Case Report, J Neurosci Clin Res Vol: 2 Issue: 1
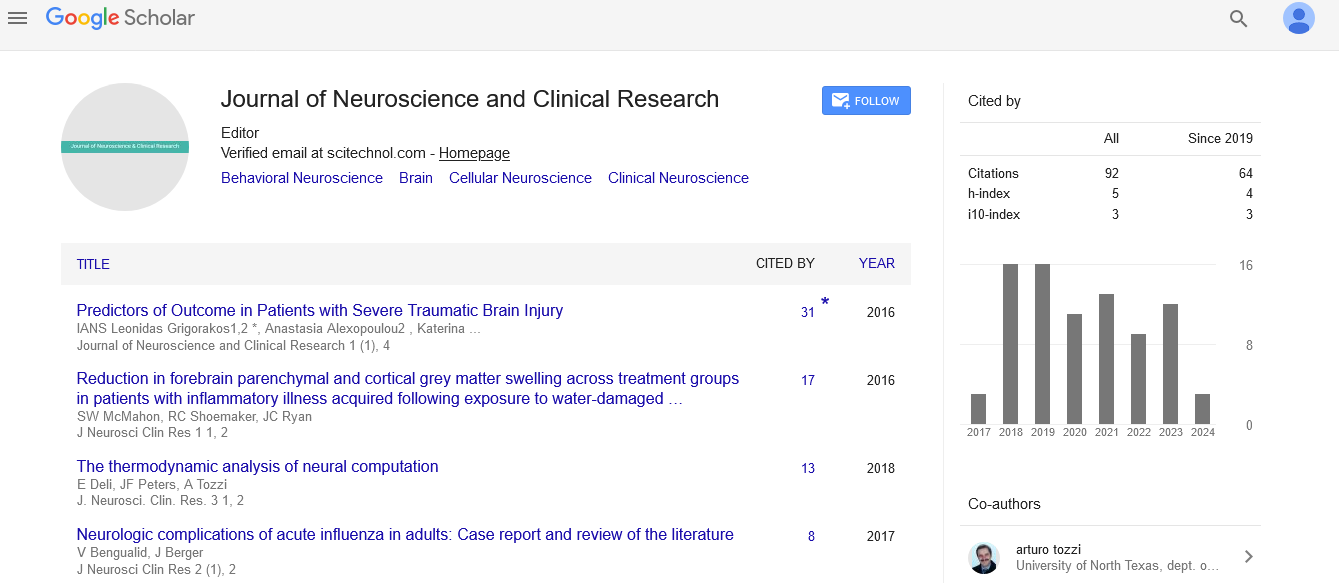
Neurologic Complications of Acute Influenza in Adults: Case Report and Review of the Literature
Victoria Bengualid* and Judith Berger
Department of Internal Medicine, St. Barnabas Hospital, Bronx, NY, USA
*Corresponding author: Dr. Victoria Bengualid
Department of Internal Medicine, St. Barnabas Hospital, 4422 Third Avenue, Bronx, NY,10457, USA
Tel: 718 960-6202
Fax: 718 960-3218
E-mail: vbengualid@sbhny.org
Received date: February 09, 2017 Accepted date: March 15, 2017 Published date: March 21, 2017
Citation: Bengualid V, Berger J (2017) Neurologic Complications of Acute Influenza in Adults: Case Report and Review of the Literature. J Neurosci Clin Res 2:1.
Abstract
We present a case of a 72 year old man with acute onset of confusion secondary to Influenza A. Unlike the pediatric literature, only 21 case reports of neurologic complication during the acute presentation of Influenza were found in adults. The most common presentation was confusion, lethargy or disorientation.
Keywords: Influenza; Neurologic complications
Introduction
Classic symptoms of the “flu” caused by influenza include fever, coryza, body aches, and cough. Central nervous system (CNS) involvement is unusual. Wiley in his review of emerging infections of the CNS describes three conditions that are necessary for the Influenza virus to go beyond its usual pulmonary presentation to causing severe neurologic disorders [1]. The virus must evade its local site of replication and reach the brain. There can occur by direct infection of nerve endings, specifically the olfactory nerve which has nerve endings in the nasal cavity [1]. How this occurs is unclear, and it is not specific for the Influenza virus as it has been described for other viruses such as adenoviruses, parainfluenza viruses, and West Nile Virus. Secondly, the virus has to infect neurons. Influenza virus can bind to neural cells by sialic acid glycosylation or through endocytosis. Once bound to neurons, neuronal proteases can facilitate cell entry, and utilize cellular machinery to replicate [1]. Lastly the virus must survive immune response manifested, in part, by cytokine release. Lee in his review of acute encephalopathy secondary to Influenza note very high levels of cytokines and chemokines in both the blood and cerebral spinal fluid. These high levels seem to correlate with disease severity and neurologic outcome [2].
Genetic factors can also play a role in the ability of Influenza to cause neurologic symptoms. Pandemic strains, as opposed to seasonal influenza, can down regulate the expression of over 30 genes involved in the central nervous system gene network presumably predisposing the host to neurologic complications [3]. In addition mutation of the RANBP2 gene has been described in families presenting with seizures and acute necrotizing encephalopathy (ANE), a known complication of Influenza and Parainfluenza [4]. The RANBP2 gene codes for proteins that help regulate molecules transported through the nuclear pore affecting molecule entry in and out of the nucleus.
Neurologic complications of Influenza have mainly been described in the pediatric population. A surveillance study in Britain from 2011-13 on neurologic complication of Influenza describes 25 cases: 84% in children [5]. The spectrum of neurologic findings runs the gamut from febrile seizures, to somnolence, coma, Rey’s syndrome, and Guillain Barre Syndrome.
We present a case of 72 year old man who presents with sudden onset of confusion and tested positive for Influenza A. We then reviewed the literature to identify other cases of neurologic complications of Influenza in adults (20 years or older) who had an acute presentation of Influenza A or B.
Case Presentation
During the Influenza season of 2016, a 72 year old man was brought to the emergency room for acute onset of confusion. Family reports that he was well during the day helping their children with homework. Then at 5 pm he started to act bizarre. He forgot his daughter’s name and was trying to turn on the TV that was already on. The ambulance arrived at the hospital at 7 pm. He was alert, awake, oriented to self and family but not to time and place. He was tremulous and looked distressed. His speech was incoherent. At triage he was afebrile, blood pressure was 238/100 mmHg, respiratory rate 16 bpm with an O2 saturation of 100% on room air. On physical exam he had some motor weakness on the left upper and lower extremities and a right sided facial droop. A head cat scan (CT) was normal. An abdominal CT scan to rule out aortic dissection was negative. A chest x-ray was negative.
His past medical history was significant for hypertension, hypothyroidism, and renal transplant one year prior to admission (on tacrolimus, mycophenolic acid, and prednisone 5 mg daily), insulin dependent diabetes and glaucoma.
The patient was given nifedipine to control his blood pressure. Twelve hours after his initial presentation he became febrile with temperature of 103°F. He was started with broad spectrum antibiotics. A spinal tap had clear fluid with 2 white blood cells (WBC) and13 red blood cells, protein of 54 and glucose of 150. Culture was negative. Antibiotics were discontinued. Several hours later on physical exam his motor weakness and facial droop resolved but he remained confused, distressed and incoherent. His influenza test became positive for Influenza A. The patient was started with oseltamivir phosphate. He remained confused and had one episode of generalized seizures. An MRI of the brain with contrast was negative. On day 6 of hospitalization his mental status started to improve. He was fluent without any focal neurologic deficits. He completed 7 days of oseltamivir phosphate. He was discharged home without any neurologic deficits.
Review of the Literature
Acute presentation is defined as having influenza-like symptoms (0-5 days) prior to the time of neurologic finding [6]. Cases where neurologic complications occurred after this time frame (sub-acute or post infection complications) represent a different disease entity and are not considered in this review. In addition patients who were co-infected with other pathogens were excluded. This review focused on adult patients (20 years or older). We used PUBMED with the keywords neurologic complications, Influenza, adults, and English. The search yielded 44 entries which were paired down to 17 with the elimination of entries that did not address Influenza infection (19 entries), acute infection (4 cases) or the adult population (4 entries). The remaining articles and their references were reviewed. The search identified 21 cases of adults with acute neurologic complications of influenza.
The 21 cases and our case are summarized in the Table 1. Twenty one of the 22 cases were infected with Influenza A, only one with Influenza B. The age ranged from 20 to 86 years with a mean of 49 years. 73% were under the age of 65 years. Females accounted for only 4 (18%) cases. Underlying medical conditions were specified in 19 cases. Six patients were previously healthy (all under 50 years of age), 3 had underlying liver disease, 3 patients had pulmonary disease, 2 patients were diabetic, 2 patients had hypertension, and one patient each with panhypopituitarism, obesity, and heart disease. Our patient was diabetic and on immunosuppressive therapy for a renal transplant.
| Authors | Age/Gender | Day of illness that neurologic symptoms developed | Symptoms at presentation | CSF | CT/MRI | Diagnosis | Outcome |
|---|---|---|---|---|---|---|---|
| Steininger et al. [5] | 60, M | Not specified. Listed as influenza encephalopathy in distinction to post-influenza encephalopathy | Convulsions, disorientation, somnolence | 203 | Normal | Influenza A Encephalitis |
Recovered |
| Steininger et al. [5] | 78, M | As above | Coma | 9 | Normal | Influenza A Encephalitis |
Died |
| Steininger et al. [5] | 59, M | As above | Coma | 500 | Not done | Influenza A Encephalitis |
Recovered |
| Steininger et al. [5] | 51, M | As above | Coma | 8 | Normal | Influenza A Encephalitis |
Recovered |
| Steininger et al. [5] | 21, M | As above | Disorientation, photophobia, somnolence | Not done | Not done | Influenza A Encephalopathy |
Recovered |
| Wang et al. [6] | 51, M | Several days | Slowed mentation, periods of somnolence during interview but able to follow commands | Not done | Non contrast enhancing lesion in the splenium of the corpus callosum | Influenza A (H3) Encephalopathy |
Recovered |
| Goenka et al. [4] | 26, F | Acute clinical presentation of Influenza | Irritability, intermittent resting tremor right hand, upper limb rigidity | Negative | Normal | Influenza A (H1N1) Acute benign encephalopathy with movement disorder |
Recovered |
| Goenka et al. [4] | 42, M | Acute clinical presentation of Influenza | Headache, bilateral upper limb tremor and rigidity, orofacial bradykinesia | Normal | Normal | Influenza A (H1N1) Encephalopathy with movement disorder |
Poor outcome |
| Ishigami et al. [7] | 35, M | Several days of fatigue and fever | Arrested for cheating and stealing food | Not done | Not Done | Influenza A Encephalitis |
Died the day after arrested. Autopsy: lung, basal ganglia and its capillary vessels stained positive for Influenza A |
| Lee et al. [2] | 76, M | 2 days after fever and cough | Disorientation, incoherent speech, mental dullness | 1 WBC | Normal | Influenza A (H1N1) Encephalopathy |
Recovered |
| Lee et al. [2] | 86, F | 2 days after fever and cough | Delirious, impaired consciousness | 0 WBC | Normal | Influenza A (H3N2) Encephalopathy |
Recovered |
| Lee et al. [2] | 72, M | 4 days after fever and cough | Disorientation, agitation, incoherent speech, involuntary 4-limb tremor | 0 WBC | Normal | Influenza A (h3N2) Encephalopathy |
Recovered |
| Gonzalez et al. [8] | 46, F | 3 days of fever and Influenza-like illness | Confusion, unable to recognize her family | 1 WBC | Normal | Influenza A (H1N1) Encephalopathy |
Recovered |
| Iijima et al. [9] | 27, M | 1 day of fever and flu like symptoms | Seizures, impaired consciousness | 352 WBC | Lesions in the thalami, brain stem and deep white matter | Influenza A (H3N2) Encephalitis Acute necrotizing encephalopathy |
Transferred 3 months later to rehabilitation in a wheelchair |
| Mc.Cray et al. [10] | 4 days of fever and influenza like illness | Confusion, memory loss | 4 WBC | Symmetrical T2 hyperintensities in the temporal lobes, thalami and cingulate cortex | Influenza A Encephalitis Acute necrotizing encephalopathy |
Residual aphasia and memory loss | |
| Akins et al. [11] | 20, M | 5 days fever and influenza like illness | Lethargy, confusion | 53 WBC | Normal. Developed seizures 3 days later, repeat CT diffuse brain edema | Influenza A (H1N1) Encephalitis |
Transferred to rehabilitation 6 weeks later, normal cognition but has generalized rigidity without tremors |
| Ishii et al. [12] | 80, M | 4 days of fever and influenza like illness | Generalized seizures | Not done | Initially normal then had low density areas in the thalamus | Influenza B Seizures Acute necrotizing encephalopathy |
Died |
| Wang et al. [13] | 22, M | 3 days of sore throat cough and fever | Incoherent speech, numbness left upper limb followed by seizures. 10 hours later peripheral paralysis of both sides of his face and sluggish pharyngeal reflex | 0 WBC | Abnormal T2 subcortical white matter basal ganglia and corpus callosum | Influenza A (H1N1) Encephalopathy |
Fully recovered 12 days later |
| Chen et al. [14] | 40, M | 2 days of fevers sore throat diarrhea vomiting and mild headache | Acute onset of violent tremors and clumsiness right side limb that generalized involving all 4 limbs, lips and tongue. Confusion and right hemiplegia developed. 24 hours later shock and respiratory failure | 13 WBC | Hyperintensity over the frontal-parietal areas. Involvement of cortical and subcortical areas but not the deep brain structures | Influenza A (H1N1) Encephalitis/encephalopathy |
Right hemiplegia, left limb rigidity, action tremors, apathy |
| Kahle et al. [15] | 26, F | Febrile, short of breath and confused | Confused Intubated for pneumonia on veno-venous hemofiltration developed a non reactive dilated pupil on hospital day 4 |
Not done | Diffuse cerebral edema | Influenza A (H1N1) Malignant cerebral edema |
Died |
| Kahle et al. [15] | 29, M | Febrile, myalgias, cough headache | Pneumonia, intubated, renal failure, veno-venous hemofiltration. Hospital day 4 developed unreactive pupil | Not done | Cerebral edema | Influenza A (H1N1) Malignant cerebral edema |
Died |
| Current case report | 72, M | Presents with confusion, 12hours later has fever and influenza like symptoms | Confused, tremulous. One episode of seizure | 2 WBC | Negative | Influenza A Encephalopathy |
Recovered |
Table 1: Summary of cases of acute neurologic complications of Influenza in Adults.
The most common presentation was confusion, lethargy, or disorientation. Five cases had a movement disorder, and five had seizures. The final diagnosis was encephalopathy in 8 cases, encephalitis (encephalopathy with a spinal tap with more than 5 WBC) in 7 cases. In three cases the pathology was further defined as ANE (case #14,15,17), two cases with malignant cerebral edema (case #20,21), and one case with reversible splenium involvement (case #6).
Ten patients had a poor outcome. This included all three patients with ANE, and both patients with malignant cerebral edema as well as four of the five patients with seizures and two of the five patients who had a movement disorder or tremors.
CT or MRI findings showed pathology in the corpus callosum, white matter basal ganglia, and one case in the cortical and subcortical regions. The 3 cases with ANE had lesions in the thalami, deep white matter, temporal lobes, and cingulate cortex. However, of the 18 patient who had a scan, 10 (55%) had normal imaging. Two patients had cerebral edema without other findings.
Discussion
Most of the descriptions of neurologic complications of Influenza are in the pediatric literature; however case reports in adults have been reported especially in times of endemic influenza. Complications are seen in all ethnicity, ages, and in people without underlying disease. Our patient was the only case on immunosuppressive therapy. Two other patients had diabetes; three had liver disease: one each with obesity, asthma, and heart disease, all known predisposing factors for Influenza. The remaining 59% were either healthy or without a known risk factor other than age.
Syndromes associated with acute neurologic complication of Influenza include mild encephalopathy with reversible splenial lesions (MERS), encephalopathy associated with malignant brain edema (EMBE) and acute necrotizing encephalopathy (ANE). Hemorrhagic shock and encephalopathy syndrome and acute encephalopathy with seizures and late restricted diffusion are mainly described in the pediatric population.
Most patients in our case review, presented with confusion, lethargy or disorientation. Of those who had a spinal tap, 7 (47%) had an evidence of meningitis. We identified one adult with MERS, two with EMBE, and three with ANE. Patients with EMBE and ANE as well as those who developed seizures or presented with movement disorder tended to have worse outcomes. Twelve patients (55%) fully recovered.
A prospective study of neurologic complications with acute onset of Influenza would help capture the full spectrum of disease. Most likely, case reports underreport mild cases of confusion or other neurologic symptoms that are quickly reversed. During the Influenza season it is very important to be aware that Influenza can cause neurologic findings especially confusion lethargy or disorientation and the threshold to test these patients for Influenza should be low.
References
- Wiley CA, Bhardway N, Ross TM, Bissel SJ (2015) Emerging infections of CNS: Avian influenza A virus, Rift Valley Fever Virus, and Human Parechovirus. Brain Patho25: 634-650.
- Lee N, Wong CK, Chan PKS, Lindegardh N, White NJ, et al. (2010) Acute encephalopathy associated with influenza A infection in adults. Emerging Inf Dis 16: 139-142.
- Ebrahimie E, Nurollah Z, Ebrahimi M, Hemmatzadeh F, Ignjatovic J (2015) Unique ability of pandemic influenza to downregulate the genes involved in neuronal disorders. Mol Biol Rep 201542: 1377-1390.
- Goenka A, Michael BD, Ledger E, Hart IJ, Absoud M, et al. (2014) Neurologic manifestations of Influenza infection in children and adults: results of a national British surveillance study. CID 58: 775-784.
- Steininger C, Popw-Kraupp T, Laferl H, Seiser A, Godl I, et al. (2003) Acute encephalopathy associated with influenza A virus infection. CID 36: 567-574.
- Wang J, Stewart E, Dapph-Afriyie K, Finn A (2015) Mild encephalopathy with reversible splenial lesion in a patient with influenza A infection-first report in an adult patient in the USA. BMJ Case Rep.
- Ishigami A, Kubo S, Ikematsu K, Kitamura O, Tokunaga I, et al. (2004) An adult autopsy case of acute encephalopathy associated with influenza A virus. Leg Med (Tokyo) 6: 252-255.
- Gonzalez BE, Brust DG (2009). Novel Influenza A (H1N1) Presenting as an Acute Febrile Encephalopathy in a Mother and Daughter. CID 49:1966-1967.
- Iijima H, Wakasugi K, Ayabe M, Shoji H, Abe T (2002) A case of adult Influenza A virus-associated encephalitis: magnetic resonance imaging findings. J Neuroimaging 12:273-275.
- Mc Cray B, Forst D, Jundal J, Henderson GV (2015) Clinical reasoning: a 57 year old woman who developed acute amnesia following fever and upper respiratory symptoms. Neurology 84: e102-106.
- Akins PT, Belko J, Uyeki TM, Axelrod Y, Lee KK (2010) H1N1 encephalitis with malignant edema and review of neurologic complications from influenza. Neurocrit Care 13: 396-406.
- Ishii N, Mochizuki H (2015) An autopsy case of elderly-onset acute necrotizing encephalopathy secondary to Influenza. J Neurol Sciences 325: 129-130.
- Wang J, Duan S, Zhao J, Zhang L (2011) Acute disseminated encephalomyelitis associated with influenza A H1N1 infection. Neurol Sci 32: 907-909.
- Chen YC, Lo CP, Chang TP (2010) Novel influenza A (H1N1)-associated encephalopathy/encephalitis A with severe neurological sequelae and unique image features-a case report. J Neurol Sciences 298: 110-113.
- Kahle KT, Walcott BP, Nahed BV, Barnard ZR, Lo EH, et al. (2011) Cerbral edema and a transtentiorial brain herniation syndrome associated with pandemic swine influenza A (H1N1) virus infection. J Clinical Neuroscience18: 1245-1248.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi