Editorial, Analg Resusc Curr Res Vol: 6 Issue: 1
Post-Surgical Pain: The Status of Evidence for the Use of Transcutaneous Electrical Nerve Stimulation (TENS)
Mark I Johnson*
Centre for Pain Research, School of Clinical and Applied Sciences, Leeds Beckett University City Campus, Leeds LS1 3HE, United Kingdom
*Corresponding Author : Mark I Johnson
Centre for Pain Research, School of Clinical and Applied Sciences, Leeds Beckett University City Campus, Leeds LS1 3HE, United Kingdom
Tel: 0113 81 23083
E-mail: m.johnson@leedsbeckett.ac.uk
Received: July 05, 2017 Accepted: July 07, 2017 Published: July 12, 2017
Citation: Johnson MI (2017) Post-Surgical Pain: The Status of Evidence for the Use of Transcutaneous Electrical Nerve Stimulation (TENS). Analg Resusc: Curr Res 6:1. doi:10.4172/2324-903X.1000e109
Abstract
The safety of surgical techniques has been identified as a publichealth concern. Surgery causes tissue damage to somatic, visceral and neural structures resulting in peripheral and central sensitisation of the nociceptive system and pain that may be nociceptive and/or neuropathic in origin. Acute post-surgical pain may be localised around the incision but may also spread because of soft tissue injury from surgical trauma and retraction. Pain may be at rest and/or on movement and paroxysmal without clear evoking stimuli. Pain may be accompanied by hyperalgesia, allodynia, hypaesthesia and dysaesthesia. Neuroplastic changes in the brain may contribute to the development of chronic post-surgical pain. The unique and complex pathophysiology of surgical pain means that pain management is challenging with a variety of pharmacological and non-pharmacological techniques available for use. However, inadequate management of post-surgical pain remains a problem and is known to increase the risk of developing moderate-to-severe acute and chronic post-surgical pain.
Keywords: Transcutaneous electrical nerve stimulation; Allodynia; Hypaesthesia; Dysaesthesia; hyperalgesia
The safety of surgical techniques has been identified as a publichealth concern [1]. Surgery causes tissue damage to somatic, visceral and neural structures resulting in peripheral and central sensitisation of the nociceptive system and pain that may be nociceptive and/or neuropathic in origin. Acute post-surgical pain may be localised around the incision but may also spread because of soft tissue injury from surgical trauma and retraction. Pain may be at rest and/or on movement and paroxysmal without clear evoking stimuli. Pain may be accompanied by hyperalgesia, allodynia, hypaesthesia and dysaesthesia. Neuroplastic changes in the brain may contribute to the development of chronic post-surgical pain. The unique and complex pathophysiology of surgical pain means that pain management is challenging with a variety of pharmacological and non-pharmacological techniques available for use [2]. However, inadequate management of post-surgical pain remains a problem and is known to increase the risk of developing moderate-to-severe acute and chronic post-surgical pain.
Strategies for post-surgical management aim to reduce suffering and facilitate mobilization including breathing deeply and normal coughing, eating and drinking because this reduces chest infection, hypoxia, cardiac problems, pressure sores, deep vein thrombosis, anorexia, wound infection, depression and anxiety [3]. Recent guidelines from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anaesthesiologist’s Committee on Regional Anesthesia, Executive Committee, and Administrative Council recommended that “…clinicians consider transcutaneous electrical nerve stimulation (TENS) as an adjunct to other post-surgical pain treatments (weak recommendation, moderate-quality evidence).” p137 [4]. Over the decades there has been a protracted debate about the efficacy of TENS for post-surgical pain. In 1990, the Royal College of Surgeons of England and the College of Anaesthetists recommended that TENS should not be offered for post-surgical pain and this may have resulted in TENS being used infrequently. Nowadays, local policy and practice dictates whether TENS is offered for post-surgical pain. The purpose of this Editorial is to outline the practicalities of using TENS for postsurgical pain and to discuss the findings from systematic reviews on clinical efficacy.
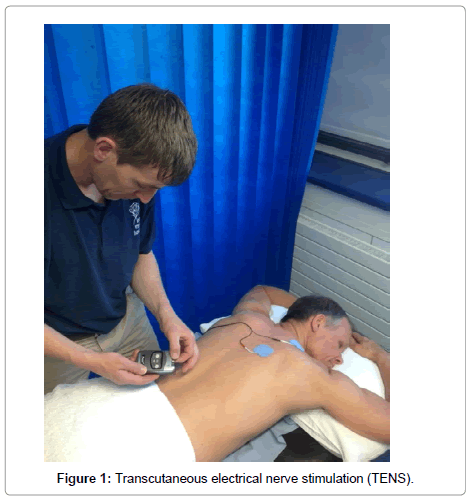
Transcutaneous electrical nerve stimulation is a non-invasive technique used to alleviate acute and chronic pain which improves activities of daily living [5]. Equipment to administer TENS is inexpensive and can be purchased without prescription (Figure 1). Transcutaneous electrical nerve stimulation can be self-administered with dosage adjusted according to need and a low risk of harm. Recently, a cost-effectiveness analysis of 88 randomised controlled clinical trials (RCTs, 7507 participants) found that TENS compared favourably against the quality-adjusted life year (QALY) threshold used by the National Institute of Health and Care Excellence (i.e. £20,000 GBP per QALY) for the management of pain associated with osteoarthritis of the knee, with an incremental cost-effectiveness ratio of £2,690 GBP per QALY versus usual care [6].
In post-surgical settings TENS is used to alleviate pain both as a stand-alone treatment and in combination with medication, with the potential to reduce analgesic consumption and associated side effects. Consequently, TENS may indirectly alleviate pulmonary atelectasis, post-surgical nausea and vomiting and ileus. TENS has an immediate onset of action, relieving pain as soon as the patient experiences a strong TENS sensation. In clinical practice this is achieved by turning a dial on the TENS device to increase the amplitude of current delivered to the skin. The rapid onset of action means that TENS is particularly useful for post-surgical pain which tends to be dynamic in nature with rapid fluctuations in severity. If pain suddenly increases in severity, as is the case during an episode of breakthrough pain, patients can immediately adjust the intensity of TENS to counteract the increase in pain intensity. This avoids the need to call a nurse for rescue medication. Likewise, by increasing the intensity of TENS prior to moving or coughing patients can pre-empt incident or coughrelated pain.
The first reports of the use of TENS in post-surgical settings emerged in the early 1970s. Hymes reported that TENS alleviated acute post-surgical pain, ileus and atelectasis and clinical trials quickly followed suggesting TENS was beneficial for abdominal or thoracic operative procedures, cardiac surgery, back surgery including laminectomies, arthroscopic knee surgery, total hip replacement, hip surgery and gynaecological laparotomies, and caesarean birth. Some studies found that TENS was not superior to placebo TENS or control groups for gastric bypass surgery, abdominal surgery, appendectomy, unilateral inguinal herniorrhaphy, caesarean section, elective cholecystectomy and decompressive lumbar laminectomy. Nowadays, TENS is used for acute post-surgical pain associated with incision and soft tissue trauma from a wide range of major and minor thoracic, abdominal and orthopaedic procedures. TENS is used for short-stay surgical procedures where the patient is fully conscious and alert including endoscopies, laser and dental surgery and for medical procedures including drain management and wound dressing changes. TENS has been used for procedural pain in adolescents and children as young as four.
The same principles and practice of TENS applies for post-surgical settings as for other pain conditions, paying particular attention to infection control [5]. There are excellent safety guidelines to direct clinical judgements [6,7]. Contraindications are often listed as cardiac pacemakers, pregnancy and epilepsy because it may be difficult to exclude TENS as a contributing factor if a problem arises. TENS can be used in these situations if it is applied to treat an unrelated pain that is distant from the affected area, although the patient must be monitored carefully. TENS should not be delivered close to transdermal drug delivery systems because of a possibility that currents may interfere with the delivery of the drug across the skin by the process of iontophoresis. Adverse events from TENS are rare and are generally minor skin irritation.
There are no robust indicators to identify whether a new patient will respond to TENS, and TENS may worsen pain in a minority of patients. Hence, trying TENS on the patient before surgery is advisable because some people do not like the sensation from TENS. TENS electrodes should be positioned so that TENS sensation covers pain. Generally, electrodes are placed around the site of pain, which is usually the incision site. Electrodes are usually positioned approximately 5cm either side of the suture line to reduce the chance of mechanical damage of the incision site when removing electrodes. Some patients may not be able to tolerate TENS at the incision site because of tenderness, hyperalgesia, tactile allodynia or dysaethesiae. In these cases, electrodes can be positioned along peripheral nerves proximal to the pain. Positioning electrodes along peripheral nerves is also useful when a body part has been removed (amputated), or if there is concern about damaged to the wound, or if skin is frail. Electrodes can also be placed at contralateral ‘mirror’ sites, paravertebrally on relevant dermatomes and on acupuncture points. Large areas of pain and multiple pains can be managed using dual channel TENS devices with four electrodes.
If a dressing is required electrodes should be applied in the operating theatre using aseptic procedures with the lead-wires protruding from the dressing to connect to the TENS device later. If a dressing is not required electrodes can be applied in the recovery room or ward. Infection control processes must be followed. TENS treatment can commence when the patient is sufficiently alert with either the patient or the nurse increasing current amplitude until a strong but comfortable TENS sensation is experienced. There should be no visible muscle twitching because the mechanical stress may hinder healing of the wound. Patients should be advised to experiment the pulse frequencies and pulse patterns of TENS to find TENS sensations that are most comfortable for them at that moment in time. Patients should be encouraged to adjust TENS settings as different settings may provide better relief at different times.
There are many systematic reviews that have attempted to evaluate the clinical efficacy of TENS for acute and for chronic pain including knee osteoarthritis, rheumatoid arthritis, low back pain, neck pain, post-amputation pain, post-stroke pain, spinal cord injury, diabetic peripheral neuropathy, chronic and recurrent headache, neuropathic pain, and cancer pain. The largest meta-analysis of TENS to date provided the evidence that TENS alleviated chronic musculoskeletal pain [8]. Often reviewers are unable to make definitive judgements about clinical efficacy because of inadequate RCT design, poor reporting and concerns about trial fidelity and TENS technique.
A Cochrane review of 19 RCTs (1346 participants) found that TENS was superior to placebo TENS as stand-alone treatment for acute pain in adults [9]. There were seven RCTs that investigated procedural pain in perioperative settings and four of these RCTs found that TENS was beneficial. Conditions included pelvic pain during office hysteroscopy (142 patients), pain during screening flexible sigmoidoscopy (90 patients), pain during unsedated colonoscopy (90 patients), pain during plastic surgery (100 patients). Three RCTS found that TENS did not confer benefit for procedural pain during laser treatment of the cervix (100 patients), intravenous needlestick techniques (71 blood donors), and flexible cystoscopy (148 patients). Simpson et al. [10] conducted a meta-analysis of four RCTs and found that TENS reduced moderate-to-severe acute lower back pain, acute pelvic pain, renal colic, and pain associated with hip fracture by 28-44 mm (95% CI) on a 100 mm visual analogue scale. They recommended TENS for use by emergency medical services in prehospital settings.
The early systematic reviews focussing on TENS for post-surgical pain were published in the 1990s and reported that TENS was not superior to controls. The first meta-analysis of TENS for postsurgical pain provided evidence that TENS reduced analgesic consumption if it was administered appropriately [11]. Strong non-painful TENS sensation at the site of pain (i.e. appropriate technique) reduced analgesic consumption by 35.5 % (range 14-51%) when compared with barely perceptible TENS that reduced analgesic consumption by 4.1 % reduction (range –10 to + 29%).
In recent years a series of systematic reviews, some with metaanalysis, provide a growing body of evidence that TENS has clinical utility in post-surgical settings. Freynet et al. [12] A reported that seven of nine RCTs found TENS reduced analgesic consumption and improved the duration of recovery room stay for patients with moderate pain associated with muscle sparing thoracotomy incision. Their review provided evidence that TENS was beneficial as a standalone treatment for mild post-thoracotomy pain (i.e. video-assisted thoracoscopy incision) but not for severe post-thoracotomy pain (i.e. posterolateral thoracotomy incision). In the same year, Sbruzzi et al. [13] provided evidence that TENS alleviated post-thoracotomy and sternotomy pain when combined with analgesic medication in a systematic review of 11 RCTs (570 patients). Subsequently, Kerai et al. [14] found that TENS reduced the severity of pain and analgesic consumption for a variety of surgical procedures (eight RCTs, 442 patients) although they noted that studies lacked adequate sample size, robust methodology and consistency in TENS parameters. Beckwee et al. [15] evaluated TENS for post-surgical knee arthroplasty pain (five RCTs, 347 patients) and reported that two studies found benefits during TENS. The three studies that did not find benefits delivered TENS at suboptimal stimulation intensities. Gajjar et al. [16] evaluated various analgesic treatments for colposcopy pain in women that included one RCT (100 women) which found that TENS did not provide additional benefit when combined with direct infiltration of lignocaine.
Studies in the 1970s provided evidence that TENS alleviated movement-evoked pain associated with deep breathing and cough, and improved peak expiratory flow rates, forced vital capacity (FVC), forced expiratory volume after one second (FEV1), functional residual capacity and partial pressure of O2 in arterial blood (Pa02) following upper abdominal and chest surgery. Patients had fewer pulmonary complications that diminish gaseous exchange and could better tolerate chest physical therapy. However, some studies have failed to find beneficial effects on pulmonary function. The findings from systematic reviews fail to resolve the inconsistency. Freynet et al. [12] reviewed six RCTs and reported improvements in FEV1, FVC, and coughing attempts where as Sbruzzi et al. [13] meta-analysed two RCTs and found no differences between TENS and placebo TENS in FVC following post-sternotomy, although a meta-analysis with so few participants is unlikely to be trustworthy.
Conclusion
Evidence from systematic reviews of placebo controlled trials suggests that TENS alleviates pain and reduces analgesic consumption when administered using appropriate technique. Indirect benefits include improvements in pulmonary mechanics and general mobilisation reducing the risk of chest infections, hypoxia, pressure sores and deep vein thrombosis. Thus, TENS should be considered as an adjunct to multimodal management, including analgesic medication, for the management of acute post-surgical pain. Nevertheless, RCTs on TENS often have small samples sizes which undermine confidence in the findings of systematic reviews. Metaanalyses of studies with small sample sizes have been shown to distort effect estimates of clinical efficacy. To improve confidence in estimates of clinical efficacy of TENS there needs to be pooling of data from RCTs with larger samples.
References
- Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, et al. (2008) An estimation of the global volume of surgery: A modelling strategy based on available data. Lancet 372: 139-144.
- Pogatzki-Zahn E, Segelcke D, Schug S (2017) Postoperative pain-from mechanisms to treatment. Pain Rep 2: e588.
- Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J (2016) Acute pain management: Scientific evidence, fourth edition, 2015. Med J Aust 204: 315-317.
- Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, et al. (2016) Management of postoperative pain: A Clinical practice guideline from the American pain society, the American society of regional anesthesia and pain medicine and the American society of Anesthesiologists' committee on regional anesthesia, executive committee and administrative council. J Pain 17: 131-157.
- Johnson MI (2014) Transcutaneous electrical nerve stimulation (TENS). Research to support clinical practice. Oxford University Press, UK.
- Woods B, Manca A, Weatherly H, Saramago P, Sideris E, et al. (2017) Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE 12: e0172749.
- Houghton P, Nussbaum E, Hoens A (2010) Electrophysical agents. Contraindications and precautions: An evidence-based approach to clinical decision making in physical therapy. Physiother Can 62: 5-80.
- Johnson M, Martinson M (2007) Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: A meta-analysis of randomized controlled trials. Pain 130: 157-165.
- Johnson MI, Paley CA, Howe TE, Sluka KA (2015) Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database Syst Rev 6: CD006142.
- Simpson PM, Fouche PF, Thomas RE, Bendall JC (2014) Transcutaneous electrical nerve stimulation for relieving acute pain in the pre-hospital setting: A systematic review and meta-analysis of randomized-controlled trials. Eur J Emerg Med 21: 10-17.
- Bjordal JM, Johnson MI, Ljunggreen AE (2003) Transcutaneous electrical nerve stimulation (TENS) can reduce postoperative analgesic consumption. A meta-analysis with assessment of optimal treatment parameters for postoperative pain. Eur J Pain 7: 181-188.
- Freynet A, Falcoz PE (2010) Is transcutaneous electrical nerve stimulation effective in relieving postoperative pain after thoracotomy? Interact Cardiovasc Thorac Surg 10: 283-288.
- Sbruzzi G, Silveira SA, Silva DV, Coronel CC, Plentz RD (2012) Transcutaneous electrical nerve stimulation after thoracic surgery: systematic review and meta-analysis of 11 randomized trials. Rev Bras Cir Cardiovasc 27: 75-87.
- Kerai S, Saxena KN, Taneja B, Sehrawat L (2014) Role of transcutaneous electrical nerve stimulation in post-operative analgesia. Indian J Anaesth 58: 388-393.
- Beckwee D, Bautmans I, Swinnen E, Vermet Y, Lefeber N, et al (2014) A systematic review investigating the relationship between efficacy and stimulation parameters when using transcutaneous electrical nerve stimulation after knee arthroplasty. SAGE Open Medicine 2.
- Gajjar K, Martin-Hirsch PP, Bryant A, Owens GL (2016) Pain relief for women with cervical intraepithelial neoplasia undergoing colposcopy treatment. Cochrane Database Syst Rev 7: CD006120.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi