Review Article, J Sleep Disor Treat Care Vol: 6 Issue: 2
Monosodium Urate as a Biomarker for Obstructive Sleep Apnea
Abrams B*
MS, 221 Linden Drive, Elkins Park, USA
*Corresponding Author : Burton Abrams, MS
221 Linden Drive, Elkins Park, PA, USA, 19027
Tel: (215)-517-7766
E-mail: burtabrams@hotmail.com
Received: March 31, 2017 Accepted: April 20, 2017 Published: April 27, 2017
Citation: Abrams B (2017) Monosodium Urate as a Biomarker for Obstructive Sleep Apnea. J Sleep Disord: Treat Care 6:2. doi: 10.4172/2325-9639.1000191
Abstract
The hypoxemia which results from obstructive sleep apnea causes three effects which quickly elevate the concentration of serum uric acid, often leading to the precipitation of monosodium urate crystals: cell catabolism which culminates irreversibly in the generation of excess uric acid fed into the blood; serum acidosis and hypercapnia which reduces the solubility of uric acid in the blood; and gradual reduction of the kidneys’ glomerular filtration rate so that the removal of serum uric acid is slowed. Monosodium urate deposits are most likely to form in the extremities or in patellar, biceps, and quadriceps tendons, where they are detectable by ultrasonic means. Once formed, the crystals dissolve very slowly, which allows their detectability at a convenient time, thereby increasing their usefulness as a biomarker for obstructive sleep apnea before its life-threatening consequences develop.
Keywords: Obstructive sleep apnea; Monosodium urate; Ultrasound; Screening
Introduction
Obstructive sleep apnea (OSA) has become recognized as a disease which can have serious, often life-threatening, long term consequences. Meta-analysis estimates that between 9% and 38% of adults in the general population has sleep apnea in at least the mild form [1]. Furthermore, OSA is readily and effectively treatable [2]. Yet, it is woefully underdiagnosed; at least 82% of those with OSA have never been clinically diagnosed [3], partly because there is not yet a reliable screening tool for primary care physicians to use to recommend suspected OSA patients for diagnosis and treatment when indicated. There remains a pressing need for such a tool because OSA is so prevalent, so seriously consequential, so readily treatable, yet so grossly underdiagnosed. Attempts to discover a serum biomarker have not been successful [4], nor have investigations of other biomarkers [5]. Ultrasonic detection of monosodium urate (MSU) may fill that need. The public health benefit would be enormous because more effective screening would lead to early diagnosis and treatment of many more OSA patients.
Consequences of OSA
The recognized consequences of OSA most commonly mentioned are cardiovascular diseases and excessive sleepiness during waking hours [6]. Many cardiovascular diseases are life threatening. The excessive sleepiness during waking hours also can be life threatening if it leads to falling asleep while driving. But there are many other serious consequences of OSA that have been recognized, such as diabetes, kidney disease, Alzheimer’s disease [7,8], cancer [9,10], autoimmune diseases [11], and even shortening of telomeres [12]. In short, OSA has been associated with almost every noninfectious scourge disease of modern life, leading to a very significant impact on mortality [13,14]. Furthermore, recent studies have found that once cardiovascular disease indicators have developed in OSA individuals, neither continuous positive airway pressure [15] nor mandibular advancement [16] treatments for it have much benefit in reversing those indicators. While much research has gone into determining these serious consequences of OSA, what is needed now is a concerted effort to give primary care and other physicians a convenient and effective tool, namely MSU detection, to screen for sleep apnea before its lifethreatening, and often irreversible, consequences develop.
MSU Formation from OSA
The hypoxemia of sleep apnea has three effects which often lead to sleep-period generation of MSU from abrupt supersaturation of serum uric acid. Effect #1 is cellular catabolism in which adenosine triphosphate degradation is accelerated, leading to nucleotide turnover which culminates irreversibly in the transient cellular generation of excess uric acid fed into the blood [17,18], faster than any food would cause. Effect #2 is transient hypercapnia and acidosis, so that the blood can hold less uric acid in solution. Effect #3 is a long term deterioration of the kidneys' glomerular filtration rate so that removal of uric acid from the blood is slowed [19]. If OSA is effectively treated, Effects #1 and #2 don’t occur, and Effect#3 may reverse [20,21].
Thus, with untreated OSA there is an abrupt increase in the influx of uric acid in the blood, slowed efflux, and abruptly reduced storage capacity -- perfect storm conditions for MSU precipitation in body tissues and fluids. Furthermore, after awakening and normal breathing is restored, the first two effects dissipate so that a blood test taken during waking hours misses their peaks. And if MSU has precipitated recently, then the measurement of serum uric acid is greatly undervalued. Thus, measurement of serum uric acid would not be a reliable indicator of OSA, unless blood samples were to be taken at frequent intervals during the sleeping period, which is highly impractical.
But detection of MSU, the serum uric acid precipitate, could be a reliable indicator of OSA. The MSU crystals form quickly, but then dissolve very slowly, if ever [22]. Thus, they are not a transient phenomenon, so their presence can be detected at a convenient time. Furthermore, the physiology described above would indicate that they first form early in the development of OSA, whereas OSA’s other consequences generally appear much later [23]. Thus, MSU detection for OSA screening has the advantage of catching OSA before it leads to other more serious, and often irreversible, consequences.
Current OSA Screening Methods
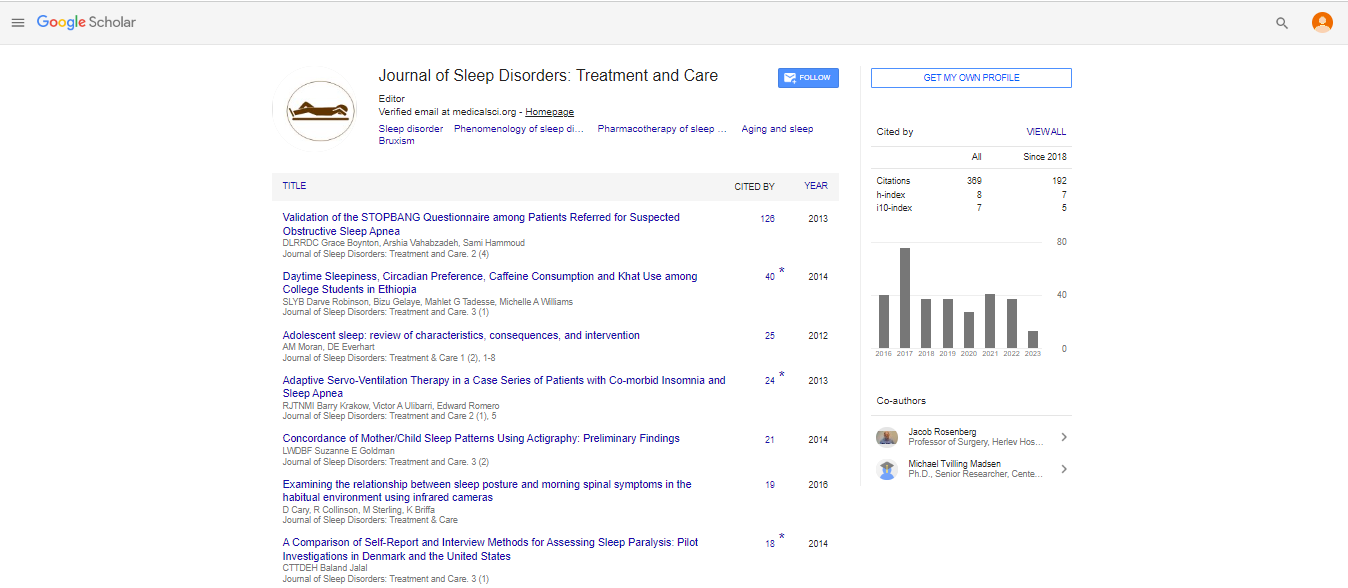
If done at all, OSA screening by physicians is usually done by one of several patient questionnaires (example: STOP BANG questionnaire, Epworth sleepiness scale, Berlin questionnaire) [24], or portions thereof. However, patient answers to some of the questions may not be reliable. For example, the patient may not recognize sleepiness which has increased gradually during the OSA development, whereas the sudden lack of sleepiness may be much more noticeable after OSA is resolved. The patient may not be aware of his or her snoring, or whether anyone else has witnessed apneic events. And there is often excessive physician reliance on body mass index [25]. Whatever the reason for the limitations of current screening methods, the significant under diagnosis of OSA attests to the need for a reliable biomarker which is much less subjective than current screening methods. MSU detection is a strong candidate for that biomarker.
Ultrasonic Detection of MSU Crystals
The formation of MSU crystals in body fluids and tissues is the modern definition of gout [26,27]. Only some cases of gout present the symptoms of arthritic pain and inflammation, or visible or palpable subcutaneous tophi, or uric acid kidney stones. When MSU crystals form in synovial fluid, they cause arthritic gout. The connection of OSA with symptomatic gout has been described previously for sleep medicine practitioners [28] and for rheumatologists [29,30].
Recent gout studies using ultrasonic inspection or dual energy computed tomography [31] have found aggregations of MSU crystals and tophi clustered around bones and tendons, even in cases where symptomatic gout has never manifested [32-34]. Dual energy computed tomography has finer resolution for better imaging, but the safer use of ultrasound provides very good detection, which is all that is required for this purpose. Because the internal body temperature is lowest in the extremities during sleep, MSU crystals are likely to precipitate in those areas. Other likely areas are the distal insertion of the patellar tendon [35] and the triceps and quadriceps tendons [36]. Thus, ultrasonic inspection of these areas for MSU crystals is proposed as the OSA biomarker.
Verification of the Biomarker
In order to verify that MSU detection is a reliable biomarker for OSA, a study is needed to demonstrate adequate sensitivity and selectivity. Sensitivity can be demonstrated by using ultrasonic detection of the presence or absence of MSU on a cohort of diagnosed OSA patients, keeping track of the time elapsed since their original OSA diagnosis and whether or not they are using an urate-lowering drug. Selectivity can be demonstrated by using the same ultrasonic detection methods on a cohort of similar individuals distinguished only by assurance that they do not have OSA. Demonstration of adequate sensitivity and selectivity by these methods will verify that MSU detection by ultrasound is a reliable biomarker for OSA.
Performing these sensitivity and selectivity calculations requires a binary decision as to whether MSU is present or not, as well as a binary decision as to whether OSA is present or not. For OSA, the algorithm is well established based on calculation from the continuum of polysomnographic data leading to a decision as to whether OSA is present (ie, treatment is recommended) or not present (ie, treatment is not recommended). One should anticipate that ultrasonic measurements will also span a continuum of MSU densities which need binary quantization to decide that MSU is present (ie, density above a selected threshold) or MSU is not present (ie, density below the threshold). The algorithm to determine that decision threshold will be an important aspect of the study.
Conclusion
Once verified, the ultrasonic detection of MSU would be an important biomarker for MSU screening as a standard practice by primary care and other physicians. The resulting early diagnosis and treatment of many more patients with obstructive sleep apnea would have an enormous public health benefit.
References
- Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, et al. (2016) Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev pii: S1087-0792.
- Calik MW (2016) Treatments for Obstructive Sleep Apnea. J Clin Outcomes Manag 23: 181-192.
- Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20: 705-706.
- Archontogeorgis K, Nena E, Papanas N, Steiropoulos P (2014) Biomarkers to improve diagnosis and monitoring of obstructive sleep apnea syndrome: current status and future perspectives. Pulm Med 2014: 930535.
- Montesi SB, Bajwa EK, Malhotra A (2012) Biomarkers of sleep apnea. Chest 142: 239-245.
- Pinto JA, Ribeiro DK, Cavallini AF, Duarte C, Freitas GS (2016) Comorbidities Associated with Obstructive Sleep Apnea: a Retrospective Study. Int Arch Otorhinolaryngol 20: 145-150.
- Abrams B (2005) Add Alzheimer's to the list of sleep apnea consequences. Med Hypotheses 65: 1201-1202.
- Pan W, Kastin AJ (2014) Can sleep apnea cause Alzheimer's disease? Neurosci Biobehav Rev 47: 656-669.
- Abrams B (2007) Cancer and sleep apnea--the hypoxia connection. Med Hypotheses 68: 232.
- Martinez-Garcia MA, Campos-Rodriguez F, Barbe F (2016) Cancer and obstructive sleep apnea current evidence from human studies. Chest 150: 451-463.
- Abrams B (2005) Long-term sleep apnea as a pathogenic factor for cell-mediated autoimmune disease. Med Hypotheses 65: 1024-1027.
- Boyer L, Audureau E, et al. (2016) Telomere Shortening in Middle-Aged Men with Sleep-disordered Breathing. Ann Am Thorac Soc 13: 1136-1143.
- Young T, Finn L, Peppard PE, Szklo-Coxe M, Austin D, et al. (2008) Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 31: 1071-1078.
- Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, et al. (2008) Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 31: 1079-1085.
- McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, et al. (2016) CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N Engl J Med 375: 919-931.
- Gagnadoux F, Pépin JL, Vielle B, Bironneau V, Chouet-Girard F, et al. (2017) Impact of Mandibular Advancement Therapy on Endothelial Function in Severe Obstructive Sleep Apnea. Am J Respir Crit Care Med.
- Hasday JD, Grum CM (1987) Nocturnal increase of urinary uric acid:creatinine ratio. A biochemical correlate of sleep-associated hypoxemia. Am Rev Respir Dis 135: 534-538.
- Grum CM (1992) Cells in crisis. Cellular bioenergetics and inadequate oxygenation in the intensive care unit. Chest 102: 329-330.
- Ahmed SB, Ronksley PE, Hemmelgarn BR, Tsai WH, Manns BJ, et al. (2011) Nocturnal hypoxia and loss of kidney function. PLoS One 6: e19029.
- Kinebuchi S, Kazama JJ, Satoh M, Sakai K, Nakayama H, et al. (2002) Short-term use of continuous positive airway pressure ameliorates glomerular hyperfiltration in patients with obstructive sleep apneoa syndrome. Clin Sci (Lond) 107: 317-322.
- Koga S, Ikeda S, Yasunaga T, Nakata T, Maemura K, et al. (2013) Effects of nasal continuous positive airway pressure on the glomerular filtration rate in patients with obstructive sleep apnea syndrome. Intern Med 52: 345-349.
- Perez-Ruiz F, Dalbeth N, Bardin T (2015) A review of uric acid, crystal deposition disease, and gout. Adv Ther 32: 31-41.
- Huang QR, Qin Z, Zhang S, Chow CM (2008) Clinical patterns of obstructive sleep apnea and its comorbid conditions: a data mining approach. J Clin Sleep Med 4: 543-550.
- Stelmach-Mardas M, Iqbal K, Mardas M, Kostrzewska M, et al. (2017) Clinical Utility of Berlin Questionnaire in Comparison to Polysomnography in Patients with Obstructive Sleep Apnea. Adv Exp Med Biol.
- Cho JH, Choi JH, Suh JD, Ryu S, Cho SH (2016) Comparison of Anthropometric Data Between Asian and Caucasian Patients With Obstructive Sleep Apnea: A Meta-Analysis. Clin Exp Otorhinolaryngol 9: 1-7.
- Terkeltaub R, Edwards NL (2011) Gout: Diagnosis and Management of Gouty Arthritis and Hyperuricemia 2nd Edition. Professional Communications Inc, USA.
- USA Centers for Disease Control and Prevention.
- Abrams B (2005) Gout is an indicator of sleep apnea. Sleep 28: 275.
- Abrams B (2010) Gout as an early warning of concomitant sleep apnea. J Clin Rheumatol 16: 305.
- Zhang Y, Peloquin CE, Dubreuil M, Roddy E, Lu N, et al. (2015) Sleep Apnea and the Risk of Incident Gout: A Population-Based, Body Mass Index-Matched Cohort Study. Arthritis Rheumatol 67: 3298-3302.
- Fodor D, Nestorova R, Vlad V, Micu M (2014) The place of musculoskeletal ultrasonography in gout diagnosis. Med Ultrason 16: 336-344.
- Pineda C, Amezcua-Guerra LM, Solano C, Rodriguez-Henríquez P, Hernández-Díaz C, et al. (2011) Joint and tendon subclinical involvement suggestive of gouty arthritis in asymptomatic hyperuricemia: an ultrasound controlled study. Arthritis Res Ther 13: R4.
- García Puig J, Beltrán L, Mejía Chew C, Torres R, Tebar Márquez D, et al. (2016) Ultrasound in the diagnosis of asymptomatic hyperuricaemia and gout. Rev Clin Esp 216: 445-450.
- Ventura-Ríos L, Sánchez-Bringas G, Pineda C, Hernández-Díaz C, Reginato A, et al. (2016) Tendon involvement in patients with gout: an ultrasound study of prevalence. Clin Rheumatol 35: 2039-2044.
- Andia I, Abate M (2016) Hyperuricemia in Tendons. Adv Exp Med Biol 920: 123-132.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi