Research Article, J Trauma Stress Disor Treat Vol: 8 Issue: 2
Outcome Expectancy for Prolonged Exposure Therapy Predicts Symptom Improvement in Veterans with Post-Traumatic Stress Disorder
Hannah C McLane1*, J Ben Barnes2, Frances S Shofer3and Jason T Goodson2
1Philadelphia VA Medical Center, Occupational and Environmental Medicine, 3900 Woodland Ave, Philadelphia, PA 19104, USA
2Corporal Michael J Crescenz Veterans Affairs Medical Center, University of Pennsylvania, PA 19104, USA
3Department of Emergency Medicine, Perelman School of Medicine, University of Pennsylvania, PA 19104, USA
*Corresponding Author: Hannah C McLane
Philadelphia VA Medical Center
Occupational and Environmental Medicine 3900 Woodland Ave
Philadelphia, PA 19104, USA
Tel: +1 215-823-5850
E-mail: hannahcmclane@gmail.com
Received date: January 19, 2019; Accepted date: February 18, 2019; Published date: February 25, 2019
Citation: McLane HC, Barnes JB, Shofer FS, Goodson JT (2019) Outcome Expectancy for Prolonged Exposure Therapy Predicts Symptom Improvement in Veterans with Post-Traumatic Stress Disorder. J Trauma Stress Disor Treat 8:2.
Abstract
Objective: This study explores outcome expectancies – how much a patient believes a therapy will result in improvement – as a predictor of outcome of prolonged exposure therapy (PE) in veterans with PTSD.
Methods: Prior to PE therapy, veterans were administered a PTSD treatment expectations (PTE) survey consisting of three 11-point Likert scale questions with possible scores of 0-30. The primary outcome was changes in total PTSD Checklist for DSM-5 (PCL-5) scores before and after PE therapy. ANOVA in repeated measures was used to evaluate the association between PTE tertiles and PTSD symptom changes.
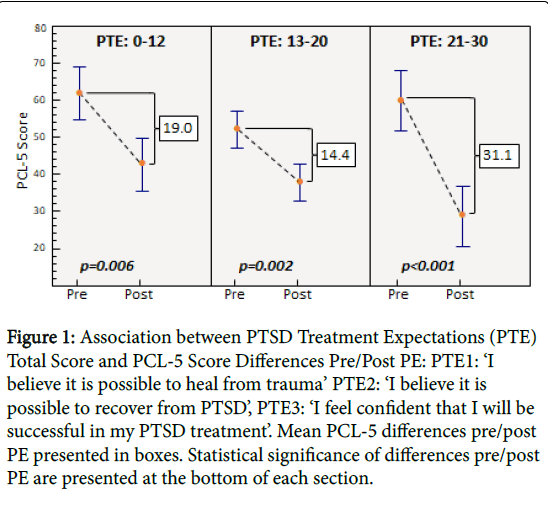
Results: 57 veterans consented and 35 (61.4%) completed therapy. Mean differences in PCL-5 scores pre-/post-PE were 19.0, 14.4, and 31.1 (p<0.0006 for all) in the low (0-12), middle (13-20) and high (21-30) PTE tertiles, respectively.
Conclusions: Consistent with current literature, our study shows that PTSD outcome expectancy may be useful in predicting treatment response to PE.
Keywords: PTSD; Post-traumatic stress disorder; Trauma; Expectancy; Expectations; Prolonged exposure therapy; veterans
Keywords
PTSD; Post-traumatic stress disorder; Trauma; Expectancy; Expectations; Prolonged exposure therapy; veterans
Introduction
Post-traumatic stress disorder (PTSD) represents a significant cause of morbidity among veterans; prevalence rates vary widely by war and era, but lifetime prevalence of PTSD among veterans from the Vietnam Era to present have been estimated at 10-30% [1]. Prolonged Exposure Therapy (PE) has been shown to be an effective treatment for PTSD in Veteran populations, although there is variability in treatment response among patients and significant amounts of dropout [2]. While results have not always been consistent, research evidence has converged on a small number of factors found to be associated with outcome, including female gender [3,4] service-connected disability status, therapist experience and age [3,5]. Given the relatively high rates of dropout (16-44%) and non-response (30-37%) to PE [2,3,6] it continues to be important to identify factors associated with PTSD treatment outcomes.
One patient factor of interest in regards to treatment outcomes is outcome expectancy [1], which has been defined as “the degree to which a client believes that therapy will result in improvement” [7]. Outcome expectancy has consistently been shown to predict treatment response in a number of different patient groups, including those with social phobia [8], anxiety disorders [9], and depression [10]. Existing measures of outcome expectancy vary in item content and scoring structure, but the most widely used measure is the credibility and expectancy questionnaire (CEQ) [11].
Few research studies have investigated the impact of outcome expectancy in PE treatment outcomes with veterans. Collins and Hyer in 1986 found that treatment expectancy was related to hospital treatment outcome in 11,283 Veterans admitted to inpatient psychiatric wards [12]. Price et al. conducted a study in which they examined outcome expectancies in 116 combat Veterans with PTSD undergoing virtual reality exposure therapy. Results suggested that outcome expectancies were associated with the magnitude of symptom change as reported by both patients and clinicians [7].
Given the paucity of data regarding associations between outcome expectancy and PTSD outcomes in PE, we conducted a study to evaluate this relationship in a sample of veterans undergoing outpatient PTSD Prolonged Exposure Therapy using a newly developed PTSD-specific expectancy measure. We hypothesized that veterans with higher outcome expectancy would show larger improvements in symptoms than those with lower outcome expectancy.
Materials and Methods
This was a cohort study of veterans being treated at a VA Medical Center who met criteria for the diagnosis of PTSD and were undergoing PE treatment. Data were collected in a naturalistic clinical setting in the general outpatient mental health clinic in a large urban VA medical center in the northeastern United States. Participants were diagnosed with PTSD and deemed appropriate for PE by their respective treatment providers. Treatment expectancies were measured before session one (see below for a detailed description of this measure) and PTSD symptoms were measured using the PCL-5 assessment before session one and at the final session of PE. The project was determined by the Corporal Michael J. Crescenz Veterans Affairs Medical Center’s Internal Review Board to meet criteria for quality management and was approved to be published as such.
Participants
Eligible veterans for this study included those meeting the following criteria: (1) their treating clinicians deemed them appropriate for PE (i.e. no immediate threat of harm to self or others, no non-PTSD related psychosis or uncontrolled bipolar disorder, and no severe TBI), (2) they agreed to initiate PE, and (3) they completed self-report assessments before treatment began.
Therapists
Prolonged Exposure therapy was provided by 18 different therapists. Seven of the therapists were licensed staff psychologists, one was a clinical nurse specialist, and 10 were psychology interns. All licensed providers were certified VA PE providers or undergoing consultation for the certification process. All of the interns received initial training by an officially certified PE trainer and all cases were supervised by official VA PE providers. All cases completed by interns were also audio-recorded and reviewed; feedback was given in weekly individual and group supervision meetings.
Treatment
Prolonged Exposure Therapy is a trauma-focused, cognitivebehavioral therapy consisting of approximately nine to fifteen individual sessions, each 90 minutes in length. The primary interventions consist of psychoeducation, breathing retraining, and imaginal (the memory) and in vivo (avoided external trauma reminders) exposure with a strong emphasis on repeated exposures completed within and between sessions.
Measures
PTSD severity measure: Symptoms of PTSD were assessed using the PTSD Checklist for DSM-5 (PCL-5) [13]. The PCL-5 is a self-report measure consisting of 20 items corresponding to the 20 DSM-5 PTSD symptom criteria (e.g. Feeling jumpy or easily startled; Trouble falling or staying asleep). Respondents indicate severity of each item by indicating how much they are bothered by symptoms in the past13 month on a 5-point Likert scale (0=not at all; 4=extremely). Individual items can be summed to provide a total score (0 – 80), with higher scores indicating greater severity of PTSD symptoms. The PCL-5 has demonstrated good psychometric properties [13-15].
Expectancy measure: For the current study a new expectancy measure was developed by one of the investigators (JTG), called the PTSD Treatment Expectancies (PTE). This measure was designed to include several core features: (1) it is specific to PTSD and trauma, (2) it is brief (3-items) and user-friendly (0-10 scale without semantic anchors to be interpreted), and (3) it contains items that assess outcome expectancy related to trauma recovery, PTSD symptom recovery, and self-efficacy. Participants are asked how much they agree or disagree with three statements on an 11-point Likert scale; possible total scores range from 0-30. The statements in the PTE are the following: (1) I believe it is possible to heal from trauma; (2) I believe it is possible to recover from PTSD; and (3) I feel confident that I will be successful in my PTSD treatment.
Statistical Analysis
The outcome measured was change in the total PTSD Checklist for DSM-5 (PCL-5) scores pre/post PE therapy. To examine differences in completers versus non-completers, Fisher’s exact tests were used for categorical variables, and 2-sample t-tests for continuous variables. To assess improvement in PCL-5, the paired t-test was used. To evaluate the relationship between the overall PTE score, with regard to PCL-5 score pre/post PE therapy, analysis of variance in repeated measures (ANOVA-RM) was used, where PTE score was a grouping factor (treated as an ordinal variable with 3 categories: 0-12, 13-20, 21-30) and time pre/post PE therapy was the repeated measure. To determine if a single PTE question is associated with PCL-5 improvement, each question was evaluated separately, using ANOVA-RM, where the categories were 0-4, 5, and 6-10. All analyses were performed using SAS statistical software (version 9.4, SAS Institute, Cary NC).
Results
Of 57 veterans that consented, 35 (61.4%) completed the therapy, with median number of sessions being 10 (range 7-20). Because this was a naturalistic clinical setting, veterans who did not successfully complete the PE protocol were not asked to complete post-treatment self-report measures and were thus considered non-completers. Completers were 80% male, 57% black, 40% white, mean age of 58.2 years (range 25 – 75, Table 1). Fifty-seven percent of veteran’s PE therapy was focused on combat-related trauma, 14.3% on Military Sexual Trauma (MST), and 28.6% on other traumas. Completers and non-completers did not differ with regard to gender, race, trauma type, Patient Health Questionnaire scores (PHQ-9, a depression screening measure), or PCL-5 scores. However, completers were significantly older compared to non-completers (58.2 vs 50.3 years of age, p=0.05). Additionally, no differences were found regarding PTE total score and non-completion of PE.
| Demographics | Completers | Non-Completers | P-value | |||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Gender | Male | 28 | 80.0 | 17 | 77.3 | 0.25 |
| Race | White | 14 | 40.0 | 5 | 22.7 | 0.09 |
| Black | 20 | 57.1 | 13 | 59.0 | ||
| Other | 1 | 2.9 | 4 | 18.2 | ||
| Combat (yes) | 20 | 57.1 | 13 | 65.0 | 0.78 | |
| Trauma Type | Combat: Vietnam/Korea | 14 | 40.0 | 4 | 18.2 | 0.11 |
| Combat: OEF/OIF/PG | 5 | 17.1 | 9 | 40.9 | ||
| Combat: MST/Sexual | 5 | 14.3 | 5 | 22.7 | ||
| Other | 10 | 28.6 | 4 | 18.2 | ||
| Mean (range) | Mean (range) | |||||
| Age, years | 58.2 ( 25-75) | 50.3 ( 24-77) | 0.05 | |||
| Pre-PHQ score | 16.7 ( 7-26) | 17.0 ( 9-27) | 0.87 | |||
| Pre- PCL5 | 56.0 ( 30-80) | 59.5 ( 45 - 80) | 0.28 | |||
| PTE score | 15.7 ( 0-30) | 15.7 ( 7-26) | 0.97 | |||
| Completers only | ||||||
| # Sessions, median (range) | 10 ( 7-20) | |||||
| Post-PHQ score | 11.6 ( 3-25) | |||||
| PCL5-Post | 37.1 ( 7-75) | |||||
Table 1: Characteristics of study participants.
Of those completing PE therapy, regardless of PTE score, all veterans improved post-treatment with regard to PCL-5 score. Mean pre and post PCL-5 scores were 56.0 (range 30-80) and 37.1 (range 7-75), respectively. When examining PCL-5 scores by total PTE score, mean differences pre/post-PE were 19.0 (p=0.0006), 14.4 (p=0.0002), and 31.1 (p<0.0001) respectively, in the low, middle and high PTE groups (Figure 1). Additionally, in the PTE group with the highest expectations, post PCL-5 scores were the lowest (28.7) compared to either the low (42.7) or middle (37.6) expectation group (p=0.013 and p=0.065, respectively).
Figure 1: Association between PTSD Treatment Expectations (PTE) Total Score and PCL-5 Score Differences Pre/Post PE: PTE1: ‘I believe it is possible to heal from trauma’ PTE2: ‘I believe it is possible to recover from PTSD’, PTE3: ‘I feel confident that I will be successful in my PTSD treatment’. Mean PCL-5 differences pre/post PE presented in boxes. Statistical significance of differences pre/post PE are presented at the bottom of each section.
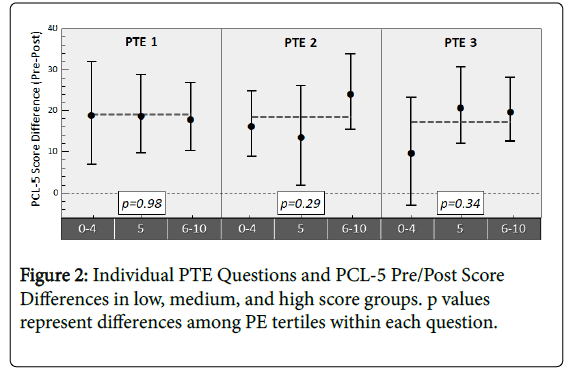
In regards to whether individual PTE questions themselves were predictive of symptom improvement, there were no differences in mean PTSD symptom-score on PCL-5 Pre/Post therapy by individual PTE question (p>0.2 for all). For PTE 2 (‘I believe it is possible to recover from PTSD’) and PTE 3 (‘I feel confident that I will be successful in my PTSD treatment’), there was some indication that higher scores on these questions may translate to larger improvements (range of PCL-5 Pre/Post differences in low, medium, and high expectancy groups were 14.0-24.6 on item 2 and 10.2-21.3 on item 3), but still not statistically significant when looking at these questions on their own. PCL-5 differences Pre/Post PE did not vary by low, medium or high expectations on PTE item 1 (‘I believe it is possible to heal from trauma’) (range 18.4-19.4, Figure 2).
Discussion
Consistent with previous research, [7,15] the current study results suggest that higher outcome expectations are associated with greater therapeutic gains in PE. Given the modest response rates of PE patients in general [3,6], the current study indicates a potentially important factor that contributes to understanding this phenomenon.
Although the pattern of associations between outcome expectancy and reduction of symptoms has previously been shown in the literature, the mediating factors explaining this trend are not yet fully understood [15]. Some possible mediators of this relationship include: better adherence to treatment regimen, greater likelihood of doing assigned homework, and stronger patient-therapist alliance (i.e. a patient with higher outcome expectations may be more likely to engage with the therapist) [15]. Further research is thus needed to fully understand the processes underlying this association.
As described above, unlike PTE items 2 and 3 and PTE total score, PTE item 1 (‘I believe it is possible to heal from trauma’) was not associated with outcome. Examination of the linguistic properties of item 1 versus the other two items may help explain this difference. In PTE item 1 veterans were asked to rate the statement ‘I believe it is possible to heal from trauma,’ whereas items 2 and 3 used the term ‘PTSD’ instead of ‘trauma.’ It is possible that the variation in language – i.e. asking about ‘trauma’ versus ‘PTSD’ – caused each question to capture unique patient attitudes.
Further research is also needed to elucidate how treatment expectancies may or may not be shifted by improving pretreatment patient education and by providing treatment rationales. One study showed that treatment testimonials influenced treatment choice in trauma-exposed treatment-naïve community members who were given a choice between PE and sertraline treatment [16] but it is unclear how treatment rationales or testimonials may change expectancies about a particular treatment, such as PE for PTSD.
Regarding study limitations, our small sample size of veterans may limit generalizability to other populations. Furthermore, only selfreport measures were used which may not give as complete a clinical picture as opposed to combining self-report with clinician-report measures. Lastly, the PTE outcome expectancy measure was used here for the first time, thus further psychometric evaluation is needed.
Conclusion
Our results show that when veterans expect improvement from PE before beginning treatment, they show larger reductions in PTSD symptom severity after treatment than veterans who have lower expectations. These results suggest that it is clinically relevant to assess veterans’ treatment outcome expectancies before PE. The PTE measure provides a concise, low-burden treatment expectancy assessment option for clinicians and patients. Identifying veterans who would most benefit from therapy may allow providers to better choose a therapeutic approach and provide more optimal treatment. Future studies should empirically test outcome expectancy interventions, such as whether patients’ attitudes and concerns about treatment represent appropriate pre-treatment education targets.
Author Note
Hannah C. McLane, Corporal Michael J Crescenz Veterans Affairs Medical Center, Department of Occupational and Environmental Medicine; University of Pennsylvania, Division of Occupational and Environmental Medicine, Department of Emergency Medicine; J. Ben Barnes, Corporal Michael J Crescenz Veterans Affairs Medical Center, Department of Psychiatry; Frances S. Shofer, University of Pennsylvania School of Medicine, Department of Emergency Medicine. Jason T. Goodson, Philadelphia VA Medical Center; University of Pennsylvania, Department of Psychiatry.
Acknowledgement
This research was supported in part by training grants from the National Institute of Occupational Safety and Health grant number:5- TO1-0H008628, and the Health Resources and Services Administration grant number: D33HP25770-01-00. The information and views set out in this study are those of the authors and do not reflect the official opinion of the funding agencies.
Conflict of interest
Authors declare no conflict of interest.
References
- U.S. Department of Veterans Affairs: Epidemiology of PTSD. USA.
- Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA (2016) Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma 8: 107-114.
- Eftekhari A, Ruzek JI, Crowley JJ, Rosen CS, Greenbaum MA, et al. (2013) Effectiveness of national implementation of prolonged exposure therapy in Veterans Affairs care. JAMA Psychiatry 70: 949-955.
- Goodson JT, Helstrom AW, Marino EJ, Smith RV (2017) The impact of service-connected disability and therapist experience on outcomes from prolonged exposure therapy with veterans. Psychol Trauma 9: 647-654.
- Goodson JT, Lefkowitz CM, Helstrom AW, Gawrysiak MJ (2013) Outcomes of Prolonged Exposure therapy for veterans with posttraumatic stress disorder. J Trauma Stress 26: 419-425.
- Jeffreys MD, Reinfeld C, Nair PV, Garcia HA, Mata-Galan E, et al. (2014) Evaluating treatment of posttraumatic stress disorder with cognitive processing therapy and prolonged exposure therapy in a VHA specialty clinic. J Anxiety Disord 28: 108-114.
- Price M, Maples JL, Jovanovic T, Norrholm SD, Heekin M, et al. (2015) An investigation of outcome expectancies as a predictor of treatment response for combat veterans with PTSD: comparison of clinician, self-report, and biological measures. Depress Anxiety 32: 392-399.
- Chambless DL, Tran GQ, Glass CR (1997) Predictors of response to cognitive-behavioral group therapy for social phobia. J Anxiety Disord 11: 221-240
- Brown LA, Wiley JF, Wolitzky-Taylor K, Roy-Byrne P, Sherbourne C, et al. (2014) Changes in self-efficacy and outcome expectancy as predictors of anxiety outcomes from the CALM study. Depress Anxiety 31: 678-689.
- Sotsky SM, Glass DR, Shea MT, Pilkonis PA, Collins JF, et al. (1991) Patient predictors of response to psychotherapy and pharmacotherapy: findings in the NIMH Treatment of Depression Collaborative Research Program. Am J Psychiatry 148: 997-1008
- Borkovec TD, Nau SD (1972) Credibility of analogue therapy rationales. J Behav Ther Exp Psy 3: 257-260.
- Collins JF, Hyer L (1986) Treatment expectancy among psychiatric inpatients. J of Clin Psychol 42: 562-569.
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, et al. (2013) The PTSD Checklist for DSM-5 (PCL-5)-Standard.
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL (2015) The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 28: 489-498.
- Constantino MJ, Arnkoff DB, Glass CR, Ametrano RM, Smith JZ (2011) Expectations. J Clin Psychol 67: 184-192.
- Pruitt LD, Zoellner LA, Feeny NC, Caldwell D, Hanson R (2012) The effects of positive patient testimonials on PTSD treatment choice. Behav Res Ther 50: 805-813.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi