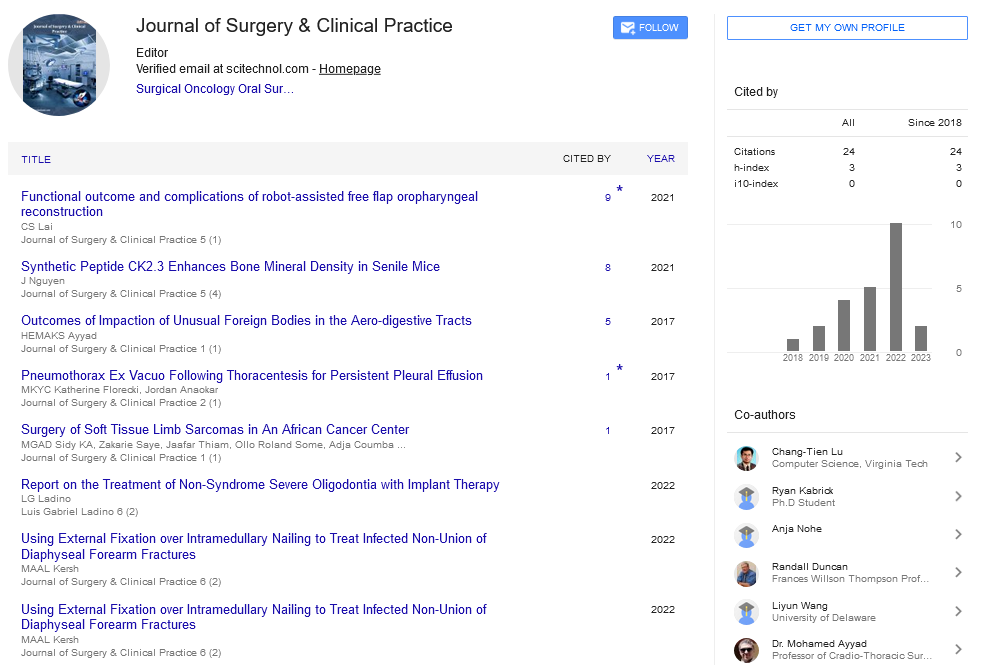
Case Report, J Surg Clin Pract Vol: 1 Issue: 1
Late Postappendectomy Faecal Fistula
Doru Moga*, Remus Maxim, Adrian Popen�?£iu, �?�?tefan Peri�?�?anu, Vanina Sab�?�?u and Horea Magdu
Department of General Surgery, “Alexandru Augustin” Military Emergency Hospital, Sibiu, Romania
*Corresponding Author : Moga Doru, MD, PhD
Department of General Surgery, Military Emergency Hospital Sibiu 44-46 Victoriei Blvd, 550024 Sibiu, Romania
E-mail: mogadoru@yahoo.com
Received: November 16, 2016 Accepted: November 25, 2017 Published: November 02, 2017
Citation: Moga D, Maxim R, Popen�?£iu A, Peri�?�?anu S, Sab�?�?u V, et al. (2017) Late Postappendectomy Faecal Fistula. J Surg Clin Pract 1:1
Abstract
Introduction: Appendectomy is one of the most common surgical intervention. Partial appendectomy may allow for potential late complications.
Presentation of Case: We present the case of a patient with an enterocutaneous fistula, that occured four years postapendectomy. Following surgery it was discovered an appendico-cutaneous fistula through the presence of a blunt long, dehiscent cutaneous appendix. The completion of the appendectomy led to healing.
Discussion and Conclusion: An appendix stump too long may cause the emergence of a appendico-cutaneous fistula.
Keywords: Faecal fistula; Stump appendicitis; Appendico-cutaneous fistula
Introduction
Acute appendicitis is the most common cause of acute surgical abdomen and appendectomy is one of the most common abdominal surgeries in the field. Incomplete appendectomy forfeits in the peritoneal cavity the appendix tip or an appendix stump too long [1]. It is recomended that the remaining appendicular stump length should be <0.5 cm [2]. Incomplete appen-dectomy is more commonly seen in the context of acute appendicitis, but was also seen in the case of chronic appendicitis [1]. The remaining segment can be a source of immediate complications (peritonitis, abscess, fistula purulent) or late ones (inflammation, abscess, fistula) [1]. The inflamation of the remaining appendix stump (stump appendicities) has the same symptoms as those of primary appendicitis.
Case Report
We present the case of a patient age 25, with mild mental retardation who was hospitalized on our ward in September 2014 showing a stercoral fistula at the post-appendectomy scar level in the right iliac fossa, with a daily flow of about 20-30 ml. Anamnesis the fistulous drainage debut was 3-4 weeks ago, after a spontaneous evacuation of a parietal abscess. To note that the patient was operated for acute appendicitis at the territorial hospital in 2010. In the postoperative period the patient was transferred to another surgical section showing a necrotizing fascitis in the right iliac fossa, with slow healing per secundam. Later, in 2012 the patient returned, presenting a right iliac fossa abscess that required incision. The patient is addmited in good general condition, afebrile, showing bowel movements, and no other significant pathological complaints. Local exam of the postoperative scar in the right iliac fossa, showed a fistulous orifice diameter of 1.5 cm. On exploring it, was visualized under the aspect of intestinal lumen. Biological samples were not modified and the abdominal fluoroscopy without hidroaerice levels or pneumoperitoneum. On September 24, 2014 the patient is operated on under spinal anesthesia through a McBurney incision in the right iliac fossa that circumscribed the fistulous hole. Excision of the scar tissue and of the ulcerated and inflamed skin area is performed. It was identified a proximal appendix bunt of 2.5 cm length, having the distal end beant fixed to the abdominal wall (Figures 1 and 2). We proceeded to the completion of appendectomy with inverting the stump (Figures 3 and 4). Postoperative evolution was uneventful. She was discharged on the fifth postoperative day. Histological examination of the resected specimen revealed an inflamed appendiceal stump. A follow-up consult one month after surgery showed a patient in good general health with no symptoms (Figure 5).
Discussion
Complications encountered after appendectomy include woundsite infection, postoperative illeus, intra-abdominal abscess, and leaks from the remnant stump [3]. The fact that the diagnosis of stump appendicitis is usually not considered as the possible etiology for right lower quadrant abdominal pain in patients with prior appendectomy creates a delay in making the correct diagnosis and explains why the rate of perforation for stump appendicitis approaches 70% [4]. The first to describe stump appendicitis for patients who had previously undergone an appendectomy for appendicitis was Rose in 1945 [5]. It is defined as the interval re-inflammation of any residual appendiceal tissue after appendicectomy [2]. This complication can occur both after the classical appendicectomy and after the laparoscopic one. Because of the lack of a 3-dimensional view and lack of tactile feedback, some authors consider that laparoscopic appendectomy is a risk factor for stump appendicitis [5]. The time from appendectomy to the development of stump appendicitis ranges from 2 months to 21 years. The length of the stump ranges from 1.3 cm to 5.1 cm [6]. The common acquired causes of enterocutaneous fistula include strangulated groin hernia especially femoral hernia, tuberculosis and other granulomatous infections, diverticular disease of the bowel, Crohn’s disease, carcinoid tumour and carcinoma of the caecum and appendix [7], foreign body, radiation, nutritional debilitation, and distal obstruction [8]. It bears serious social, psychological, medical and nutritional hazards [8]. An appendicocutaneous fistula was first described by Volz in 1846 at autopsy [9]. Cutaneous fistula may develop after drainage of appendix abscess or after appendicectomy or it may develop spontaneously as a complication of acute perforating appendicitis or as a hazard of incomplete appendicectomy [10-12]. Complete surgical removal of an inflamed appendix is the treatment for stump appendicitis.
Conclusion
During appendectomy should be avoided leaving a long appendix blunt as it may cause complications. Among the causes of stercoral fistula may include apendico-cutaneous fistula. The differential diagnosis of a right iliac fossa pain of a patient with appendicectomy, the posibility of stump appendicitis should not be overlooked.
Acknowledgement
The Authors thank Mrs Andra Riti for providing language help.
References
- Setlacec D, A�?�?chie I (1999) Complica�?£ii severe postapendicectomie. Bucure�?�?ti: Ed. Medical�?�?.
- Kanona H, Al Samaraee A, Nice C, Bhattacharya V (2012) Stump appendicitis: A review. Int J Surg 10: 425-428
- Çiftci F, Abdurrahman I, Tatar Z (2015) Stump Appendicitis: A Clinical Enigma. Chirurgia 110: 562-564.
- Awe JAA, Soliman AM, Gourdie RW (2013) Stump Appendicitis: An Uncompleted Surgery, a Rare but Important Entity with Potential Problems. Case Reports in Surgery: 972596.
- Constantin V, Popa F, Carâp A, Socea B(2014) Stump Appendicitis – An Overlooked Clinical Entity. Chirurgia 109: 128-131.
- Mentes O, Zeybek N, Oysul A, Onder SC, Tufan T (2008) Stump appendicitis, rare complication after appendectomy: report of a case. Ulus Travma Acil Cerrahi Derg 14: 330-332.
- Singal R, Gupta S, Mittal A, Gupta S, Singh M (2012) Appendico-cutaneous Fistula Presenting as a Large Wound: a Rare Phenomenon – Brief Review. Acta Med Indones 44: 53-56.
- Shamim M, Haider SA, Iqbal SA (2009) Persistent appendiceal faecal fistula following a complicated open appendicectomy. J Pak Med Assoc 59: 181-183.
- Hyett A (1995) Appendiculocutaneous fistula: a hazard of incomplete appendicectomy. Aust NZJ Surg 65: 144-145.
- Koak Y, Jeddy TA, Gidings AEB (1999) Apendico-cutaneous fistula. J R Soc Mec 92: 639-640.
- Chowdhury DAH, Hassan MF, Rahman M, Anwar AB, Khatun S (2008) Spontaneous appendico-cutaneous fistula, after drainage of a right loin abscess – A case report. Int J Surg 6: 97-99.
- Haoudi KE, Majdoub KI (2014) Fistule appendiculo-cutanée: complication rare de l’appendicite aiguë. Pan African Med J 19: 194.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi