Short Communication, J Mol Biol Methods Vol: 3 Issue: 1
Potential False Negatives in the Molecular Diagnostics of COVID-19 Infection: Experience of an Italian Laboratory during the COVID-19 Epidemic
Alessandro Pancrazzi*, Roberta Perticucci, Stefania Vecchietti, Gianluca Magrini, Guendalina Vaggelli, Pasqualino Magliocca, Angelo Galano, Manuela Mafucci, Irene Alessandra Galanti and Agostino Ognibene
U.O.C. Analysis Laboratory, Molecular and Clinical Pathology Sector, San Donato Hospital, COVID Hospital, Arezzo, Italy
*Corresponding Author : Alessandro Pancrazzi
Biologist Manager, U.O.C. Analysis Laboratory, Molecular and Clinical Pathology Sector, San Donato Hospital, COVID Hospital, Arezzo, Italy
Tel: +39 0575 255 271
E-mail: alessandro.pancrazzi@uslsudest.toscana.it
Received: March 23, 2020 Accepted: April 7, 2020 Published: April 14, 2020
Citation: Pancrazzi A, Perticucci R, Vecchietti S, Magrini G, Vaggelli G, et al. (2020) Potential False Negatives in the Molecular Diagnostics of COVID-19 Infection: Experience of an Italian Laboratory during the COVID-19 Epidemic. J Mol Biol Methods 3:1. doi: 10.37532/jmbm.2020.3(1).106
Abstract
The current situation in the molecular diagnostics field applied to the SARS-CoV-2 (Severe Acute Respiratory Syndrome Corona virus 2) virus detection has forced various laboratories to quickly offer a solution for the identification of the infected people in this pandemic scenario recently declared by the World Health Organization.
In the epidemiological emergency, the rapid commercialization of CE-IVD kits pushed numerous hospitals to adopt these methods without complete internal validations that would allow evaluating the actual analytical methods limits. Moreover, the same WHO, given the global escalation of the epidemic, has listed the methods used so far for the viral RNA detection also in lack of validation data reports.
This communication reports the starting experience in using Seegene molecular kit for COVID-19 (CO-rona VI-rus Disease) at the San Donato Hospital in Arezzo, a territorial support hospital structure for the molecular screening COVID-19.
The investigation strategy is based on molecular analysis starting from RNA extract obtained from oropharyngeal / nasal / sputum swabs. The problem linked to this type of samples consists mainly in obtaining an intact analysis matrix not affected by degradation due to incorrect conservation or by the presence of RNase.
Keywords: COVID-19; Molecular diagnostics
About the Study
The current situation in the molecular diagnostics field applied to the SARS-CoV-2 (Severe Acute Respiratory Syndrome Corona virus 2) virus detection has forced various laboratories to quickly offer a solution for the identification of the infected people in this pandemic scenario recently declared by the World Health Organization [1].
In the epidemiological emergency, the rapid commercialization of CE-IVD kits pushed numerous hospitals to adopt these methods without complete internal validations that would allow evaluating the actual analytical methods limits. Moreover, the same WHO, given the global escalation of the epidemic, has listed the methods used so far for the viral RNA detection also in lack of validation data reports [2]. On the other hand, the manufacturing companies themselves faced a sudden high request to comply need for epidemiological investigation by the health authorities [3].
The commercial kits, currently available on the market, are produced by Seegene Inc. (South Korea, locally distributed by Arrow Diagnostics Diagnosticss.r.l., Italy) and GENDX (GeneFinder ™ OSANG healthcare).
In Italy, many analysis laboratories, given the widespread use of NIMBUS (Hamilton Italy Srl) preparation platforms, already previously adopted for molecular virology and for high throughput necessities, have chosen Seegene technology.
This communication reports the starting experience in using Seegene molecular kit for COVID-19 (CO-rona VI-rus D-isease) at the San Donato Hospital in Arezzo, a territorial support hospital structure for the molecular screening COVID-19.
The investigation strategy is based on molecular analysis starting from RNA extract obtained from oropharyngeal / nasal / sputum swabs. The problem linked to this type of samples consists mainly in obtaining an intact analysis matrix not affected by degradation due to incorrect conservation or by the presence of RNase [4-6].
The PCR design of the Seegene assay, according to the publications reported by WHO, is based on multitarget detection of the regions E, RdRp and N [7]. The analytical positivity determination system has following approach: the samples showing valid amplification for all the three targets are considered positive. This kit also contains an exogenous reaction control (RP-V IC, henceforth called IC), this material is added at first step, in pre-extraction phase, in the amount of 10 ng in each individual sample to be analyzed. This addition allows verifying correct conditions for the reverse transcription and subsequent PCR.
A critical point of this system is the lack of specific oligonucleotides for housekeeping sequences, necessary to verify the integrity of the extracted material. According to auto-analysis setting (See gene Viewer for Real time Instruments V3, version 3.18.003 trial corona, Seegene Inc.), negative result consists in absence of target signal and valid amplification of IC within fortieth cycle. This approach does not allow verifying if the initial analysis matrix had a successful extraction process of RNA.
For this critical condition, we attempted to interpret Ct value of IC to obtain information about analysis reliability.
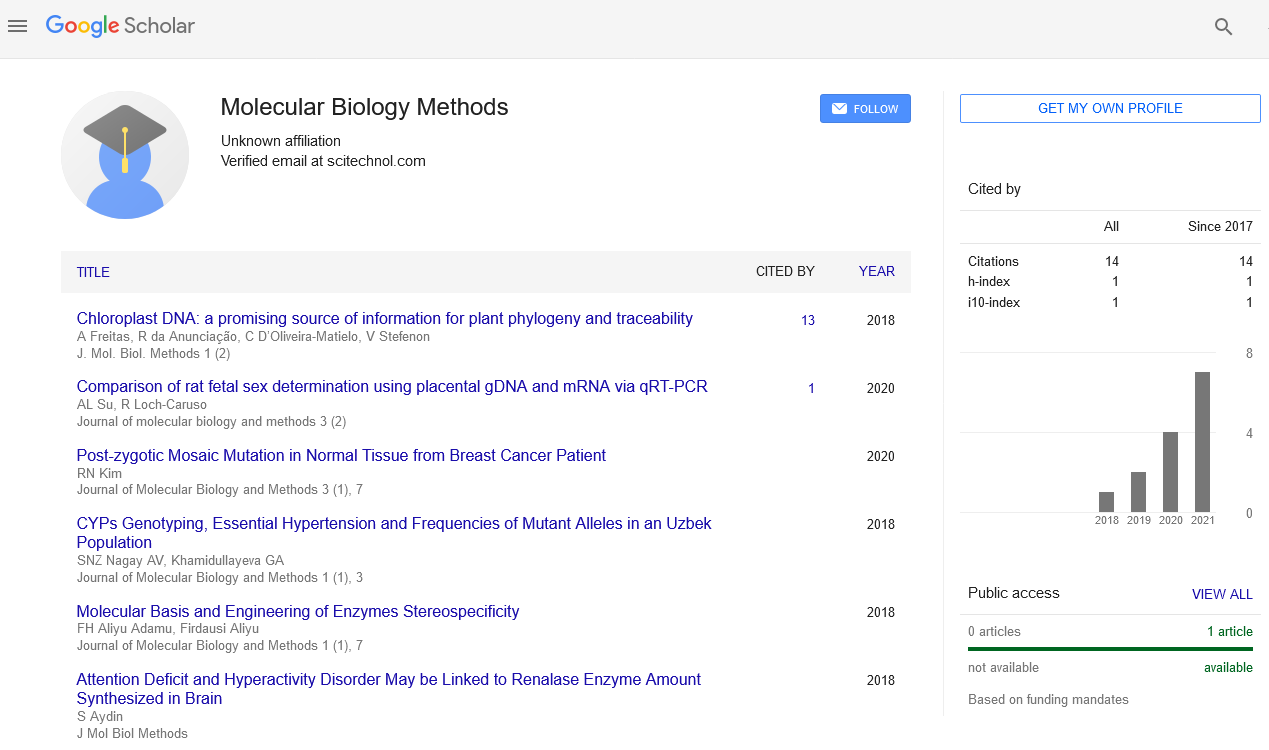
We examined 424 swab samples, sent from clinical critical area of the hospital, among which the autoanalysis setting system identified 333 negatives, 76 positives, 11 inconclusive (partial amplification of the panel of the three targets) and 4 invalid (total absence of amplification for viral and IC targets). The kit contains probes concentration created for unbalanced competitive reaction to the benefit of the viral target’s amplification (E, RdRp and N), therefore, in case of the positive sample, viral sequence amplification has more efficiency than referred to IC.
In case of negative samples, the IC amplification performance should be optimal and above all relatively homogeneous, considering that the amount of IC RNA dispensed in each sample is the same and in these cases there is no viral competition target cDNA.
In most of the samples defined negative by the self-analysis we noted an oscillation of the PCR efficiency referred to IC about two orders of magnitude around the average value (± 6.6 ΔCt). Regard a relatively small percentage (5/333, 1.5%) of cases, defined like negatives, a significant deviation from the total negatives average is observed (bigger than two logarithmic values, ΔCt> 6.6). Part of these "outlier" samples, characterized by a significantly lower theoretical efficiency compared to the other "Selected" negatives (p value <0.0001), have a value of ΔCt ICs (= Ct IC Sample Negative -Ct average Negative Samples) greater than 12 cycles. Based on these observations, OUTLIER can be defined a sample without viral sequence amplification result and ΔCt ICs >6.6 (Table 1).
| Total Negative | Selected Negatives | Outlier Negatives | |
|---|---|---|---|
| Ct Average | 25.74 | 25.62 | 36.31 |
| ds | 1.83 | 1.26 | 2.94 |
| Min | 23.37 | 23.37 | 32.44 |
| Max | 38.97 | 31.03 | 39.97 |
| Ct Median Value | 25.34 | 25.33 | 37.61 |
Table 1: Ct variability values of IC in negative samples.
Possible causes generating outlier negatives could be due to:
- Incorrect dispensing volume of the IC: the lower initial quantity of control would affect the yield.
or
- Technical problem related to the automated extraction phases: this case is normally checked and promptly reported by the platform, never happened in these analytical sessions;
or
- Presence of PCR inhibitors in the collection, including the possible presence of protease RNAs that could partially degrade both the sample and the control.
The automatic analysis settings, programmed by the manufacturer, provide for considering a valid run if the Ct value of the exogenous control (IC) is lesser of 40 cycles of amplification, this is the pre-set limit also for the outputs of the viral specific targets E, RdRp and N [8].
However, if a significant amount of RNAse is present on the collected sample, there is concrete possibility that the sample is unsuitable for analysis and the "late" exit of the IC control (outlier) could be a sign of this condition. In particular, IC amplification results close to the 40th cycle and the amplification absence of the viral region targets should persuade to confirm test outcome by repeat collection or using another analysis method. The recommendation to repeat this result type should be part of best laboratory practice aimed at decreasing false negatives risk.
One of the systems that could make it possible to select unsuitable samples due to the occurrence of RNA degradation could be to perform a external to the automated system PCR using oligonucleotides and specific probes for housekeeping genes. Unfortunately, the need to quickly use an automated system (mass screening necessity as currently happens in Italy) and the impossibility to recover the cDNA phase from the automated preparation platform, impede realization of this solution.
Given the relatively large number of samples analysed, the low incidence found here of the outlier negative samples (5/333 neg samples, 1.5% ; 1.2% in relation to the analysed total ), it is proposed not to provide a response result for these and to recommend a new collecting of the swab.
The interpretation that is proposed here consist to reject negative result for samples that have ΔCt IC higher than 6.6 (“outlier samples”) and recommend a new collection.
The OUTLIER cohort identification is relatively simple considering statistically significant diversity compared to the other negatives so far collected in this records (Figure 1).
Naturally, this proposed response is already practiced for the 2 invalids (1%), these evidently can be considered the consequence of the same hypothetical cause that generated the outliers.
This solution seems acceptable and appropriate for the following reasons:
The risk, even if remote, of generating a false negative laboratory data produces a dangerous effect in hospital environments. This eventuality could contribute to increase the exposure time to contagion in critical departments such as the emergency room, surgery or intensive care.
According to our experience, it would be rejected only a small percentage of samples and the repetition of the swab collection does not impose particularly invasive procedures for the patient and is a quick activity for the health worker.
This type of recommendation could spur the health workers to put attention to the execution of the swab collection and to determine a future reduction of doubtful or false negative results.
The need to use simple techniques and to provide quick responses in contexts such as the current COVID-19 emergency, have certain contributed to the automation development in the molecular biology field.
This technical note remembers how the biologist individual professional skills are important to avoid laboratory responses that are increasingly entrusted to the technical result and how a sudden emergency like this COVID-19 pandemic, risks to reduce analytical accuracy.
References
- https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory-guidance
- https://www.360dx.com/coronavirus-test-tracker-launched-covid-19-tests
- Park NJ, Li Y, Yu T (2006) Characterization of RNA in Saliva Clin Chem 52 : 988-994.
- Bauer (2007) RNA in forensic science. Forensic Sci Int Genet 1: 69-74.
- Castagnola M (2011) Potential Applications of Human Saliva as Diagnostic Fluid. Acta OtorhinolaryngolItal 31: 347-357.
- Corman M(2020) Plenty of Coronaviruses but no SARS-CoV-2. Euro Surveill 25: 2000045.
- http://www.seegene.com/assays/allplex_2019_ncov_assay
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi