Research Article, Androl Gynecol Curr Res Vol: 5 Issue: 4
Peri-ovulatory Phytoestrogen Improves Pregnancy Rate in Women with Polycystic OvarianSyndrome Receiving Ovulation Induction with Clomiphene Citrate
Reham Elkhateeb*
Department of Obstetrics and Gynecology, Faculty of Medicine, Minia University, Egypt
*Corresponding Author : Reham Elkhateeb
Department of Obstetrics and Gynecology, Faculty of Medicine, Minia University, Egypt
Tel: 201000222994
E-mail: rehamelkhateeb78@yahoo.com
Received: December 13, 2017 Accepted: December 19, 2017 Published: December 23, 2017
Citation: Elkhateeb R (2017) Peri-ovulatory Phytoestrogen Improves Pregnancy Rate in Women with Polycystic Ovarian Syndrome Receiving Ovulation Induction with Clomiphene Citrate. Androl Gynecol: Curr Res 5:4. doi: 10.4172/2327-4360.1000158
Abstract
Abstract Background: PCOS is the most common ovarian factor of female infertility, in low resource countries clomiphene citrate is the most popular drug used for induction of ovulation as its price is affordable for most of patients with least side effects. Objective: Evaluate the effect of phytoestrogen in women receiving induction with clomiphene citrate when given peri ovulatory to oppose antiestrogenic effect of clomiphene citrate. Methodology: Prospective study conducted on 500 patients with PCOD who attended infertility clinic, patients were randomized into 2 groups both groups received traditional CC induction , group (1) 225 patients received phyto-estrogen, starting in the 7th day of the cycle till the day of HCG injection ,group(2) 225 patients received clomiphene citrate only. Endometrial thickness and follicular growth were assessed by transvaginal US. When follicles reached 18 mm, 10,000 IU HCG was administered together with timed intercourse. Both groups were compared as regard cumulative pregnancy rate, ovulation, endometrial thickness and change in hormonal milieu. Results: Midluteal serum progesterone was significantly higher in the study group as compared with the control group (15.93 ±1.8 versus 12.93 ± 1.8); endometrial thickness was also greater in the study group as compared with the control group, (10.3 ± 1.1 versus 8.2 ± 0.9). Ovulation in the three cycles was in favor of study group 82.5% versus 80.4% but not statistically significant. The CPR was significantly higher in the study group than in the control group (34.2% vs. 20.8%. P = 0.1). There were 6 cases of multiple pregnancy in the study group and 4 cases in the control group. Conclusion: Adding phytoestrogen to CC induction improve ovulation and pregnancy rate, it is a good option for patients with PCOS seeking for pregnancy treatment with affordable price and minimal side effects
Keywords: Polycystic ovary syndrome; Clomiphene citrate; Phytoestrogen
Introduction
Polycystic ovary syndrome (PCOS) is the most common cause of an ovulatory infertility accounting for 70-80% of cases it affects 4-18% of females in childbearing period [1,2]. The diagnosis of PCOS is based on the Rotterdam criteria in which at least two of the following three criteria are met: 1) oligo or anovulation, 2) clinical or biochemical hyperandrogenaemia, 3) polycystic ovaries (>12 follicles <10 mm and/or ovarian volume >10 ml per ovary by vaginal ultrasound [3,4]. Clomiphene citrate (CC) is considered as the first line treatment used for ovulation induction in women with PCOS. It acts through anti-estrogenic effect on the hypothalamus by binding to estrogenic receptors; an action that stimulates gonadotropin releasing hormone (GnRH) pulse which in turn induces gonadotropin release from the anterior pituitary gland [5,6]. The ovulation rate with CC is 80%; however, the cumulative pregnancy rate (CPR) is 30-40% [7]. This discrepancy between ovulation and CPR can be attributed to the anti-estrogenic effect of CC on the endometrium and cervical mucus; endometrium is significantly thin in women receiving CC induction [8,9]. Phytoestrogen (Cimicifugaracimosa extract) it is an alternative to estrogen, originally used to alleviate menopausal symptoms. The mechanisms of action of various phytoestrogens have been reviewed recently its estrogenic action is evident [10-13]. The aim of this study was to evaluate the effect of adding phytoestrogen to CC during ovulation induction in women with PCOS on the ovulation rate, pregnancy rate and hormonal profile.
Materials and Methods
This study is a prospective randomized controlled trial conducted at Maternity Hospital and some private clinics during from September 2015 to August 2017. Ethical approval for the study was obtained from the local ethical committee of the department of Obstetrics and Gynecology; Minia University. All participants gave written informed consents before being enrolled in the study. Inclusion criteria for the study were: a) age between 18-35 years, b) diagnosis of PCOS according to Rotterdam criteria, c) proved potency of at least one fallopian tube and d) normal semen analysis of the male partner. Women with history of prior ovulation induction cycles, laparoscopic ovarian drilling (LOD) and women with distorted uterine cavity were excluded from the study.
All participants were subjected to thorough history taking, examination and baseline hormonal assessment. Patients were randomized at the beginning of the study into two groups by sealed envelopes containing computer random generated numbers. All participants received CC 100 mg orally for five days starting from cycle day 2. Patients in the study group received phytoestrogen (klimadynon®, Bionorica, neumarketi.dOBf., Germany) 20 mg daily staring from cycle day 7 till day of HCG injection. Patients in the control group received placebo tablets in the same days as in the study group. The treatment was double blinded to the patients and the doctors who prescribed the treatment. The study was prospectively registered in PCTR and its unique ID number is PACTR201510001265121. Cycle monitoring was done using transvaginal ultrasound to assess endometrial thickness and follicular development. Scanning was started on cycle day 9 and then every other day till a follicle of 18 mm in diameter, HCG was given at a dose of 10000 IU IM. Patients were advised to have intercourse every other day. Once a follicle of 14 mm in diameter was reached. Serum FSH and LH and midluteal progesterone levels were assessed every treatment cycle. Patients were followed up to three treatment cycles.
Study outcome measures
Primary outcome measure of the study was ovulation rate and clinical pregnancy defined as detected fetal pulsation with ultrasound two weeks after a positive pregnancy test. Secondary outcome measures of the study were midluteal phase progesterone level and endometrial thickness.
Sample size calculation
Sample size was calculated to prevent type II error. CPR with CC at the unit where the study was conducted was 32%. To be of clinical significance, it was assumed that addition of phytoestrogen to CC will achieve a CPR of 50%. Based on these data, we would need to study 91 patients in each arm to be able to reject the null hypothesis that the rates for study and control groups are equal in CPR with a probability of 80%. The type one error probability associated with this test for the null hypothesis is 0.05. To compensate for discontinuation, we recruited 225 patients in each arm.
Statistical analysis
The Statistical analysis was performed using Statistical Package for Social Science (SPSS Inc, Chicago) version 21 for Microsoft Windows. Data were described in terms of mean ± SEM (standard error of the mean) for continuous variables and frequencies (number of cases) and percentages for categorical data. Independent Student‘s t-test was used to compare quantitative variables and Chi square test was used to compare categorical data. P<0.05 was considered significant.
Results
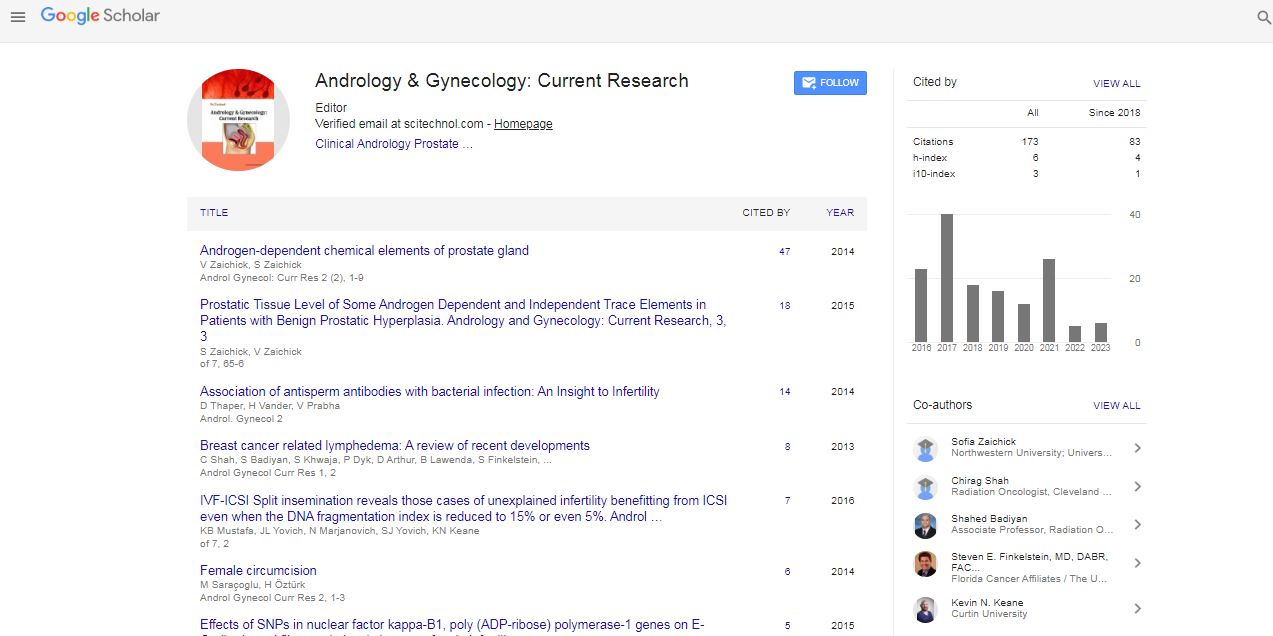
The study included 500 patients. There was no significant difference in the demographic features and baseline hormones between the two groups as shown in Table 1.
| Phytosetrogen group | Control group | P value | |
|---|---|---|---|
| Age | 25.1 ± 2.11 | 24.3 ± 3.0 | 0.71 |
| BMI | 30.1 ± 3.25 | 31.6 ± 2.61 | 0.83 |
Infertility types:
|
115 110 |
125 100 |
|
| Infertility durations | 4 ± 0.23 | 3 ± 0.15 | 0.32 |
Menstrual patterns:
|
15 170 40 |
10 185 30 |
|
| Clinical hyperandrogenism: Acne Hirsutism |
90 35 75 |
85 40 90 |
|
| FSH | 5.1 ± 2.1 | 4.8 ± 2.1 | 0.10 |
| LH | 12.9 ± 1.92 | 11.6 ± 1.81 | 0.04* |
Table 1: Demographic features and hormonal melieu in the study population.
Discussion
In the current study, we assessed the effect of adding the PE to CC during ovulation induction in women with PCOS. The study proved a benefit of PE in terms of improving the CPR in addition to improving the endometrial thickness and increasing mid-luteal serum progesterone levels. The exact mechanism of PE is still unclear. There are three postulated mechanisms for its action (Table 2). The first theory states that a high dose of PE displaces the endogenous estrogen and binds to its receptors or affects the tissue expression of estrogenreceptor subtypes the second theory suggests that PE competes with the anti-estrogenic isomer of clomiphene for estrogen receptors and has a less potent anti-estrogenic effect than the clomiphene cis-isomer [14]. The third theory suggests that PE acts through displacement of clomiphene ligands from estrogen receptors [15]. The rationale for using PE in this study was trying to reverse the anti-estrogenic effect of CC on the endometrium and the cervical mucus which may be responsible for the marked discrepancy between the ovulation rate and the cumulative pregnancy rate achieved with CC. A study was done by Kamel comparing CC with PE alone failed to find a significant difference in the CPR between the two groups. However, the endometrial thickness and the improvement of hormonal milieu were in favor of the PE group [16].
| First cycle | Second cycle | Third cycle | P value | ||||
|---|---|---|---|---|---|---|---|
| PE group | Control group | PE group | Control group | PE group | Control group | ||
| No. of follicles=17mm | 2.3 ± 0.1 | 2.1 ± 0.15 | 2.4 ± 0.9 | 2.3 ± 0.1 | 3.7 ± 0.5 | 3.2 ± 0.8 | NS |
| Endometrial thickness on HCG day | 8.9 ± 1.4 | 7.5 ±1.3 | 9.3 ± 0.81 | 7.8 ± 0.3 | 10.3 ± 1.1 | 8.2 ± 0.9 | <0.001* |
| Serum estradiol on HCG day (pg/ml) | 254 ± 20.9 | 252 ± 20.6 | 268 ± 21.8 | 260 ± 29.8 | 274.5 ± 48.5 | 267 ± 22.1 | NS |
| Midluteal serum progesterone(ng/ml) | 11.2 ± 0.8 10 | 8.3 ± 0.81 | 14.3 ± 1.1 | 11.3 ± 1.1 | 15.93 ± 1.8 | 12.93 ± 1.8 | 0.04* |
| Ovulation | 57 | 55 | 61 | 60 | 68 | 66 | NS |
| Clinical pregnancy | 19 | 7 | 26 | 14 | 32 | 26 | |
| Multiple pregnancy | 1 | 0 | 2 | 1 | 3 | 2 | |
| Miscarriage | 1 | 1 | 1 | 1 | 1 | 2 | |
| OHSS | 0 | 0 | 2 | 1 | 1 | 3 | |
Show main outcome in both groups: midluteal serum progesterone level was significantly higher in the phytoestrogen group as compared with the control group (15.93 ± 1.8 versus 12.93 ± 1.8); endometrial thickness was also greater in the phytoestrogen group as compared with the control group, (10.3 ± 1.1 versus 8.2 ± 0.9). Ovulation in the three cycles was in favor of study group 82.5% versus 80.4% but not statistically significant. The CPR was significantly higher in the phytoestrogen group than in the control group (34.2% vs. 20.8%. P = 0.1). There were 6 cases of multiple pregnancy in the study group and 4 cases in the control group.
Table 2: Outcome measures in the two groups.
In our study the number of dominant follicles and rate of ovulation in women received CC alone was less than women received CC with PE but the difference was not statistically significant this was not in accordance with results were found by Maged, et al. ovulation rate was (82% vs. 100% respectively) this may difference in timing of start PE in our study it was started in the 7th day while Ahmed M Maged, et al. [17] started in the second day of the cycle. As regard endometrial thickness it was better in PE group 10.3 ± 1.1 versus 8.2 ± 0.9 in control group same was found by Shahin and Mohamed found that women received phytoestrogen had thicker endometrium than those who received CC alone 12.5 ± 1.9 versu 8.5 ± 1.9 [18]. In our study CPR in women received CC alone was lower than pregnancy rate in women received CC and phytoestrogens (34.2% versus 20.8%). Same was found by Shahin and Mohamed PE plus CC group had significantly higher clinical pregnancies per cycle (33/192 (17.2%) versus 71/204 (34.8%), p < 0.01), compared to the CC only group. But Kamel found higher but clinically insignificant pregnancy rate between two groups [16]. Unfer et al. in their randomized double blind study evaluated the synergetic effect of phytoestrogens with CC in induction of ovulation during preparation of infertile women with PCOD for intrauterine insemination [14]. They found a statistically significant difference between the 2 groups regarding endometrial thickness it was thicker in group 2. They reached the conclusion that high doses of phytoestrogens administration have the ability to reverse the antiestrogenic effects of CC on endometrial thickness consequently contributed to increase pregnancy rates, while the clinical pregnancy rate in another study showed that no statistically significant difference between the 2 groups (14.0% versus 21.1%, respectively) in Shahin et al., explanation of difference in CPR in our research than others, is timing of start of PE is periovulatory both to decrease antiestrogenic effect of CC on cervical mucous and good preparation of endometrial receptivity at time of ovulation but more prospective study is indicated to confirm our conclusion [19].
Acknowledgement
No financial support was provided by any pharmaceutical company to conduct current research. The author thanks all the infertility clinics that have given their help in recruiting women for this study.
Disclosure
The author declares that there is no conflict of interest.
References
- Homburg R (2004) Management of infertility and prevention of ovarian hyperstimulation in women with polycystic ovary syndrome. Best Prac Res Clin Obstet Gynaecol 18: 773-788.
- Moran LJ, Hutchison SK, Norman RJ, Teede HJ (2011) Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev 16.
- The Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod 19: 41-47.
- Chakraborty P, Goswami SK, Rajani S, Sharma S, Kabir SN, et al (2013) Recurrent pregnancy loss in polycystic ovary syndrome: role of hyperhomocysteinemia and insulin resistance. PLoS One 8.
- Homburg R (2005) Clomiphene citrate–end of an era? A mini-review. Hum Reprod 20: 2043-2051.
- Kousta E, White DM, Franks S (1997) Modern use of clomiphene citrate in induction of ovulation. Hum Reprod Update 3: 359-365.
- Havelock JC, Bradshaw KD (2007) Ovulation induction. In Reproductive Endocrinology and Infertility. (Vivian Lewis edi.) Landes bioscience, Austin, Texas United State of America.
- Dehbashi S, Parsanezhad ME, Alborzi S, Zarei A (2003) Effect of clomiphene citrate on endometrium thickness and echogenic patterns. Int J Gynaecol Obstet 80: 49-53.
- Haritha S, Rajagopalan G (2003) Follicular growth, endometrial thickness, and serum estradiol levels in spontaneous and clomiphene citrate-induced cycles. Int J Gynaecol Obstet 81: 287-292.
- Dang ZC (2009) Dose-dependent effects of soy phyto-oestrogen genistein on adipocytes: mechanisms of action. Obes Rev 10: 342-349.
- Li Y, Tollefsbol TO (2010) Impact on DNA methylation in cancer prevention and therapy by bioactive dietary components. Curr Med Chem 17: 2141-2151.
- Lorand T, Vigh E, Garai J (2010) Hormonal action of plant derived and anthropogenic non-steroidal estrogenic compounds: phytoestrogens and xenoestrogens. Curr Med Chem 17: 3542-3574.
- Shanle EK, Xu W (2011) Endocrine disrupting chemicals targeting estrogen receptor signaling: identification and mechanisms of action. Chem Res Toxicol 24: 6-19.
- Unfer V, Casini ML, Costabile L, Mignosa M, Gerli S,et al (2004) High dose of phytoestrogens can reverse the antiestrogenic effects of clomiphene citrate on the endometrium in patients undergoing intrauterine insemination: a randomized trial. J Soc Gynecol Investig 11: 323-328.
- Casper RF (2004) Phytpestrogens, clomiphene, and the uterus. Journal of the Society for Gynecologic Investigations 11: 261-262.
- Kamel HH (2013) Role of phyto-oestrogens in ovulation induction in women with polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol 168: 60-63.
- Ahmed M Maged, Wessam S Deeb (2015) Phytoestrogens as an alternative to estradiol in reversing the antiestrogenic effect of clomid on endometrium in ovulation induction in cases of polycystic ovarian syndrome (PCOS) Uterus & Ovary 1.
- Shahin AY, Mohammed SA (2014) Adding the phytoestrogen Cimicifugae Racemosae to clomiphene induction cycles with timed intercourse in polycystic ovary syndrome improves cycle outcomes and pregnancy rates-a randomized trial. Gynecol Endocrinol 30: 505-510.
- Shahin AY, Ismail AM, Shaaban OM (2009) Supplementation of clomiphene citrate cycles with Cimicifugaracemosa or ethinyloestradiol--a randomized trial. Reprod Biomed Online 19: 501-507.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi