Opinion Article, J Pls Sur Cos Vol: 5 Issue: 1
Plantations of Major Upper Extremities: Long-term Outcomes
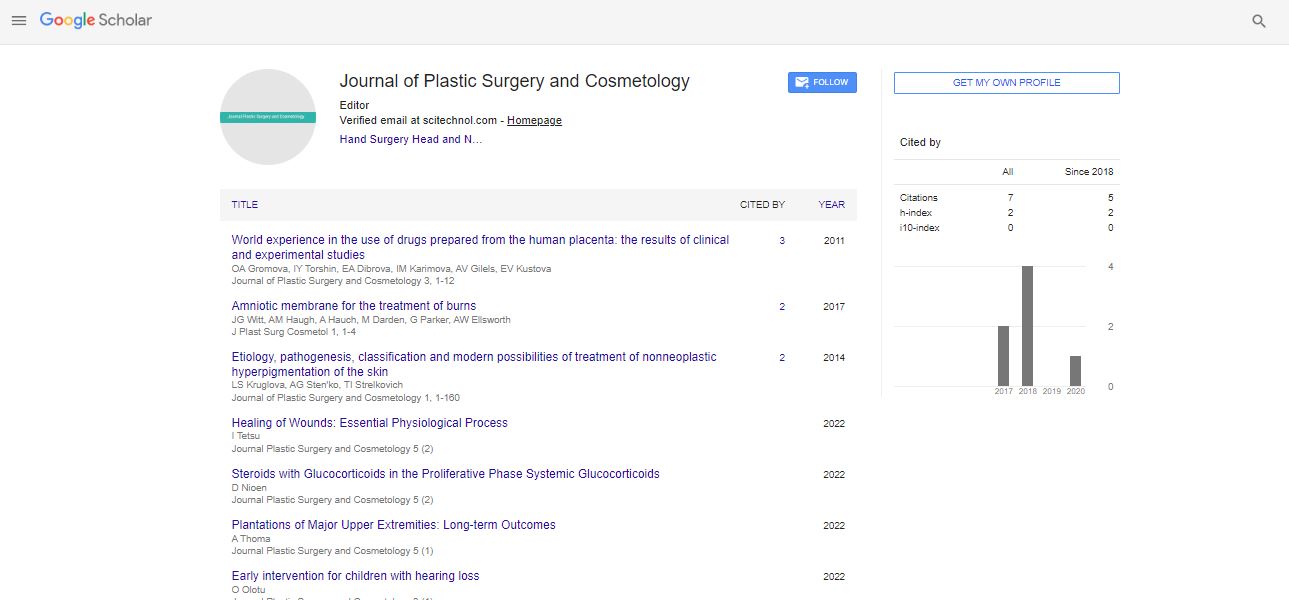
Achilleas Thoma*
Division of Plastic Surgery, McMaster University, Hamilton, Ontario
*Corresponding Author:
Achilleas Thoma
Division of Plastic Surgery, McMaster University, Hamilton, Ontario
E-mail:ac.retsamcm18@amohta
Received date: 04 February, 2022; Manuscript No. JPSC-22-56324;
Editor assigned date: 07 February, 2022; PreQC No. JPSC-22-56324(PQ);
Reviewed date: 17 February, 2022; QC No JPSC-22-56324;
Revised date: 28 February, 2022; Manuscript No. JPSC-22-56324(R);
Published date: 07 March, 2022; DOI: 10.4172/jpsc.100030.
Keywords: Plantations
Introduction
Upper extremity replantation, initially performed by Dr. Ronald Malt in Boston in 1962, is now commonly utilised to treat patients who have amputations of the thumb, multiple digits, hand, wrist, and forearm that are sharp, guillotine-type, and little polluted [1,2].
The most common criterion used to assess the success or failure of this operation is the survival of the transplanted extremity. It's been estimated to be between 80% and 94% [3]. This outcome measure, on the other hand, merely indicates if the replanted limb is functional at the follow-up appointment. More helpful outcome metrics are those that examine the surgical functional outcome, such as chen's criteria, the ability to return to work, range of motion in comparison to normal, sensibility, and power [4]. Assessments that cover both patient-reported quality of life and functional outcomes are ideal. These provide a more accurate indication of replantation success or failure.
Even though there is a risk of bias, clinician-measured physiological outcomes provide useful information about patient recovery status. For example, a surgeon may consider a viable replanted limb a success; yet, if the patient is unable to do the majority of his or her Activities of Daily Living (ADL) and requires social help, the treatment may be regarded a failure.
It's surprising that these outcomes have never been assessed using patient-reported outcome measures, given that major upper extremity replantation have been conducted and documented for more than three decades [5,6].
Amputation is a disfiguring procedure [7] that causes the patient significant psychological, social, vocational, and financial distress. As a result, it's critical to keep the patient at the centre of the replantation surgical outcome evaluation. Patients' experiences with disease and disability are increasingly being assessed using patient-reported outcome measures [8]. They represent the patient's perceived advantage or loss following surgery and are useful for preoperative and postoperative patient counselling. They are also used to determine the allocation of health-care resources and as standards for treatment efficacy.
The goal of this study was to use both objective and patient-reported outcome measures to examine the long-term effects of major upper extremity replantation. Amputations of the metacarpal, wrist, forearm, elbow, or arm are considered major upper extremity amputations [9]. The findings of this study, we feel, add to the substantial upper extremity replantation literature and highlight the benefits of using patient-reported outcome measures to assess surgical outcomes.
From 2002 to 2012, a retrospective chart study of all major upper extremity replantation performed at three McMaster University affiliated hospital sites in Hamilton, Ontario (Hamilton General Hospital, St Joseph's Healthcare Hamilton, and McMaster University Medical Centre) was conducted. All patients who had metacarpal, wrist, forearm, elbow, or arm amputations and underwent replantation surgery were included. Patients who had digital replantation were not included in the study.
Patient age, occupation, hand dominance, mode of injury, medical history, concurrent injuries, in-hospital services required, additional surgeries, complications, and the most recent follow-up appointment were all noted.
The research investigator (WN) or medical administrative assistants from each surgeon's office made at least three efforts to reach the included patients via phone. The study's goals were communicated to the patients, and they gave their informed consent. The Hamilton Integrated Research Ethics Board in Hamilton, Ontario, gave its approval to the project. These patients were invited back to the clinic for a follow-up visit.
Objective Measures
The study investigator took grip and strength measurements with a JAMAR dynamometer (Sammons Preston, USA) and a key pinch device during this follow-up session (WN). A two-arm goniometer was used to measure active range of motion. A padgett two-point discriminator was used to measure dynamic two-point discrimination in millimeters. All assessments were done twice (on both the afflicted and non-affected extremities), with the best effort from the two trials being recorded for analysis. The initial author carried out all of these measurements (WN).
Patient-reported outcome measures
The patients filled out a battery of three self-report questionnaires during their follow-up visits: The Disabilities of the Arm, Shoulder, and Hand (DASH) [10,11], the Michigan Hand Questionnaire (MHQ) [12-16], and the Hospital Anxiety and Depression Scale (HADS) [17-20]. Because the DASH and MHQ are the most commonly used patient-reported outcome measures in hand surgery, they were chosen. Meanwhile, a 30-item scale linked to upper extremity function is included in the DASH questionnaire. It is graded on a percentage scale (0 indicates no problems). These scales have been proven to be accurate in assessing impairments, activity limitations, and participation restrictions in everyday activities. The MHQ is made up of 37 hand-specific items that are grouped into five domains: Overall hand function, ADL, pain, work performance, aesthetics, and patient satisfaction with hand function.
Because it provides a psychological viewpoint on patients' well-being, the HADS was chosen. It's thought to be a useful screening tool for detecting concomitant anxiety and depression in people with musculoskeletal problems. The HADS is a self-administered questionnaire that is used to screen for depression and anxiety. The HADS was created to offer therapists with a practical measure for diagnosing and quantifying depression and anxiety that was acceptable, reliable, valid, and easy to use. The HADS scale cannot be used to make clinical diagnosis; however raw scores of 8 to 10 indicate mild instances, 11 to 15 moderate cases, and 16 severe cases.
Patient Characteristics
Between 2002 and 2012, 17 patients at the hospital centres (Hamilton General Hospital, St Joseph's Healthcare Hamilton, and McMaster University Medical Centre) underwent major upper extremity replantation surgery. All patients were replanted under general anesthesia with tourniquet control where possible, following a typical replantation procedure that began with bone stabilization and ended with graft placement. In none of these cases, arterial shunting was used.
The bulk of the patients in the study (16 of 17 (94.1%)) were men. Ten of the 17 patients (50.8%) worked as manual laborers in factories or construction sites, two (11.8 %) were students, one (5.9%) was a truck driver, and the remaining four (23.5%) did not describe their occupation. The patients' mean (SD) age at the time of injury was 45.513.0 years (range 14 years to 68 years). Eight patients (47.1%) had their metacarpals amputated, 6(35.3%) had their wrists amputated, and three had their forearms amputated (17.7%). Over a four-year follow-up period, 13(76.5%) of the 17 patients required reoperations, including five revision amputations (range 1 year to 10 years).
Replantation and Revascularizations
Previous investigations detailing upper extremity replantation and revascularizations found that functional results in using replanted upper extremities were reasonably consistent (between 88% and 94%) as subjectively stated by patients and through no standardized monitoring. However, the assessment and inclusion criteria in these studies varied, and the follow-up period was brief. The majority of studies that looked at the results of upper extremity replants employed objective or surgeon-reported criteria such Chen's criteria, range of motion, grip strength, and sensitivity. These metrics, however, only provide a limited picture of the patient's functional status. We report on the long-term results of upper extremity replantation in this study, utilizing both objective and patient-reported (i.e. DASH, MHQ and HADS) assessments. Furthermore, we chose to concentrate on major replantation rather than digital replantation because the latter is more common and extensively reported. Finally, no long-term significant replantation outcomes have been documented in any Canadian study to date.
Patients continued to have significant reductions in range of motion (reduced by 59.4% for the mean total active range of motion for the best digits in the replanted extremity compared to the no affected extremity) and grip strength even after a four-year follow-up (range 1 year to 10 years) (reduced by 87.4% compared with the no affected extremity). The best digital dynamic two-point discrimination was good, it should be mentioned (mean 7 m, range 5 mm to 9 mm). The individuals were found to have mild depression and anxiety symptoms, as measured by the HADS. We were unable to collect the baseline status (i.e. immediate postoperative) of the included patients due to the nature of the study design.
References
- Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: The DASH (Disabilities of the Arm, Shoulder, and Hand) (corrected). The Upper Extremity Collaborative Group (UECG). Am J Industr Med 29: 602-608. [Crossref],[Google Scholar],[Indexed]
- Chung KC, Pillsbury MS, Walters MR, Hayward RA (1998) Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg 23: 575-587. [Crossref],[Google Scholar],[Indexed]
- Dias JJ, Rajan RA, Thompson JR (2008) Which questionnaire is best? The reliability, validity and ease of use of the patient evaluation measure, the Disabilities of the Arm, Shoulder and Hand and the Michigan Hand Outcome Measure. J Hand Surg Eur Vol 33: 9-17. [Crossref],[Google Scholar],[Indexed]
- Hoang-Kim A, Pegreffi F, Moroni A, Ladd A (2011) Measuring wrist and hand function: Common scales and checklists. Injury 42: 253-258. [Crossref],[Google Scholar],[Indexed]
- Shauver MJ, Chung KC (2009) The minimally clinically important difference of the Michigan Hand Outcomes questionnaire. J Hand Surg 34: 509-514. [Crossref],[Google Scholar],[Indexed]
- Waljee JF, Chung KC, Kim HM, Patricia BB, Frank DB, et al. (2010) Validity and responsiveness of the Michigan hand questionnaire in patients with rheumatoid arthritis: A multicenter, international study. Arthr Care Res 62: 1569-1577. [Crossref],[Google Scholar],[Indexed]
- Crawford JR, Henry JD, Crombie C, Taylor EP (2001) Brief report: Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol 40: 429-434. [Crossref],[Google Scholar], [Indexed]
- Crawford JR, Garthwaite PH, Lawrie CJ, Julie DH, Marie AMD, et al. (2009) A convenient method of obtaining percentile norms and accompanying interval estimates for self-report mood scales (DASS, DASS-21, HADS, PANAS, and sAD). Br J Clin Psychol 48: 163-180. [Crossref],[Google Scholar], [Indexed]
- Harter M, Reuter K, Gross-Hardt K, Bengel J(2001) Screening for anxiety, depressive and somatoform disorders in rehabilitation validity of HADS and GHQ-12 in patients with musculoskeletal disease. Disabil Rehabil 23: 737-744. [Crossref],[Google Scholar], [Indexed]
- Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 67: 361-370. [Crossref],[Google Scholar], [Indexed]
- Berger A, Millesi H (1980) Functional results from replantation surgery: A five year report from the Viennese replantation team. Austral NZ J Surg 50: 244-247. [Crossref],[Google Scholar],[Indexed]
- Kleinert HE, Jablon M, Tsai TM (1980) An overview of replantation and results of 347 replants in 245 patients. J Trauma Acute Care Surg 20: 390-398. [Crossref],[Google Scholar], [Indexed]
- Russell RC, O'Brien BM, Morrison WA, Pamamull G, MacLeod A (1984) The late functional results of upper limb revascularization and replantation. J Hand Surg 9: 623-633. [Crossref],[Google Scholar],[Indexed]
- Scott FA, Howar JW, Boswick JA (1981) Recovery of function following replantation and revascularization of amputated hand parts. J Trauma Acute Care Surg 21: 204-214. [Crossref],[Google Scholar], [Indexed]
- Davidson J (2004) A comparison of upper limb amputees and patients with upper limb injuries using the Disability of the Arm, Shoulder and Hand (DASH). Disabil Rehabil 26: 917-923. [Crossref],[Google Scholar],[Indexed]
- Ostlie K, Franklin RJ, Dip Phys G, Anders Skrondal, Per Magnus (2011) Assessing physical function in adult acquired major upper-limb amputees by combining the Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire and clinical examination. Arch Phys Med Rehabil 92: 1636-1645. [Crossref],[Google Scholar],[Indexed]
- Friedrich JC, Poppler LH, Mack CD, Frederick PR, Scott LL, et al. (2011) Epidemiology of upper extremity replantation surgery in the United States. J Hand Surg 36: 1835-1840. [Crossref],[Google Scholar], [Indexed]
- Laing TA, Cassell O, O'Donovan D, Eadie P (2012) Long term functional results from major limb replantations. J Plast Reconstr Aesthet Surg 65: 931-934. [Crossref],[Google Scholar], [Indexed]
- Raja SS, Venkatramani H, Bharathi RR, Dheenadhayalan J, Bhat VR, et al. (2007) Technical considerations and functional outcome of 22 major replantations. J Hand Surg Eur 32: 488-501. [Crossref],[Google Scholar], [Indexed]
- Daoutis NK, Gerostathopoulos N, Efstathopoulos, Misitzis D, Bouchlis G, et al. (1995) Major amputation of the upper extremity: Functional results after replantation/revacularization in 47 cases. Acta Orthop Scand 264: 7-8. [Crossref],[Google Scholar], [Indexed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi