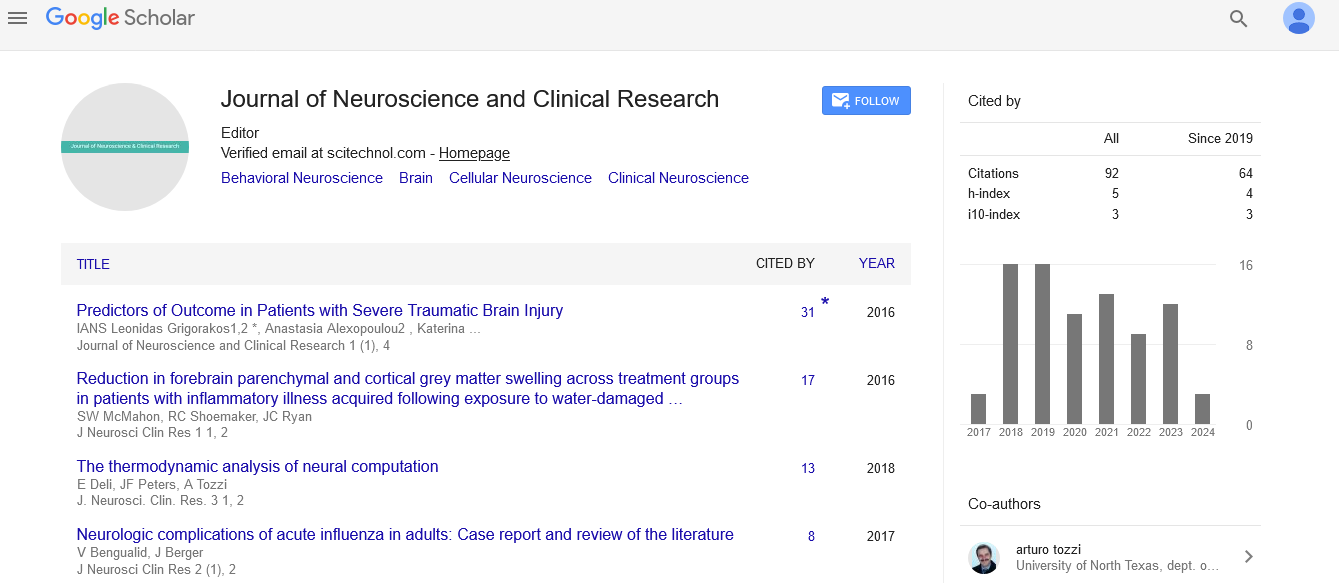
Case Report, J Neurosci Clin Res Vol: 3 Issue: 1
Neuroboriellosis and Associated Myoclonus in a Patient with Kartegener’s Syndrome
Sule Aydin Turkoglu1*, Fatma Sirmatel2, Hayriye Orallar3, Siddika Halicioglu4, Serpil Yildiz1, Erol Ayaz5 and Nebil Yildiz1
1Department of Neurology, Abant Izzet Baysal University Medical Faculty, Bolu, Turkey
2Department of Infectious Diseases Abant Izzet Baysal University Medical Faculty, Bolu, Turkey
3Department of Poultry Science Abant Izzet Baysal University Agriculture and Natural Sciences Faculty, Bolu, Turkey
4Department of Radiology, Abant Izzet Baysal University Medical Faculty, Bolu, Turkey
5Department of Parasitology, Abant Izzet Baysal University Medical Faculty, Bolu, Turkey
*Corresponding Author : Sule Aydin Turkoglu, MD
Department of Neurology, Abant Izzet Baysal University Hospital, 14280, Bolu, Turkey
Tel: +903742534618
Fax: +903742534615
E-mail: suleaydinturkoglu@hotmail.com
Received: November 14, 2016 Accepted: January 02, 2018 Published: January 08, 2018
Citation: Turkoglu SA, Sirmatel F, Orallar H, Halicioglu S, Yildiz S, et al. (2018) Neuroboriellosis and Associated Myoclonus in a Patient with Kartegener’s Syndrome. J Neurosci Clin Res 3:1.
Abstract
Kartegener’s Syndrome is an autosomal recessive disease with primary ciliary dyskinesia. It has a triad of bronchiectasis, dextrocardia or situs inversus and chronic sinusitis. Lyme disease is a multisystem illness. It is referred to as neuroboriellosis if neuropsychiatric involvement is predominant. Myoclonus is a rapid and short hyperkinetic motion disorder. Its secondary etiology is located in the subset of post infectious disease. In this case report we are presenting a female patient of 38 year old known to have Kartegener’s Syndrome who had myoclonic contractions. In the etiological work up, no other finding other than acute infection with Borrelia burgdorferi was found. Lyme disease is a rare etiological factor in involuntary movements, which directed us to prepare this case report.
Keywords: Myoclonus; Lyme disease; Neuroboriellosis; Kartegener’s syndrome
Abbreviations
SEP: Somatosensory Evoked Potential; MRI: Magnetic Resonance Imaging; EEG: Electroencephalography; CT: Computed Tomography; MS: Multiple Sclerosis; ENT: Ear-Nose-Throat; HRCT:High Resolution Computed Tomography
Introduction
Kartegener’s Syndrome is an autosomal recessive disease with primary ciliary dyskinesia. It has a triad with bronchiectasis, dextrocardia or situs inversus and chronic sinusitis [1]. Lyme Disease (LD) is an infectious disease caused by Borrelia burgdorferi. This infectious agent is a spirochete transmitted by tick bites [2]. Being a multisystem disease, LD manifests itself with dermatologic, skeleton-muscular and neuropsychiatric symptoms [3]. Atypical findings can be absent in neuroboriellosis. These are, acute idiopathic polyneuritis, urinary retention, hyponatremia, sensory deficits, visualhallucinations and constipation [4].
Myoclonus is a rapid and short hyperkinetic motion disorder. It is divided into three groups according to etiology; physiological, essential and epileptic. Secondary myoclonus may result from cortical or subcortical disease. Among the secondary reasons, postinfectiousencephalitis belongs to the subset of cortical reasons [5].
In this case report we are presenting a 38 year of female patient known to have Kartegener’s Syndrome who had myoclonic contractions. In the etiological work up no other finding than acute infection with Borrelia burgdorferi was found. Lyme disease is a rare etiological factor in involuntary movements, which directed us toprepare this case report.
Case Report
A 38-year-old woman living in the village working as a farmer, admitted to the outpatient neurology clinic with myoclonic contractions which increased gradually for the last 4 years. She has been followed for Kartegener’s Syndrome (bronchiectasis, situs inversus and chronic sinusitis) for 20 years. Her solid organs located in the abdomen and thorax on the opposite location (Figure 1). She has been followed for Bronchiectasis and pansinusitis by the Clinics of Pulmonary Medicine and ENT. She had immotile cilia and anosmia and she had been treated for Pneumonia caused by Pseudomonas Aeruginosa. In the ultrasound imaging of the abdomen, it was seen that the solid abdominal organs were located on the opposite side.
The patient has been experiencing numbness on the right foot which was relieved by motion, right knee pain and difficulty in standing up for approximately 5 years. She also had stabbing type back pain and pain that was aggravated by deep inspiration. The patient experienced fasciculations in her body, legs and sometimes in her face which was sometimes accompanied by a brief jerk. These involuntary movements happened while she was asleep. She was admitted to a neurology outpatient clinic but no pathological finding was discovered in the EEG. She was prescribed valproic acid for involuntary movements. The patient experienced partial relief. Acute pansinusitis and otitis were the only pathological findings in the cranial CT and MRI (Figure 2). Her treatment was modified with theaddition of levetirasetam and the cessation of valproate.
The patient experienced partial relief with the new treatment as well and for the last year she had 20 daily involuntary movements all through her body. She has been experiencing knee pain andoccasionally fever.
She was admitted to our clinic. Synchronized EEG and videomonitorization was utilized but no epileptiform activity was observed during the myoclonic contractions. Posterior Tibial SEP and median SEP was normally range. Extended routine laboratory workup was done. When the acute phase reactant results were analyzed retrospectively increase in CRP, ESR and WBC values secondary to chronic infection was noticed. Nothing special was noticed in Vasculitis tests, Lupus anticoagulant, ANA, ds-DNA. Her liver function tests were within the normal range. She had normal seruloplasmin levels and she had no Kaiser Flesher Ring in the ocular examination, thus Wilson’s disease was ruled out. For the investigation of LD, Borrelia burgdorferi antigens came out to be Ig M (+) and Ig G (+) in the Elisa and Ig M (+) and Ig G (+) in the Western Blot. She was internalized in the Infectious Disease Clinic. She had no history of tick bite. Ceftriaxone 2×1 gr iv and tetracycline 2x100 mg iv treatment was initiated. Posttreatment 3rd month Borrelia burgdorferi antigen values were Ig M (-), Ig G (++), and the 5th month antigen values were Ig M negative, Ig G positive (+) in the Elisa. No change in the involuntary movements was observed after the antibiotherapy butthe acute phase reactants decreased.
Discussion
Kartegener’s Syndrome is an autosomal recessive disease with primary ciliary dyskinesia. It has a triad with bronchiectasis, dextrocardia or situs inversus and chronic sinusitis [1]. Chronic bacterial infections are common due to accumulating secretions. The most common infectious agents are Haemofilus influenza, Pseudomonas aeruginosa, Streptococcus pneumonia, Moraxella kataralis and Staphylococcus aureus [6]. Our case was followed forPseudomonas aeruginosa in accordance with the literature.
Myoclonus is a rapid and short hyperkinetic motion disorder [5]. It is classified as cortical myoclonus, brain stem myoclonus and spinal myoclonus according to its etiology. In cortical myoclonus abnormal activity starts in the sensory motor cortex and it continues through the spinal cord in the pyramidal tract [7,8]. In propriospinal myoclonus, muscles are activated and the activity is both from up and down. Axial myoclonus consists of flexion of the neck and body, abduction of the arms and flexion of the hips. It could be caused from the spinal cord or the brain stem. Spinal trauma, infection, tumor and disc herniation were defined in its etiology [9]. Brain stem reticular myoclonus is the most important reason of axial myoclonus. The myoclonic activity starts from the lower brain stem and spreads tothe higher brain stem and the spinal cord. There is no relation with the cortex. Anoxic encephalopathy, posttraumatic encephalopathy,sarcoidosis, viral encephalomyelitis, MS and paraneoplastic reasonsare the causes among the many etiological factors [10-14]. InHastam�?±zda yap�?±lan video EEG, the posterior Tibial SEP and medianSEP responses was not considered because it has not detected specialcaracter myoclonus for özellik saptanmamas�?± nedeniyle kortikalmiyoklonus dü�?�?ünülmemi�?�?tir Cortical myoclonus was ruled outas no pathological finding was found in the video EEG in PosteriorTibial SEP and median SEP response . Our patient had head andneck flexion type jerks which was more prominent on the left upperextremity. The jerks were abduction in the arms and flexion in thelegs. They were consistent with axial myoclonus especially brain stemreticular myoclonus. As the patient did not have history of trauma,tumor or anoxia infectious etiology was considered to be the reason.In the infectious disease workup acute neuroboriellosis infection wasfound. Neuroboriellosis causes lymphocytic meningo-radiculopathyafter 4-6 weeks of inoculation. This causes painful sensory complaintsand motor radiculoneuritis [15,16]. Limited number of cases withproprioceptive myoclonus and LD were reported in the literature[17,18].
Chronic pain and arthralgia are commonly seen together in Lyme disease [19,20]. The patient had extensive muscle and joint pain for 1-2 years which was in conjunction with the literature. Our case had increased ESR and CRP values. According to the literature increase in ESR and CRP could be seen in LD [21,22]. Since the patient has been followed for Kartegener’s Syndrome with chronic sinusitis, bronchiectasis and immotile cilia the rise in the infectious markers could be secondary to chronic infection or Lyme disease. After treatment for Lyme Disease the acute phase reactants decreased. The chronic joint and stabbing back pain that the patient experienced for 4-5 years were ignored and linked with her chronic condition. According to the literature in some elderly patients who admitted with the symptoms of Polymyalgia romatica and increase in ESR and CRP values; Lyme disease is discovered [23]. In cases with ESR and CRP increase and extensive muscle and joint pain as the initial symptoms who have other chronic conditions differential diagnosis could be quite challenging and establishing definitive diagnosis could be delayed. We think the diagnosis was delayed from the same reasonin our patient.
Conclusion
In conclusion, in patients presenting with atypical symptomslike progressive myoclonic jerks, extensive muscle and joint pain infectious and treatable etiologies like LD could be thought in thedifferential diagnosis.
Informed Consent
Written informed consent was obtained from patient whoparticipated in this study.
References
- Bush A, Chodhari R, Collins N, Copeland F, Hall P, et al. (2007) Primary ciliary dyskinesia: current state of the art. Arch Dis Child 92: 1136-1140.
- Steere AC, Grodzicki RL, Kornblatt AN, Craft JE, Barbour AG, et al. (1983) The spirochetal etiology of Lyme disease. N Engl J Med 308: 733-740.
- Bransfield RC (2001) The Neuropsychiatric Assessment of Lyme Disease. 14th International Scientific Conference on Lyme Disease and Other Tick-Borne Disorder 21-23.
- Shamim EA, Shamim SA, Liss G, Nylen E, Pincus JH, et al. (2005) Constipation heralding neuroborreliosis: an atypical tale of 2 patients. Arch Neurol 62: 671-673.
- Espay AJ, Chen R (2013) Myoclonus. Continuum (Minneap Minn) 19: 1264-1286.
- Alanin MC, Nielsen KG, von Buchwald C, Skov M, Aanaes K, et al. (2015) A longitudinal study of lung bacterial pathogens in patients with primary ciliary dyskinesia. Clin Microbiol Infect 21: 1093.e1-1093.e7.
- Caviness JN (2009) Pathophysiology and treatment of myoclonus. Neurol Clin 27: 757-777, vii.
- Shibasaki H, Hallett M (2005) Electrophysiological studies of myoclonus. Muscle Nerve 31: 157-174.
- Capelle HH, Wöhrle JC, Weigel R, Grips E, Bäzner HJ, et al. (2005) Propriospinal myoclonus due to cervical disc herniation. Case report. J Neurosurg Spine 2: 608-611.
- Kojovic M, Cordivari C, Bhatia K (2011) Myoclonic disorders: a practical approach for diagnosis and treatment. Ther Adv Neurol Disord 4: 47-62.
- van der Salm SM, Erro R, Cordivari C, Edwards MJ, Koelman JH, et al. (2014) Propriospinal myoclonus: clinical reappraisal and review of literature. Neurology 83: 1862-1870.
- Li JY, Cunic DI, Paradiso G, Gunraj C, Pal PK, et al. (2008) Electrophysiological features of myoclonus-dystonia. Mov Disord 23: 2055-2061.
- Brown P, Thompson PD, Rothwell JC, DayBL, Marsden CD (1991) Paroxysmal axial spasmsof spinal origin. Mov Disord 6: 43-48.
- Brown P, Thompson PD, Rothwell JC, Day BL, Marsden CD (1991) Axial myoclonus of propriospinal origin. Brain 114 : 197-214.
- Hansen K, Crone C, Kristoferitsch W (2013) Lyme neuroborreliosis. Handb Clin Neurol 115: 559-575.
- Kaiser R (1998) Neuroborreliosis. J Neurol 245: 247-255.
- de la Sayette V, Schaeffer S, Queruel C, Bertran F, Defer G, et al. (1996) Lyme neuroborreliosis presenting with propriospinal myoclonus. J Neurol Neurosurg Psychiatry 61: 420.
- Schoof J, Kluge C, Heinze HJ, Galazky I (2013) Startle myoclonus induced by Lyme neuroborreliosis: a case report. J Med Case Rep 7: 124.
- Zimering JH, Williams MR, Eiras ME, Fallon BA, Logigian EL, et al. (2014) Acute and chronic pain associated with Lyme borreliosis: clinical characteristics and pathophysiologic mechanisms. Pain 155: 1435-1438.
- Garakani A, Mitton AG (2015) New-onset panic, depression with suicidal thoughts, and somatic symptoms in a patient with a history of lyme disease. Case Rep Psychiatry 2015: 457947.
- Mauch E, Vogel P, Kornhuber HH, Hahnel A (1990) Clinical value of antibody titers to Borrelia burgdorferi and titer course in neurologic disease pictures. Nervenarzt 61: 98-104.
- Hirose K, Wener MH, Duckert LG (1999) Utility of laboratory testing in autoimmune inner ear disease. Laryngoscope 109: 1749-1754.
- Paparone PW (1995) Polymyalgia rheumatica or Lyme disease? How to avoid misdiagnosis in older patients. Postgrad Med 97: 161-164, 167-170.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi