Review Article, J Clin Genom Vol: 1 Issue: 1
Move Toward to Non Invasive Mechanical Ventilation in Amyotrophic Lateral Sclerosis: A Clinical Review
Solimando AG1*, Ciccol S1, Di Lernia G1, Leonel P1, D’Errico E2, Schneider A3, Fritz G4, Brienza N5, Racanelli V1 and Vacca A1
1Department of Biomedical Sciences and Human Oncology, Section of Internal Medicine “G. Baccelli”, University of Bari Medical School, Bari, Italy
2Department of Basic Medical Sciences, Neurosciences and Sense Organs, University of Bari “Aldo Moro”, Bari, Italy
3Department of Internal Medicine I, Emergency Medicine and Intensive Care, University Medical Center Würzburg, Germany
4Department of Intensive Care and Anesthesiology, Heart Center Brandenburg, Bernau, Germany
5Anaesthesia and Intensive Care Unit, Department of Emergency and Organ Transplantation, University of Bari, Policlinico, Bari, Italy
*Corresponding Author : Antonio Giovanni Solimando
Department of Biomedical Sciences and Human Oncology, Section of Internal Medicine “G.Baccelli”, University of Bari Medical School, Policlinico, Piazza GiulioCesare 11, Italy
Tel: +393395626475
E-mail: antonio.solimando@uniba.it
Received: November 29, 2017 Accepted: January 04, 2018 Published: January 10, 2018
Citation: Solimando AG, Ciccol S, Di Lernia G, Leonel P, D’Errico E, et al. (2018) Move Toward to Non Invasive Mechanical Ventilation in Amyotrophic Lateral Sclerosis: A Clinical Review. J Clin Genom. 1:1.
Abstract
Subjects with amyotrophic lateral sclerosis (ALS) can have fast or slow evolution. Precocious diagnosis significantly impacts on natural history, even though the prognosis remains severe, indeed the mortality rate at 5 years is higher than 80%. Progressive weakness of bulbar, limb, and respiratory muscles is characteristic. Death generally occurs from 2 to 4 years following symptom onset, primarily owing to respiratory failure. Treatments for respiratory aspects of ALS are evolving. This manuscript that recapitulates the current indications is aimed to define a rational basis for a patientoriented approach to treatment of ALS, mainly focused on noninvasive mechanical ventilation (NIV).
Keywords: Amyotrophic Lateral Sclerosis; Mechanical ventilation; Hypercapnia
Introduction
The correct diagnosis and clinical management of patients suffering from Amyotrophic lateral sclerosis (ALS) remains an important challenge in this field. The ALS onset occurs usually in middle aged patients and the disease leads to death after 3-5 years. In most epidemiologic reports there is an incidence of 1-3 cases/ 100000 / year and a prevalence of 3-5 / 100,000. The clinical scenario of presentation is unpredictable, depending on the predominant initial involvement of the upper or lower motor neurons [1,2].
Common starting symptoms include hyposthenia, hypotrophy, stiffness, cramping and collision of the muscles of the hands and arms (often seen at the level of the intrinsic muscles of the hand). Lower limbs (stiffness, cramps, and hyposthenia) are less severe than the ones in upper limbs. Symptoms of cerebral trunk include dysphagia, which can lead to aspiration pneumonia and impairment of energy supply; the tongue can undergo a pronounced atrophy, which causes difficulty in the word articulation (dysarthria), phonation and swallowing [1,3].
Hypersensitivity to respiratory muscles leads to respiratory failure. Other characteristic features of ALS are the absence of sensitive abnormalities, pseudobulbar paralysis (with lax and involuntary tears) and the absence of intestinal or bladder dysfunction. Dementia is not a component of sporadic ALS. In some families ALS is inherited along with a frontotemporal dementia, characterized by secondary behavioural alterations to frontal lobe dysfunctions [1]. Precocious diagnosis has a significant impact on natural history, even if the prognosis remains severe, in fact the mortality rate at 5 years is higher than 80% [3].
Progressive weakness of bulbar, limb, and respiratory muscles is characteristic. Death generally occurs from 2 to 4 years following symptom onset, primarily owing to respiratory failure. Only 20% of patients live more than 5 years. The disease mostly appears at 43-52 years of age if it is familiar, otherwise at 58-63 years for the sporadic cases [4]. Regrettably, if the skeletal muscles are implicated, the respiratory apparatus could determine a rapid respiratory degeneration. This may because a decrease in general condition and a higher risk of aspiration pneumonia due to dysphagia, an exaggerated modification in the response to muscle relaxants, and, among other adverse side effects, a delayed recovery of spontaneous breathing after general anesthesia [5]. Consequently, anesthetic approach in ALS should include cautious monitoring and proper drug choice, in order to avoid severe complications [5]. This review is aimed to update on the new therapeutic landscape for pulmonary aspects of ALS which is still an unachieved medical goal.
Pathophysiology of ALS
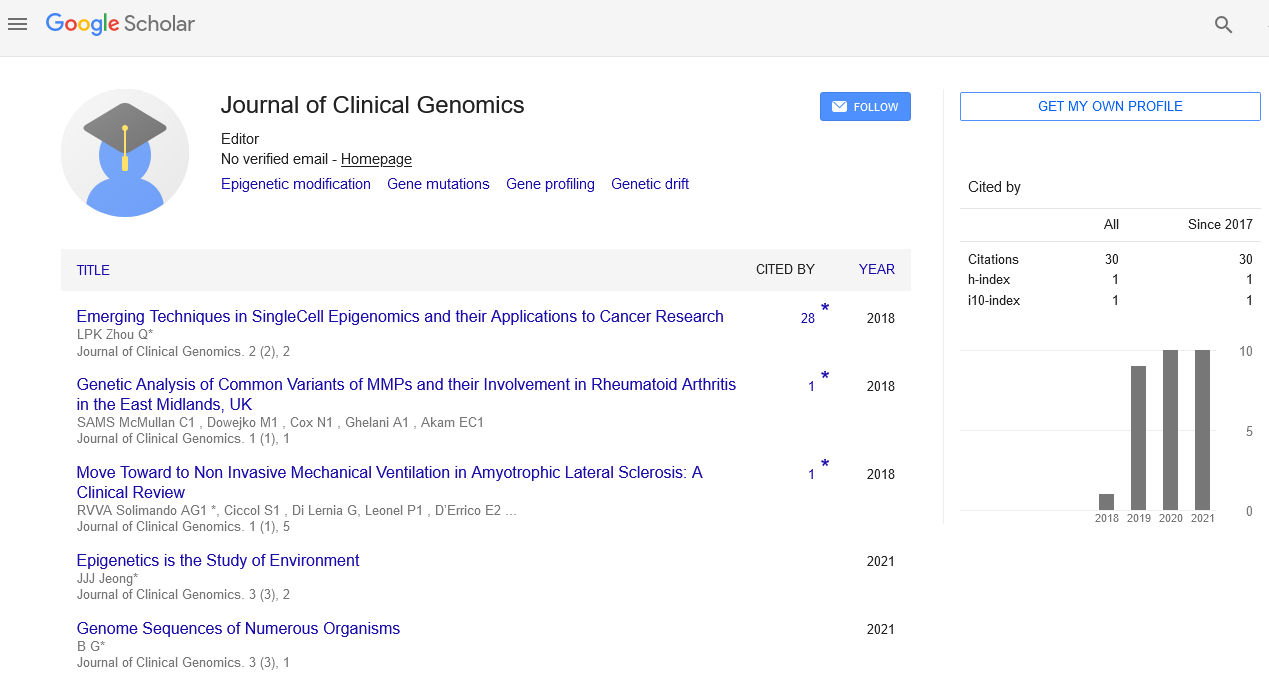
If on one side ALS lacks predictable biomarkers, on the other side one common guideline to a correct diagnosis of the disease is missing. We are still far away from the identification of a single gene responsible for disease progression, even though the latest findings revealed a pattern of genes involved in the same manner [5]. The identified pattern of genes seems to share some cellular functions such as RNA metabolism, protein degradation, ER-Golgi pathway, trafficking and endosomal sorting complexes required for transport. Guerriero R. et al. have drawn up a complete table with all the genes involved in ALS and Frontotemporal dementia and the possible pathways connected. Regarding ALS the most reliable genes are TAR DNA Binging protein (TARBDP) and FUS RNas Binding protein; they both confirm the involvement of DNA/RNA metabolism [6]. Unfortunately, their specific role and how their dysfunction regulates ALS development are still unknown. Also protein accumulation seems to affect the disease progression. It has been shown that the accumulation of filaments of ubiquitinated material on motor neurons is associated with ALS [7]. The evidences that characterize the mechanism behind these accumulations is still scanty. Nevertheless, the disease progression with the increasing instability of the genome, seem to be responsible for the production of material aggregates destined for degradation [8,9]. In this scenario, it is worth highlighting even the possible involvement of autophagy deregulation as a cause of the disease [10,11]. Research in this field is growing very fast due to the role of autophagy in the elimination of cellular damaged components and the evidence that neurodegenerative diseases are connected with accumulation of material that has not been wasted. In ALS it seems that autophagy is enhanced by an accumulation of LC3-II protein in mouse models for the disease [12,13]. Notwithstanding the promising hypothesis and the early evidence in animal models, still there are no therapeutic results regarding autophagy-modulation drugs [2] (Figure 1).
Figure 1: The ALS disease biology. A multifaceted interaction between genetic factors and molecular pathways has a pivotal role. Mutations in DNA/ RNA-regulating genes including the recently reported c9orf72 (chromosome 9 open reading frame 72) gene, suggesting an important role for dysfunction of RNA metabolism in ALS pathogenesis. Further, dysfunction of molecular pathways, including glutamate-mediated excitotoxicity, has been identified in sporadic and familial ALS, indicating the existence of a common pathogenic pathway.
Clinical remarks
Subjects with ALS can have rapid or slow evolution. Symptoms could be muscular weakness, loss of coordination, spasticity, atrophy, fasciculation and hyperreflexia that lead to a progressive degeneration of motor neurons. In this scenario the patient could develop a progressive asymmetric limb weakness and bulbar manifestations such as difficulty in speaking (dysarthria), problems in swallowing (dysphagia) and in some cases problems related to respiratory muscle with consequent difficulty in breathing [14,15]. The distinctive anatomy-pathological characteristic of the ALS is the death of both lower motor neurons (spinal cord horn cortex cells and their counterparts in the cerebral trunk that innervate the bulbar muscle), as well as upper or corticospinal motoneurons (which originate in the fifth layer of the cortex motor and descend through the pyramidal beam to contract synapse with the lower motoneurons). Although initiating ALS may cause a selective loss of only lower motor carcasses or only upper motor neurons, it ultimately results in a progressive loss of both types [1]. The absence of a clear involvement of both motor neurotic populations must lead to questioning the possible diagnosis of ALSs. Liquor is usually normal. Muscle enzymes (e.g. CK) can be elevated. Many types of secondary motor neurone disorders, similar to ALS, are curable [2,3].
MRN or myelo-CT is often necessary to exclude compression lesions of the forearm magna or cervical column. When only inferior motoneurons are affected, another important clinical issue to consider is motor multifocal neuropathy with conduction block. ALS-like lower axonal motor neuropathy sometimes can be associated with hematopoietic disorders such as lymphomas or multiple myeloma; the presence of a serum monoclonal component should bring to a rapid execution of a bone marrow biopsy. Lyme disease can also cause axonal lower motor neuropathy, typically with intense proximal limbs in the limbs and pleural effusion. Other benign conditions that rarely imitate ALS are chronic lead poisoning and thyrotoxicosis [3].
Pulmonary evaluation in ALS
Premature decline of the respiratory components (muscles and neuromuscular degeneration) may determine death before the disease involves additional sites [16]. A mask based evaluation can be used to obtain measures (as indicated in bulbar ALS) that are fundamental to motivate non invasive mechanical ventilation (NIV) [17]. Nonetheless, frequent intensive monitoring and following up adjustments when necessary, are a valuable choice in a multidisciplinary clinic field [18]. Certainly providing extensive and detailed education, selecting the interface carefully, and controlling sialorrhea, are fundamental topics [19]. However, the role of early NIV is debated [3,20,21]. It is worthwhile to plan the ventilation program in a patient oriented manner. Therefore the appropriate strategy to initiate ventilation has to be discussed well in advance. Ventilation capacity (FVC), mean inspiratory pressure (MIP), and expiratory CO2 level (ETCO2) are fundamental parameters to take into account in order to better plan the neurologic approach.
Clinical studies evidences
Long-term mechanical ventilation is exceptionally used [22]. Nevertheless this approach can considerably boost life expectancy. Remarkably, most patients cannot be weaned from ventilator support [23]. Early decision making should include thorough documentation of discussions [24]. Studies demonstrate patients’ preference for physician to initiate the discussion [22-25]. Diaphragm pacing option demonstrated conflicting results [26]. Three studies were halted for increased mortality in treatment arm [26-28]. A meta-analysis from all studies examine reasons for disparities and attempt to identify subgroups of patients who may benefit [29]. Death in ALS is in most of the cases linked to the respiratory function: people die because of respiratory failure. An intervention that could impact respiratory function would be incredibly important in ALS, which raises the stakes in terms of effectively measuring respiratory capacity [30]. The most commonly used measure in clinical trials is the vital capacity VC, however there is a difference between the experimental and clinical way used to measure VC [31].
Respiratory function tests can be useful for ventilation management. The swallowing assessment allows the identification of patients at risk of aspiration. A genetic test is available for the mutations of superoxide dismutase 1 (SOD1) responsible for 20% of the family forms of ALS, as well as for rare mutations of other genes [32].
