.002 | -48.2 ± 0.6 | |
| 25 | 5 | 108 ± 3 | 0.129 ± 0.012 | -36.07 ± 0.45 |
| 10 | 100.7 ± 2.4 | 0.142 ± 0.020 | -41.5 ± 1.0 | |
| 15 | 79.1 ± 1.7 | 0.230 ± 0.042 | -39.2 ± 1.9 | |
| 20 | 70.9 ± 1.6 | 0.215 ± 0.019 | -42.4 ± 0.1 | |
| 10 | 100.7 ± 2.4 | 0.142 ± 0.020 | -41.5 ± 1.0 | |
| 15 | 79.1 ± 1.7 | 0.230 ± 0.042 | -39.2 ± 1.9 | |
| 20 | 70.9 ± 1.6 | 0.215 ± 0.019 | -42.4 ± 0.1 |
Table 1: Vesicle size (nm), PDI, and Zeta-Potential (mv) of Nano liposomes prepared by sonication treatment Particles size, Zeta potential, and PDI
Sonication method
Sonication procedure was conducted in order to obtain acceptable size distribution, since particles smaller than 200 nm are preferred for ocular applications. Suspension containing 2.5:1 (w/v) SPC: SDC was subjected to 5, 10, 15, 20 min of sonication treatment with different amplitudes (15, 25% of full power). Formulations were kept in an ice bath to prevent from heating during sonication [16].
Characterization of formulations
Particle size, Zeta potential, and Poly Dispersity Index (PDI).
The liposomal dispersion was homogenized by vortexing and diluted 1:10 (v/v) with freshly filtrated (0.2 μm) distilled water before size measurement. Each sample was analyzed in triplicate. The Malvern Zetasizer Nano Series gave information about the average size based on intensity, volume, and the number of liposomes, Poly Dispersity Index (PDI), and zeta potential [17].
Encapsulation efficiency
The amount of Rosmarinic acid loaded into liposome formulation was measured utilizing a UV-visible spectrophotometer. First, for plotting the calibration curve, different concentration of Rosmarinic acid ethanolic solutions (1, 2, 5, 8, 10, 12, 14 μg/ml) were prepared [18]. To determine the encapsulation efficiency of the liposomal formulations, prepared lipid vesicles were separated from the (unseparated) drug by centrifugation at 14,000 rpm for 15 min; in these conditions, the liposomes remained suspended, and the free drug precipitated [19]. Small aliquots of liposomes (50 μl) were diluted in 950 μl methanol, were subjected to sonication until liposomes disruption, and quantified spectrophotometrically at 327 nm, which corresponded to the maximum absorbance of RA. Hence, encapsulation efficiency was measured using following equation:

Morphological characterization of liposomes using Scanning Electron Microscopy (SEM)
For the morphological observation, 1 ml of the sample was placed in the sample holder and dried in a desiccator in order to dry. Then the sample was coated with a 5 nm gold layer using a rotary pumped coater, and the morphology was observed by a mira 3 te scan [20].
Release rate of rosmarinic acid from liposome
The release test was evaluated by the release of Rosmarinic acid from encapsulated liposome. In brief, 2 ml of liposomal solution was loaded into a dialysis bag (MW, 12000), then two ends were clipped and placed in 400 ml of fresh PBS medium (pH 7.4) at 60 rpm under sink conditions. At specific periods, 2 ml of the samples were withdrawn and 2 ml of fresh PBS buffer was immediately replaced. The released RA amounts were analyzed by UV/vis spectrophotometer at 327 nm. Drug concentration was calculated using a standard calibration curve (R2=0.9987) and expressed as a cumulative percent of drug release. The release study was performed in triplicate [21].
Kinetic release study: The release mechanism of Rosmarinic acid from the liposomes was interpreted by four classic models including zero-order (Eq 1), first-order (Eq 2), Higuchi (Eq 3), Korsmeyer- Peppas (Eq 4), and Hixon-Crowell (Eq 5) models [22]:
Zero order model-Mt/M ∞=Kt………(eq 1)
First-order model-Log Mt/M ∞=Kt………(eq 2)
Higuchi model-Mt/M ∞=Kt1/2………(eq 3)
Korsmeyer-Peppas-Mt/M ∞=Ktn………(eq 4)
Hixon-Crowell model-(Mt/M ∞) 1/3=Kt………(eq 5)
Where Mt is the cumulative amount of released drug at time t, Mt / M∞ is the fraction of drug released, and k is the constants for each models.
Stability: Storage stability was investigated under two different conditions (4°C and 25°C ± 60% relative humidity). Different parameters such as particle size, zeta potential, and poly dispersity index in residual RA were measured at regular intervals. The initial amount of RA in the formulations was 100% [23].
Statistical analysis
Statistical analysis of the data was conducted using Microsoft® Excel 2016. Data were reported as mean ± Standard Deviation (SD).
Results
Sonication treatment
Firstly, for achieving suitable particle size probe sonication was applied to formulations. Results illustrated that sonication procedures were capable to decrease particle size. The data as shown in table 1. Particle size was reduced by increasing both sonication time and amplitude. The particle size of Nano liposomes reached 108, 100.7, 79.1, and 70.9 nm after a 5, 10, 15, and 20 min-treatment and 25% amplitude treatment respectively. It is suggested that high-power sonication results in mechanical vibration and generate powerful waves, inducing smaller particle. However, increasing time may result in the degradation of particles, so 5 min sonication treatment and 25% amplitude was selected for further studies.
The mean particle size showed minor variation with respect to the liposome component. Among formulations, F9, showed the lowest particle size which correlated to the lack of SDC in the formulation? The highest particle size was obtained in the case of F2.
All formulations except F2 were decreased with decreasing content of SDC. The PDI values obtained in this work ranged from 0.247 to 0.089. The highest PDI value was 0.247, corresponding to the F2 formulation, whereas the smallest PDI value was obtained from the F4 formulation. The PDI values of F5 and F6 were more or less the same.
The zeta potential varied between F1 and F9 formulations. The zeta potential of the study was constantly negative except for f9 formulation. For F1 and F2 formulations, the zeta potential is bigger than -30 mv. Encapsulation efficiencies of RA in different formulations are presented in Table 1. As illustrated, efficiencies varied between 51.81 ± 0.59% and 11.87 ± 0.56%. The highest encapsulation efficiencies for RA related to F2 and there was statistically significant difference between F1 and F2 (p<0.05). As demonstrated, the encapsulation efficiencies of liposomes decreased with decreasing content of sodium deoxycholate from 35 to 0 μg/ml. whereas, with increasing amount of SDC from 35 to 40 μg/ml leads to decreasing encapsulation efficiencies. The lowest encapsulation efficiencies corresponded to F9 (Table 2).
| Formulations code | RA |
SPC |
SDC |
Mean particle size (nm) | PDI | Zeta Potential (mv) | Encapsulation Efficiency (%) |
|---|---|---|---|---|---|---|---|
(µg/ml) |
(µg/ml) |
||||||
| F1 | 25 | 100 | 40 | 108 ± 3 | 0.129 ± 0.012 | -36.07 ± 0.45 | 32.5 ± 1.01 |
| F2 | 25 | 100 | 35 | 136 ± 3 | 0.247 ± 0.022 | -32.83 ± 0.71 | 51.81 ± 0.59 |
| F3 | 25 | 100 | 30 | 128 ± 1 | 0.231 ± 0.01 | -28.8 ± 0.36 | 42.27 ± 0.15 |
| F4 | 25 | 100 | 20 | 97 ± 1 | 0.089 ± 0.009 | -24.63 ± 0.61 | 38.86 ± 0.29 |
| F5 | 25 | 100 | 16 | 76 ± 2 | 0.152 ± 0.022 | -22.43 ± 1.2 | 31.02 ± 0.66 |
| F6 | 25 | 100 | 12 | 63 ± 2 | 0.159 ± 0.024 | -21.17 ± 0.59 | 21.11 ± 0.27 |
| F7 | 25 | 100 | 8 | 56 ± 1 | 0.123 ± 0.013 | -17.6 ± 0.77 | 17.34 ± 0.59 |
| F8 | 25 | 100 | 4 | 54 ± 1 | 0.11 ± 0.03 | -11.2 ± 1.1 | 12.11 ± 0.34 |
| F9 | 25 | 100 | 0 | 44 ± 1 | 0.21 ± 0.008 | 1.2 ± 0.63 | 11.87 ± 0.56 |
Table 2: The composition of liposomal formulations and obtained results for size, PDI, zeta potential, and encapsulation efficiency
SEM image
The shape of the optimized RA-loaded Nano liposomes was evaluated using SEM. It should be noted that the SEM images were taken by F2 formulations, which showed optimal characteristics based on particle size, zeta potential, encapsulation efficiencies (Figure 2).
In vitro release of RA liposome
The release study is presented in figure 3. The data showed that cumulative release percentage of free Rosmarinic acid and Rosmarinic acid liposome remarkably differed. Approximately all amount of free Rosmarinic acid was released after 6 h, while the Rosmarinic acid liposome displayed a sustain release, which nearly 73% of contents was release at the same time.
Kinetic release study
The in vitro drug release profile was applied in different mathematical models and was interpreted in the form of graphical presentation and evaluated by the correlation coefficient (R2) represented in (Table 3). Korsmeyer-Peppas best fitted model.
| Model | Equation | R2 |
|---|---|---|
| Zero-order | y=6.2198x+29.06 | R2=0.687 |
| First-order | y=-0.0556x+1.8429 | R2=0.8396 |
| Higuchi | y=0.9607x-10.759 | R2=0.8575 |
| Krosmeyer-Peppas | y=0.0243x+0.2438 | R2=0.8902 |
| Hixson-Crowell | y=0.5025x+1.1173 | R2=0.5985 |
Table 3: kinetic analysis of liposome RA
Stability
Particle size was measured following 6 months of storage at 4, and 25° C to study stability. No significant changes in the particle size of lyophilized liposomes were seen after reconstitution. Initially, the average particle size was 136 nm. Following 6 months the average particle size was 143 and 150 nm at 4 and 25°C, respectively (Table 4).
| Conditions | Time (Months) | Average Size (nm) | Polydispersity Index | Zeta Potential (mV) |
|---|---|---|---|---|
| 4°C ± 0.5°C/60 % ± 5 % RH1 | Initial | 136 ± 3 | 0.247 ± 0.022 | -32.83 ± 0.71 |
| 1 | 141.6 ± 3.2 | 0.234 ± 0.001 | -33.41±1.65 | |
| 3 | 139.2 ± 6.7 | 0.331 ± 0.089 | -34.7±2.41 | |
| 6 | 143 ± 2.6 | 0.341 ± 0.002 | -36.42±1.32 | |
| 25°C ± 2°C/60 % ± 5% RH1 Conditions |
Initial | 136.81 ± 2.54 | 0.276 ± 0.056 | -33.12±0.71 |
| 1 | 140.5±1.2 | 0.221 ± 0.005 | -32.54±1.21 | |
| 3 | 143.2 ± 1.3 | 0.229 ± 0.003 | -33.79±0.31 | |
| 6 | 150 ± 1.6 | 0.267 ± 0.002 | -31.52±1.7 | |
| Time (Months) | Average Size (nm) | Polydispersity Index | Zeta Potential (mV) |
Table 4: Storage stability of RA liposome under different conditions (4°C and 25°C)
Note: Relative Humidity (RH1)
Discussion
Nano liposomes have several advantages including, increase drug concentration in ocular tissues, increasing corneal permeation, and controlling drug release [24]. The main aim of the current study was to investigation of novel RA Nano liposomes prepared by ethanol injection method which possess suitable physicochemical characteristics. Because of low water solubility of RA and poor bioavailability, encapsulation of RA into liposomes can enhance bioavailability and increasing stability of phenolic compounds. Liposomes were prepared by ethanol injection method because of safety, rapidity, and reproducibility. Different liposomal formulations (F1-F9) were prepared and characterized such as particle size, zeta potential, PDI, and encapsulation efficiencies. Furthermore, surface morphology was characterized by SEM. It is a well-established fact that particles smaller than 200 nm, showed higher penetration to the eye (about 50-fold) compared than micron-sized particles [25]. Furthermore, particle size affect encapsulation efficiencies and drug release [26]. In this study all formulations showed smaller than 200 nm particle size. However, Formulation F3 was considered to be optimum, which is prepared by a 35 μ g/ml SDC. It showed an average particle size of 136 ± 3 nm and higher encapsulation efficiencies (51.81 ± 0.59). The most interesting result in this study was found when the concentration of SDC increased from 35 to 40 μ g/ ml. In this state, the particle size decreased from 136 ± 3 to 108 ± 3 nm. This phenomenon is in agreement with previous reporting that increasing the content of SDC resulted in smaller vesicles [27]. This could be explained based on the fact that micelles start to form instead of vesicles with an increase in SDC concentrations. The size of the Nano liposomes prepared by our method was smaller than similar work that who have worked on the liposomal formulation of RA using the lipid film hydration method 18.
Poly Dispersity Index (PDI) is utilized to evaluate size distribution of formulations, which affects directly to stability. An acceptable range of PDI is 0.3 or less, meaning that 66.7% of all nanoparticles have same distributions [28]. In this study, the amount of SDC incorporation had no obvious impact on the mean PDI of the vesicles. However, all PDI formulations were in the acceptable range.
An important parameter used in this study was zeta potential which measures the overall charge of vesicles in a medium and showing the stability of Nano liposomes. Generally, formulations less than -30 mV and greater than 30 mV is the stable, which demonstrate a good stability and prevent aggregation. In this work, all formulation showed negative zeta potential except F9 formulation. The relatively positive zeta potential of F9 was not amazing in that liposome due to lack of SDC. The reason for negative charge is related to the presence of SDC in the formulation and also with increasing amount of SDC, the negative charge was increased. It is uncertain that whether the carboxylic acid of RA is contributed to zeta potential or not, so it can be assumed that the net charge of vesicle surface is depend on SDC because of neutral charge of SPC. It should be noted that, increasing electrostatic repulsion between the particles led to decreased particles aggregation, which displays a longer shelf-life and more stability.
The encapsulation efficiencies of RA in liposomes prepared by ethanol injection was relatively varied and ranged from 12 to 52%. In general, encapsulation efficiency was observed to be linked to the particle size. In this study, the behavior of the encapsulation efficiencies was nearly similar to particle size and amount of SDC. For instance, when particle size decreased as a result of declining amount of SDC, encapsulation efficiencies decreased too. This could be explained by the fact that, the gradual rise in entrapment efficiency might also result from enhanced viscosity of the micellar system, supporting the stability of the internal aqueous phase and limiting the interaction with outer aqueous media.
Similar to particle size, the result of this study confirmed that increase in surfactant concentration directly correlate to encapsulation efficiency, may be due to the increased solubility of the drug. But, higher SDC concentration (above a 35 μ g/ml) reduced the encapsulation efficiencies. This phenomenon could be related to drug leakage which affected by micelles formation above certain concentration and shown in the particle size. Similarly, Arafat et.al. Developed a Nano sized liposomes containing Sodium Deoxy- Cholate. They announced that drug encapsulation is correlated to particle size [27].
The SEM micrograph gives important information regarding spherical shape of the Nano liposomes and also revealed the presence of nanoparticles with particle sizes smaller than 200 nm.
Taking into account that liposomes prepared the 35 μg/ml are at an optimum concentration. Therefore, this formulation was used in the next step to evaluate the release study and also for stability evaluations.
In order to develop an efficient delivery system with desired release characteristics, it is crucial to calculate the rate of drug release. Because, in vitro release conditions (37°C and pH often predict the in vivo performance of formulations. The results indicate that slow release of liposomes RA was mainly owing to its hydrophobic nature of RA which loaded in the bilayer of liposome. The rapid release of free RA may be contributed to lack of bilayer structure which cause delay in the release of RA.
The release kinetics seems to that Korsmeyer-Peppas best fitted experiment in the basis of correlation coefficient (R2=0.8902). It can be concluding that RA released from vesicles according to diffusion and erosion controlled release. Therefore, at the initial time, liposomes might expand to some degree and allow the RA diffuse through the interface to the medium.
Stability studies for six months were performed to evaluate the ability of the prepared formulations to protect its physicochemical properties. The optimized formulation (F2) was stored at 4, and 25°C. High physical stability of the formulations was seen during these periods. It is important to mention that liposomes remained unchanged, neither flocculation nor sedimentation. The result demonstrates that liposome RA were stable at 4, and 25°C for 3 months. However, biological assessment for the efficacy of current formulation should be evaluated.
Conclusion
Rosmarinic acid as a potential anti-cataract agent was loaded into liposomes, and its physicochemical characteristics were evaluated. The morphology of the obtaining formulation was spherical. The encapsulation efficiency of RA was ~52%, and its release behavior displayed a delayed release compared to free RA (73% compared to 100% in 9 hours). Finally, physical stability revealed that formulation was stable after 6 months. Consequently, this delivery system can be effective for delivery of RA to the anterior segment of the eye.
Acknowledgment
This study was technically supported by Tehran University of Medical Sciences.
Conflict of Interest
There is no conflict of interest.
References
- Steinmetz JD, Bourne RR, Briant PS, Flaxman SR, Taylor HR, et al (2020) Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 9:e144-e160.
- Lamoureux EL, Fenwick E, Pesudovs K, Tan D (2011) The impact of cataract surgery on quality of life. Curr Opin Ophthalmol 22:19-27.
- Brian G, Taylor H (2001) Cataract blindness: Challenges for the 21st century. Bull World Health Organ 79:249-256.
- Ashwin PT, Shah S, Wolffsohn JS (2009) Advances in cataract surgery. Clin Exp Optom 92:333-342.
- Chemerovski-Glikman M, Mimouni M, Dagan Y, Haj E, Vainer I, et al. (2018) Rosmarinic acid restores complete transparency of sonicated human cataract ex vivo and delays cataract formation in vivo. Sci Rep 8:9341.
- Ono K, Li L, Takamura Y, Yoshiike Y, Zhu L, et al. (2012) Phenolic compounds prevent amyloid β-protein oligomerization and synaptic dysfunction by site-specific binding. J Biol Chem 287:14631-14643.
- Tsai CF, Wu JY, Hsu YW (2019) Protective effects of rosmarinic acid against selenite-induced cataract and oxidative damage in rats. Int J Med Sci 16:729.
- Nadeem M, Imran M, Aslam Gondal T, Imran A, Shahbaz M, et al (2019) Therapeutic potential of rosmarinic acid: A comprehensive review. Appl Sci 9:3139.
- Luño V, Gil L, Olaciregui M, González N, Jerez RA, et al (2014) Rosmarinic acid improves function and in vitro fertilising ability of boar sperm after cryopreservation. Cryobiology 69:157-162.
- Xu J, Fu Q, Chen X, Yao K (2020) Advances in pharmacotherapy of cataracts. Ann Transl Med 8:1552
- Meisner D, Mezei M (1995) Liposome ocular delivery systems. Adv Drug Deliv Rev 16:75-93.
- Dai Y, Zhou R, Liu L, Lu Y, Qi J, (2013) Liposomes containing bile salts as novel ocular delivery systems for tacrolimus (FK506): In vitro characterization and improved corneal permeation. Int J Nanomedicine 8:1921-1933.
- Shen Y, Tu J (2007) Preparation and ocular pharmacokinetics of ganciclovir liposomes. AAPS J 9:E371-E377
- van der Valk FM, van Wijk DF, Lobatto ME, Verberne HJ, Storm G, et al (2015) Prednisolone-containing liposomes accumulate in human atherosclerotic macrophages upon intravenous administration. Nanomedicine 11:1039-1046.
- He Y, Luo L, Liang S, Long M, Xu H (2019) Influence of probe-sonication process on drug entrapment efficiency of liposomes loaded with a hydrophobic drug. Int J Polym Mater 68:193-197.
- Marsalek R (2014) Particle size and zeta potential of ZnO. APCBEE Procedia 9:13-17.
- Yücel Ç, Şeker Karatoprak G, Değim İT (2019) Anti-aging formulation of rosmarinic acid-loaded ethosomes and liposomes. J Microencapsul 36:180-191.
- Haeri A, Sadeghian S, Rabbani S, Anvari MS, Lavasanifar A, el at (2013) Sirolimus-loaded stealth colloidal systems attenuate neointimal hyperplasia after balloon injury: A comparison of phospholipid micelles and liposomes. Int J Pharm 455:320-330.
- Buhr E, Senftleben N, Klein T, Bergmann D, Gnieser D, et al (2009) Characterization of nanoparticles by scanning electron microscopy in transmission mode. Meas Sci Technol 20:084025.
- Jeetah R, Bhaw-Luximon A, Jhurry D (2014) Nanopharmaceutics: Phytochemical-based controlled or sustained drug-delivery systems for cancer treatment. J Biomed Nanotechnol 10:1810-1840.
- Dash S, Murthy PN, Nath L, Chowdhury P (2010) Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm 67:217-223.
- Du Plessis J, Ramachandran C, Weiner N, Müller DG (1996) The influence of lipid composition and lamellarity of liposomes on the physical stability of liposomes upon storage. Int J Pharm 127:273-278.
- Phua JL, Hou A, Lui YS, Bose T, Chandy GK, et al (2018) Topical delivery of senicapoc nanoliposomal formulation for ocular surface treatments. Int J Mol Sci 19:2977.
- Baba K, Tanaka Y, Kubota A, Kasai H, Yokokura S, et al (2011) A method for enhancing the ocular penetration of eye drops using nanoparticles of hydrolyzable dye. J Control Release 153:278-287.
- Honary S, Ebrahimi P, Hadianamrei R (2014) Optimization of particle size and encapsulation efficiency of vancomycin nanoparticles by response surface methodology. Pharm Dev Technol 19:987-998.
- Arafat M, Kirchhoefer C, Mikov MM, Sarfraz MK, Löbenberg R (2017) Nanosized liposomes containing bile salt: A vesicular nanocarrier for enhancing oral bioavailability of BCS class III drug. J Pharm Pharm Sci 20:305-318
- Maritim S, Boulas P, Lin Y (2021) Comprehensive analysis of liposome formulation parameters and their influence on encapsulation, stability and drug release in glibenclamide liposomes. Int J Pharm 592:120051.
- Smith MC, Crist RM, Clogston JD, McNeil SE (2017) Zeta potential: A case study of cationic, anionic, and neutral liposomes. Anal Bioanal Chem 409:5779-57787.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 


 ) RA solution, (
) RA solution, ( ) RA liposome.
) RA liposome.