There is no treatment that blocks the basic pathological process of ALS. Riluzole produces a modest elongation of survival; in a study, 18-month survival in riluzole (100 mg / day) subjects was similar to the one in15-month-placebo-treated patient. Its mechanism of action very likely decreases the release of glutamate thus reducing the excitotoxic death of neuronal cells. Riluzole toxicity profile can comprise weight loss, dizziness, nausea, and liver toxicity [33].
Currently, several therapeutic agents for ALS are being studied in clinical trials, including ceftriaxone, pramipexole and tamoxifen. Interventions such as the use of antisense oligonucleotides, which are able to reduce the expression of the mutant SOD 1 protein, are currently undergoing clinical trials on ALS cases associated with mutated forms of SOD1 [32,34]. Several rehabilitative aids can substantially help ALS sufferers. Showers to prevent foot falls make walking easier, while the ones suitable for the extension of patients’ fingers strengthen their grip.
In the cases with bulbar involvement, normal chewing and swallowing can be affected and gastrostomy may be useful in restoring normal nutrition and hydration. Voice synthesizers increase the chances of speaking in the advanced stages of bulbar paralysis. Respiratory care can ensure survival. For patients who choose to avoid long-term ventilation through tracheostomy, positive pressure ventilation through the nose or mouth provides transient relief (a few weeks) from hypercapnia and hypoxia. Respiratory devices that cause artificial cough are also useful: they help release the respiratory tract and prevent pneumonia from aspiration [35,36]. The variability in the clinical approach to the patient with ALS highlights the lack of guidelines in the long-term integrated approach [37]. The available data suggest that the early use of non –invasive ventilation (NIV) can change clinical outcome and improve quality of life [38].
Discussion and Outlook
In ALS respiratory failure is the most important co-morbidity affliction in patient survival. A useful tool in this setting is ventilation. It could be managed both in invasive (using tracheostomy ventilation - TV) and in NIV manner. In ALS patient management more intensive treatments, such as a feeding gastrostomy or TV, are associated with numerous side effects both in early and late stage of the disease. Also NIV entails many problems and does not ensure a later use of TV; therefore physicians should ask themselves if the decision to treat is reasonable and when to perform the treatment [37]. Respiratory failure is often related to hospitalizations, with more frequent bulbar onset [39]. Actually in those who were hospitalized the use of TV larger than in NIV, mainly in the cases with spinal onset. Respiratory failure and pneumonia (both infective and aspiration) are the most common cause of emergency and death [39]. It takes time to discuss the different therapeutic approaches with the patient but if respiratory failure occurs and hypercapnia confusion arises, patients could not be able to provide adequate informed consent for treatment [37].
The sooner a closely monitored disease progression and respiratory function are set the better in order to provide an adequate follow-up and to estimate the risk of decompensating. A FVC less than 50% and/or symptoms of hypoventilation are signals suggesting a respiratory failure: physicians have to prompt a discussion on therapeutic options allowing patients, their families and care-givers to have enough time for a constructive discussion avoiding hasty decisions in a life-threatening emergency setting [3].
TV is the most effective choice for life-long survival but it also results in an intensive resource utilization, an increase in ventilator entrapment risk and finally in an emotionally difficult acceptance, in fact; despite a very high increase in life survival [40,41]. TV enhances disability and dependency, consequently decreasing the quality of life. On the contrary NIV does not affect significantly the use of facial, nasal or mouthpiece tools which are therefore more useful and manageable. Via these different types of masks NIV system provides a ventilator-assisted support using a volume cycled or a bilevel pressure volume ensuring an intermittent positive pressure to support patient ventilation.
A few trials have tried to understand which is the best ventilation to be used in ALS patients. One of them showed an increase in median survival associated to a better quality of life [42,43]. The above result was mostly due to a benefit in a patient with mild-to-moderate bulbar impairment but, notably, in the standard treatment group, 67% of patients died within two weeks after randomization which prompted an accurate appraisal of the presumably overrated positive effect of NIV. Moreover authors had found an improvement in sleep-related symptoms but not in life survival in patients with severe respiratory dysfunction. In another double-blind single-center trail, patients were randomized to NIV use or placebo [44]. The majority of patients in both groups reported no and only mild problems with NIV treatment. The most common complaints were about dry eyes, nose, or mouth and facial discomfort. Authors described that an increase in FVC% after one month of NIV treatment was found compared to placebo but this result did not involve a difference in survival between the two groups. This could be due to the mild ALS dysfunction (evaluated by the specific score) of the patients and because the study was not based on clinical outcomes.
Some authors have also suggested the possibility of using NIV to prevent respiratory failure. In fact, according to Bourke results, a non-randomized study described a decrease in FVC decline and an increase in survival in ALS patients if NIV was used at an earlier stage in disease progression [45]. Some RCT are ongoing to explore the impact of early NIV use in mild respiratory failure ALS patients but exhaustive results are not available yet. Some retrospective series have explored the outcome of ALS patients receiving NIV, finding that most of those who experience this type of ventilator support need a TV after one month of NIV [46,47].
In a French retrospective cohort study researchers found that NIV was mostly used in late stages of disease when severe respiratory symptoms (orthopnea, respiratory-related nocturnal symptoms and hypercapnia) are present [48]. This management is mostly due to the adherence of the prescribers to the French guidelines and to a not strictly surveillance of respiratory function. However in this study authors had also found that in the 90% of patients NIV was not performed in case of acute respiratory distress. In particular they had found that NIV was initiated when a decreased FVC or other parameters such as the presence of daytime or nocturnal symptoms, daytime hypercapnia, decreased maximal inspiratory pressures (Pimax and SNIP), isolated nocturnal desaturations, and polysomnography results occurred. Even the definition of volume needed to perform adequate ventilation is still on debate. In fact many authors suggest low tidal volume ventilation in this particular setting. A more accurate evaluation needs to be performed on both inspired and E-spired volume to avoid a lung dysfunction in particular in patients with a sufficient muscular strength. Maintaining an optimal tidal volume has to be the aim of the use of ventilation. In this prospective it has to be used NIV with a volume-assured pressure support via a pressure-cycled mode (VAPS). In fact, another retrospective single-center cross-sectional cohort study making a comparison between VAPS and a pressure support (PS) had shown that an higher tidal volume was achieved with VAPS [49]. Additionally it has to be stressed that the same authors have described a decreased spontaneous breath cycling not related to the type of ventilation, even if the triggering is less severely impaired in the main percentage of patients under scrutiny [49].
In a retrospective study on ALS patients receiving either NIV or TV authors try to identify the best volume to use [50]. They found that only in the patients who performed TV and not in those with NIV there was a significant positive correlation between body weight (both actual and predicted) and volume both in tidal and minute volume inspired. On the contrary no difference was found in Positive Inspired Pressure (PIP) used for both the groups. It could be noted that PIP appears to be a relatively constant and important parameter when compared to tidal volume and it is not related to severity of bulbar dysfunction in initial NIV treatment or shifting to TV. Moreover in order to ensure an adequate ventilation volume it is essential to take into account the body weight. Body weight is also a clue to acceptance of ventilation particularly in outpatients. It has been highlighted that low body weight and female sex as well as spinal onset imply a lower tolerance to NIV use [51].
Clinical judgment directed approach
One of the most important debates is centered on the best timing for NIV initiation. Many evidences suggest that an earlier initiation of NIV ensures a change in the course of the disease based on a favorable effect on the rate of lung function decline. On the contrary the present guidelines allow physicians to start NIV in only 21% of patients with ALS and only if they qualify for it [52]. Many efforts have been made to access to the best way to drive respiratory management in ALS. A Revised Amyotrophic Lateral Sclerosis Functional Rating Scale score, (ALSFRS-R) has also been proposed to be used in order to identify the possible risk population. This score is not only referred to respiratory functional description but it also explores twelve working items [53]. However even if it may be useful in patient stratification it varies from time to time also with the same patient [54].
Before starting NIV it is necessary an accurate evaluation of pulmonary function. A lung capacity prediction in ALS and functional vital capacity (FVC) measured in an erect posture are the most frequently used procedures. In fact baseline FVC has been found as a predictor of survival in several studies on ALS and it was confirmed in a 20-year cohort study: FVC reduction impacts as a negative prognostic indicator. On the other hand, supine measurement of FVC could be an important marker because the imitation of the sleeping position provides information about diaphragm functionality. Starting NIV in patients performing a FVC shows that about 65% obtains a oneyear survival increase compared to those who start NIV later. After NIV treatment was settled, the rate of FVC reduction was statistically significantly lower than in patients without NIV [52].
Several symptoms described in ALS patients (i.e. excessive daytime sleepiness, morning headache and orthopnea) are a consequence of sleep disturbances associated to nocturnal desaturation. Nocturnal respiratory functions in ALS are more sensitive measurements of FVC. In particular maximal inspiratory pressure (MIP) is a more sensitive indicator of respiratory decline compared to FVC, while Sniff nasal inspiratory pressure (SNIP) measurement has been shown to be more sensitive than MIP and FVC in predicting hypercapnia in ALS patients also when there is no significant bulbar involvement. SNIP should be considered as a marker of diaphragm muscular fatigue, in particular when there has been found a measurement of 40 cmH2O which is related to nocturnal hypoxemia [55].
An RCT meant to study evaluate if polysomnography could be useful to guide the NIV treatment is still ongoing [51].
Performing a full polysomnography (PSG) is much more effective than measuring sleep quality subjectively, Nocturnal desaturation and apnea/hypopnea index are useful parameters to decide when to start NIV [52].
However in clinical practice most of the neurologists base their decision on nocturnal hypoxemia but only 39% perform also a FVC and just 13% use SNIP [56]. Abnormalities in respiratory functional tests (such as a supine drop in FVC, a reduced SNIP, or prolonged nocturnal desaturation) are considered a red mark for initiation of NIV in less than 10% of cases [48]. SNIP is a good tool to quantify the decline in respiratory function. In a retrospective study it has been found that SNIF declined to the utmost in the three months before NIV treatment compared to FVC or inspiratory/expiratory pressure [57].
Another parameter which appears to be effective in decision making is Peak cough flow (PCF) which estimates the efficacy in cough and airway clearance. PCF is measured by performing a maximal inspiration, followed by a cough as forcefully as possible, while the lips are sealed tightly around the tube. It results lower in those who start a NIV treatment compared to those who have not yet had indication to NIV [57]. In other retrospective studies the evaluation described was done on arterial blood gas (ABG) analysis to drive the NIV: even though no significant differences have been found in arterial gas mean values, bicarbonate >30 mg/dL, PCO2 >50 mmHg and pH <7.30 were associated with an increased death risk [46,47]. In ALS patients a delay in initiation of NIV treatment mostly results negative because a poor surveillance of pulmonary function has been performed. The main difficulties are related to patient’s mobilization as well as technical difficulties to perform respiratory tests. A standardized method to study, follow and screen ALS respiratory function is needed to avoid the difficulty to decide when to start NIV. In the retrospective study on the French registry authors had analyzed the importance of guideline use for NIV treatment in ALS patients [48]. After the guideline acceptance they described a less frequent indication to NIV for daytime hypercapnia while a larger number of patients had a poor quality sleep related symptoms associated to a decreased ALSFRS-R score, suggesting a trend to an earlier initiation of ventilation.
References
- Kiernan MC, Vucic S, Cheah BC, Turner MR, Eisen A, et al. (2011) Amyotrophic lateral sclerosis. Lancet 377: 942-955.
- Vucic S, Rothstein JD, Kiernan MC (2014) Advances in treating amyotrophic lateral sclerosis: insights from pathophysiological studies. Trends Neurosci 37: 433-442.
- Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, et al. (2012) EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS)--revised report of an EFNS task force. Eur J Neurol 19: 360-375.
- Haverkamp LJ, Appel V, Appel SH (1995) Natu,ral history of amyotrophic lateral sclerosis in a database population. Validation of a scoring system and a model for survival prediction. Brain 118: 707-719.
- Iguchi Y, Katsuno M, Ikenaka K, Ishigaki S, Sobue G, et al. (2013) Amyotrophic lateral sclerosis: an update on recent genetic insights. J Neurol 260: 2917-2927.
- Guerreiro R, Bras J, Hardy J (2015) SnapShot: Genetics of ALS and FTD. Cell 160: 798
- Leigh PN, Anderton BH, Dodson A, Gallo JM, Swash M, et al. (1988) Ubiquitin deposits in anterior horn cells in motor neurone disease. Neurosci Lett 93: 197-203.
- Majcher V, Goode A, James V, Layfield R (2015) Autophagy receptor defects and ALS-FTLD. Mol Cell Neurosci 66: 43-52.
- Barmada SJ, Serio A, Arjun A, Bilican B, Daub A, et al. (2014) Autophagy induction enhances TDP43 turnover and survival in neuronal ALS models. Nat Chem Biol 10: 677-685.
- Navone F, Genevini P, Borgese N (2015) Autophagy and Neurodegeneration: Insights from a Cultured Cell Model of ALS. Cells 4: 354-386.
- Ghavami S, Shojaei S, Yeganeh B, Ande SR, Jangamreddy JR, et al. (2014) Autophagy and apoptosis dysfunction in neurodegenerative disorders. Prog Neurobiol 112: 24-49.
- Morimoto N, Nagai M, Ohta Y, Miyazaki K, Kurata T, et al. (2007) Increased autophagy in transgenic mice with a G93A mutant SOD1 gene. Brain Res 1167: 112-117
- Song CY, Guo JF, Liu Y, Tang BS (2012) Autophagy and Its Comprehensive Impact on ALS. Int J Neurosci 122: 695-703.
- Zarei S, Carr K, Reiley L, Diaz K, Guerra O, et al. (2015) A comprehensive review of amyotrophic lateral sclerosis. Surg Neurol Int 6.
- Trivedi S, Tibrewala N, Balsara K (2015) Anaesthetic management of a patient with amyotrophic lateral sclerosis undergoing laparoscopic diaphragmatic pacing. Indian J Anaesth 59: 683-685.
- Sancho J, Servera E, Diaz J, Marin J (2004) Efficacy of mechanical insufflation-exsufflation in medically stable patients with amyotrophic lateral sclerosis. Chest 125: 1400-1405.
- Simonds AK (2017) Progress in respiratory management of bulbar complications of motor neuron disease/amyotrophic lateral sclerosis? Thorax 72: 199-201.
- Banfi P, Ticozzi N, Lax A, Guidugli GA, Nicolini A, et al. (2015) A review of options for treating sialorrhea in amyotrophic lateral sclerosis. Respir Care 60: 446-454.
- Volanti P, Cibella F, Sarva M, De Cicco D, Spanevello A, et al. (2011) Predictors of non-invasive ventilation tolerance in amyotrophic lateral sclerosis. J Neurol Sci 303: 114-118.
- Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, et al. (2009) Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 73: 1218-1226.
- McClellan F, Washington M, Ruff R, Selkirk SM (2013) Early and innovative symptomatic care to improve quality of life of ALS patients at Cleveland VA ALS Center. J Rehabil Res Dev 50: vii-xvi.
- Blackhall LJ (2012) Amyotrophic lateral sclerosis and palliative care: where we are, and the road ahead. Muscle Nerve 45: 311-318.
- Albert SM, Murphy PL, Del Bene ML, Rowland LP (1999) A prospective study of preferences and actual treatment choices in ALS. Neurology 53: 278-283.
- Munroe CA, Sirdofsky MD, Kuru T, Anderson ED (2007) End-of-life decision making in 42 patients with amyotrophic lateral sclerosis. Respir Care 52: 996-999
- Astrow AB, Sood JR, Nolan MT, Terry PB, Clawson L, et al. (2008). Decision-making in patients with advanced cancer compared with amyotrophic lateral sclerosis. J Med Ethics 34: 664-668.
- McDermott CJ, Bradburn MJ, Maguire C, Cooper CL, Baird WO, et al. (2016) DiPALS: Diaphragm Pacing in patients with Amyotrophic Lateral Sclerosis - a randomised controlled trial. Health Technol Assess 20: 1-186
- Miller RG, Lewis RA (2016) Diaphragm pacing in patients with amyotrophic lateral sclerosis. Lancet Neurol. 15: 542.
- Safety and efficacy of diaphragm pacing in patients with respiratory insufficiency due to amyotrophic lateral sclerosis (DiPALS): a multicentre, open-label, randomised controlled trial. Lancet Neurol (2015) 14: 883-892.
- Onders RP, Elmo M, Khansarinia S, Bowman B, Yee J, et al. (2009) Complete worldwide operative experience in laparoscopic diaphragm pacing: results and differences in spinal cord injured patients and amyotrophic lateral sclerosis patients. Surg Endosc 23: 1433-1440
- Proudfoot M, Jones A, Talbot K, Al-Chalabi A, Turner MR, et al. (2016) The ALSFRS as an outcome measure in therapeutic trials and its relationship to symptom onset. Amyotroph Lateral Scler Frontotemporal Degener. 17: 414-425
- Simon NG, Turner MR, Vucic S, Al-Chalabi A, Shefner J, et al. (2014) Quantifying disease progression in amyotrophic lateral sclerosis. Ann Neurol 76: 643-657.
- Bosco DA, Morfini G, Karabacak NM, Song Y, Gros-Louis F, et al. (2010) Wild-type and mutant SOD1 share an aberrant conformation and a common pathogenic pathway in ALS. Nat Neurosci 13: 1396-1403
- Bruijn LI, Cudkowicz M (2006) Therapeutic targets for amyotrophic lateral sclerosis: current treatments and prospects for more effective therapies. Expert Rev Neurother 6: 417-428.
- Smith RA, Miller TM, Yamanaka K, Monia BP, Condon TP, et al. (2006) Antisense oligonucleotide therapy for neurodegenerative disease. J Clin Invest 116: 2290-2296.
- Hogden A, Foley G, Henderson RD, James N, Aoun SM, et al. (2017) Amyotrophic lateral sclerosis: improving care with a multidisciplinary approach. J Multidiscip Healthc 10: 205-215.
- Soofi AY, Bello-Haas VD, Kho ME, Letts L (2017) The impact of rehabilitative interventions on quality of life: a qualitative evidence synthesis of personal experiences of individuals with amyotrophic lateral sclerosis. Qual Life Res.
- Danel-Brunaud V, Touzet L, Chevalier L, Moreau C, Devos D, et al. (2017) Ethical considerations and palliative care in patients with amyotrophic lateral sclerosis: A review. Rev Neurol 173: 300-307.
- Terzano C, Romani S (2015) Early use of non-invasive ventilation in patients with amyotrophic lateral sclerosis: what benefits? Eur Rev Med Pharmacol Sci 19: 4304-4313.
- Pisa FE, Logroscino G, Giacomelli Battiston P, Barbone F (2016) Hospitalizations due to respiratory failure in patients with Amyotrophic Lateral Sclerosis and their impact on survival: a population-based cohort study. BMC Pulm Med 16: 136.
- Bach JR (1993) Amyotrophic lateral sclerosis. Communication status and survival with ventilatory support. Am J Phys Med Rehabil 72: 343-349.
- Cazzolli PA, Oppenheimer EA (1996) Home mechanical ventilation for amyotrophic lateral sclerosis: nasal compared to tracheostomy-intermittent positive pressure ventilation. J Neurol Sci 139: 123-128.
- Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, et al. (2006) Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 5: 140-147.
- Radunovic A, Annane D, Rafiq MK, Mustfa N (2013) Mechanical ventilation for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev.
- Jacobs TL, Brown DL, Baek J, Migda EM, Funckes T, et al. (2016) Trial of early noninvasive ventilation for ALS: A pilot placebo-controlled study. Neurology 87: 1878-1883.
- Carratu P, Spicuzza L, Cassano A, Maniscalco M, Gadaleta F, et al. (2009) Early treatment with noninvasive positive pressure ventilation prolongs survival in Amyotrophic Lateral Sclerosis patients with nocturnal respiratory insufficiency. Orphanet J Rare Dis 4: 10.
- Kataoka H, Nanaura H, Kinugawa K, Uchihara Y, Ohara H, et al. (2017) Risk of Unsuccessful Noninvasive Ventilation for Acute Respiratory Failure in Heterogeneous Neuromuscular Diseases: A Retrospective Study. Neurol Int 9: 6904.
- Cabrera Serrano M, Rabinstein AA (2012) Usefulness of pulmonary function tests and blood gases in acute neuromuscular respiratory failure. Eur J Neurol 19: 452-456.
- Georges M, Golmard JL, Llontop C, Shoukri A, Salachas F, et al. (2017) Initiation of non-invasive ventilation in amyotrophic lateral sclerosis and clinical practice guidelines: Single-centre, retrospective, descriptive study in a national reference centre. Amyotroph Lateral Scler Frontotemporal Degener 18: 46-52.
- Nicholson TT, Smith SB, Siddique T, Sufit R, Ajroud-Driss S, et al. (2017) Respiratory Pattern and Tidal Volumes Differ for Pressure Support and Volume-assured Pressure Support in Amyotrophic Lateral Sclerosis. Ann Am Thorac Soc 14: 1139-1146.
- Park D, Lee GJ, Kim HY, Ryu JS (2017) Different characteristics of ventilator application between tracheostomy- and noninvasive positive pressure ventilation patients with amyotrophic lateral sclerosis. Medicine 96: e6251.
- Bertella E, Banfi P, Paneroni M, Grilli S, Bianchi L, et al. (2017) Early initiation of night-time NIV in an outpatient setting: a randomized non-inferiority study in ALS patients. Eur J Phys Rehabil Med 53: 892-899.
- Miller RG, Anderson F, Brooks BR, Mitsumoto H, Bradley WG, et al. (2009) Outcomes research in amyotrophic lateral sclerosis: lessons learned from the amyotrophic lateral sclerosis clinical assessment, research, and education database. Ann Neurol 65: S24-S28.
- Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, et al. (1999) The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. BDNF ALS Study Group (Phase III). J Neurol Sci 169: 13-21.
- Bedard ME, McKim DA (2017) Continuous Mouthpiece Daytime Amyotrophic Lateral Sclerosis in Noninvasive Ventilation: Definitive Solid Therapy? Reply Respir Care 62: 387-388.
- Morgan RK, McNally S, Alexander M, Conroy R, Hardiman O, et al. (2005) Use of Sniff nasal-inspiratory force to predict survival in amyotrophic lateral sclerosis. Am J Respir Crit Care Med 171: 269-274.
- O'Neill CL, Williams TL, Peel ET, McDermott CJ, Shaw PJ, et al. (2012) Non-invasive ventilation in motor neuron disease: an update of current UK practice. J Neurol Neurosurg Psychiatry 83: 371-376.
- Tilanus TBM, Groothuis JT, TenBroek-Pastoor JMC, Feuth TB, Heijdra YF, et al. (2017) The predictive value of respiratory function tests for non-invasive ventilation in amyotrophic lateral sclerosis. Respir Res 18: 144.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi