Research Article, J Ergon Res Vol: 2 Issue: 1
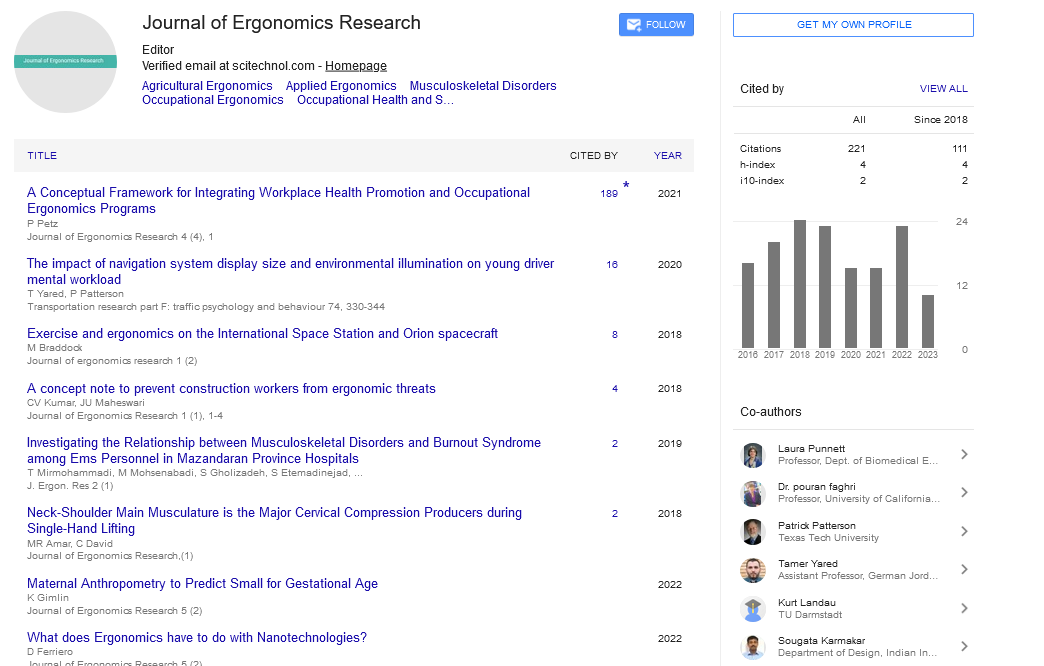
Investigating the Relationship between Musculoskeletal Disorders and Burnout Syndrome among Ems Personnel in Mazandaran Province Hospitals
Mirmohammadi T, Mohsenabadi M*, Gholizadeh S, Etemadinejad S, Yazdani J, Bozorgi F, Ahmadi M
Department of Medical Sciences, University of Mazandaran, Mazandaran, Iran
*Corresponding Author : Mohsenabadi M
Department of Medical Sciences, University of Mazandaran, Mazandaran, Iran
E-mail: m.mohsenabadi@gmail.com
Received: September 11, 2018 Accepted: October 10, 2018 Published: February 02, 2019
Citation: Mirmohammadi T, Mohsenabadi M, Gholizadeh S, Etemadinejad S, Yazdani J, et al. (2019) Investigating the Relationship between Musculoskeletal Disorders and Burnout Syndrome among Ems Personnel in Mazandaran Province Hospitals. J Ergon Res 2:1.
Abstract
Background and aims: The main objective of this research was finding the relations between musculoskeletal disorders and job burnout among pre-hospital emergency staff that supervised by Mazandaran University of Medical Sciences.
Methods: In this study, 224 individual were selected randomly in 2016 from 365 pre-hospital emergency staff, supervised by Mazandaran University of Medical Sciences. Socio-demographic, Nordic Musculoskeletal Disorders and Maslach job burnout questionnaire were applied as research tools. SPSS v.19.0 software and statistical techniques such as t-test, and ANOVA were employed to analyzing the data.
Results: Moderate levels of severity and frequency of feelings of depersonalization and lack of personal accomplishment and high levels of emotional exhaustion reported. Also, work-related musculoskeletal disorders were also at high level. It was found that there is a significant relationship between musculoskeletal disorders and job burnout. Significant differences among the three components of burnout with an emphasis on "marriage" and "work experience" was determined.
Conclusion: Job burnout and work-related musculoskeletal disorders (WMSDs) of pre-hospital emergency staff is in the high level in order to the harmful nature of their jobs. Emergency managers and physicians have lower depression in comparison with other groups because of their low physical pressure. Further to the stressful nature of emergency job without concerning the job position, whole of the staff have high musculoskeletal disorders. It is necessary for the proper authorities to track and providing the necessary solutions in terms of economic, environmental, management and staff people, to help them.
Keywords: Musculoskeletal; Disorders; Physical pressure
Introduction
These days, it's priority and necessary to prevent musculoskeletal disorders on workspaces in practical measures. Several studies investigate that pain in various parts of musculoskeletal system of the body is one of the majore problems on workspaces cause more than half of work absences [1]. Complications such as psychosocial stress, increasing musculoskeletal disorders (MSDs), inertia and fatigue are the causes of poor technology development despite of increasing production and productivity. Musculoskeletal disorders in industrial and developing countries are common causes of work injuries and disability. These disorders start with pain and cause sikness [2]. NIOSH (National Institute of Safety and Health) has categorized occupational diseases and complications based on importance in prevalence, sevierty, and prevention in which WMSDs rank secound after occupational respiratory illnesses. Studies showed that musculoskeletal disorderes economically are very costly so that ranked first in incidence and pain suffering individuals in which low back pain (LBP) is first of all of these disorders [3]. According to the report of the Deputy Director of Treatment of the Social Security Organization of the Islamic Republic of Iran during the years 1370 to 1373, MSDs caused 14.4% of the total incapacity in the country. In this regard, after neurological diseases (16.8%), Psychological illnesses (16.1%) and cancer (16%) had the fourth rank [4]. The incidence of MSDs basically are affected with different factors such as: heavy physical works, static postures at work, bending and rapid rotations, picking up heavy objects, pulling and pushing loads, repeated works, vibration, and psychosocial and psychological stress [5,6]. Work psychological characteristics are of most important risk factors of MSDs incidences [7]. Several studies demonstrated that both psychosocial factors and work physical demands have significant effect on work life quality of individuals [8,9]. Although physical factors exposure and poisioning are mostly controlled in work environments, so additional investigating about psychosocial situations is required. Occupational psychosocial factors include job requirements, support (from organizations and employers), job security, and job satisfaction [10,11]. Occupational physical factors are also in communication and may iteract potentially with psychosocial factors thus can increase MSDs risk. Recent epidemiological studies about back, wrists and upper torso disorders investigated that psychosocial work related factors in exposed workers increase MSDs risk when interacts with physical risk factors at work, the increase which is due to the interaction between psychosocial and physical factors can cause increase in MSDs risk even the physical risk factors exposure is low. However, the more exposure with both risk factors, the most MSDs risk occur [12,13]. One of psychological problems at work environments is the work related burnout and it occurs in tasks facing and make closer communication with other people during work time. Now a day, anyone in any place and position, can feel different levels of burnout on his/her workplace and it’s an undeniable reality at modern work environments [14]. During the existing statistics, one of seven employees got burned out in the end of work day. Among the jobs, health care personnels have the highest incidence of occupational injuries, such as burnout syndrome, the US Department of the Interior reported [15]. Job burnout is one of the various psychosocial risk factors certain impressions which appear in somatoform symptoms [16]. Various factors such as shift working, inadequate use of personal abilities, work overload, ambiguity of job prospects, pey discrimination, realationships with colleagues, unfamiliarity of individual or organizational goals, leadership and management practices at superficial levels, hard and inflexible laws and regulations in organizations causing negative and pessimistic tendencies on clients and colleagues, so can lead to changing behavior between employees and clients making short-tempered and immoral staff, so reduces daily work activities. Therefore, improving the situation causes better relationships in the workplace 18. 17. Borritz et al. [17] conducted a study entitled “Occupational Burnout of Emergency Medical Staff in Hamedan Province” on 110 individuals of EMS. The findings showed that EMS operational personnel’s had moderate severity and frequency of emotional exhaustion, and personality deprivation, and particularly, high level of personal insecurity Khatibian et al. [18] investigated the relationship between occupational stresses with job burnout in pre-hospital emergency staff on 44 EMS departments in Golestan province during 1391-92 (2011-2012). They found that 117 individuals (75.5%) had moderate to high stress in which organizational factors had the highest score in causing stress, and physical, occupational, and group factors had the lower effects respectively. Among all subjects, 76.6% had experienced moderate to high burnout and there was a significant correlation between the overall level of job stress and burnout [19]. The prehospital emergency technicians in Isfahan showed average levels of emotional exhaustion and depersonalization intensity and frequency and feel highly unaccomplished Moradi et al. [20]. Nurses of 5 hospitals in Tehran, reported their high emotional exhaustion, high depersonalization and feeling low competent. The most factor contributing in nurses’ burnout in assessed private sectors was the inappropreatness between income and the wowrkload and its difficulties Masoudi et al. [21]. Mahmudi et al. [22] in a study abut the relationship between nurses’ burnout with Physical conditions and specialized facilities of work place (2006), found that the highest level of job burnout had been on emotional dimension (8.43%). Honkonen et al., performed an investigation among 3368 individuals between 30 to 64 years old to find the association between burnout and physical illness in the general population. They showed that people with higher level of burnout, have been developed more physical illnesses and the prevalence of illnesses has a direct relation with the intensity of depression. Thus, burnout had direct relation with heart disease in men and musculiskeletal disorders in women in which these disorders increased by depression [23]. Langballe et al. [24] studied the relationship between burnout and musculoskeletal pain in seven occupational groups with 4507 personnal of different jobs. The study demonstrated that burnouthave relationship with musculoskeletal pain and its severity have a significant relation among women, men and various jobs. Sorour et al., investigated the relationship between MSDs, job demands, and burnout among 58 emergency nurses and showed that prevalence of MSDs have significant relationship with job demands and job burnout also [25]. Elen et al. [26] studied job burnout prevalence in 550 oncologists on 2014 working on oncology units. Results showed that they are suffered from emotional exhaustion, depersonalization, and a lack of personal accomplishment with 51.2%, 31.8%, and 6.8% respectively. Abdolghafour et al., studied burnout syndrome among physicians working in primary health care centers in Kuwait on 2011. They represented more than half (56%) of women participated in the study were 30-49 years old and 51% were not Kuwaitian nationality. They showed that emotional exhaustion and depersonalization had the lowest percentage, which is positive result; and personal accomplishment and physicians envolvement were in mild score. The investigated results were as nationality, work place, the job, and income have significant relations with job burnout elements. Totally, job burnout syndrome is prevalent between physicians on primary health care units. This syndrome is more prevalent among not-Kuwaitian physicians, general physicians and individuals with lower income [27]. As, careing about health to increase the effeciancy on processes and avoid job related injuries is important, so investigate the prevalence of causes and relations between risk factors and represented disorders can be efficient to achieve best work environment goals. EMS staff are mostly in expose of job burnout and MSDs risk factors [28]. The present study will be performed to investigate the relations between MSDs and job burnout syndrome as in recent years no investigations were performed about EMS staff in the subject [29].
Methods
This is a descriptive investigstion. 224 individuals have been randomatically chosen as samples from 365 prehospital EMS bases staff supervised by Mazandaran University of Medical sciences in 1395. Three questionnaires were applied such as personal and job information, Nurdick musculoskeletal disorders, and Maslach burnout questionnaire. All participants were told about privacy and security of collected data.
Tools
1-The personal-job questionnaire: This questionnaire includes information such as height, weight, age, sex, base of work, work experience, employment status, marital status, number of children, education level, activity type, the amount of work, shift of work, the amount of overwork, and economical status.
2-Nurdick musculoskeletal disorders questionnaire: this questionnaire has been designed and revealed in 1987 by Corinca et al., in occupational health institute of Scandinavian countries, and reliability and validity of the questionnaire has been qualified and approved by related experts [30]. The preseted questionnaire, divides the mechanical system of the body into 9 parts, includes demographic information, general body information and specially information about back, shoulders and neck in which such part has been completed by the questioner and the other part fill out by the participant.
3-The Maslach burnout inventory questionnaire: This questionnaire is the most common tool to assess job burnout which includes 22 separate parts and covers each three aspect of job burnout (e.g. exhaustion, depersonalization and personal unaccomplishment). This questionnaire consists 3 items about emotional exhaustion (allows participants to express excessive weakness and emotional exhaustion in front of patients and workspace), 9 items about depersonalization (allows the participants to express their sight about unconcern’s and indifference to other patients), and 2 items about personal unaccomplishment (allows the participants to express the amount of competence and achieving success in care of patients). Maslach and Jackson report 0.71 to 0.9 for the internal reliability of the questionnaire and report internal reliability of each subscale at the optimal level as fallow: emotional exhaustion (r=0.9), depersonalization (r=0.79) and personal unaccomplishment (r=0.71). the scientific credit of this tool reported more than 0.9 [31]. the frequency of these emotions ranked as 0 to 6 (never, several times a year, once a month, several times a month, once a week, every day), and the severity 0 to 7 (never, seldom, rarely, sometimes, average, usually, much, very much). The the Maslach job burnout demonstrating scores for the frequency are as follows:
Low emotional exhaustion: score lower than 17
Moderate emotional exhaustion: score between 18-29
High emotional exhaustion: score more than 30
Low depersonalization: score lower than 5
Moderate depersonalization: score between 6-11
High depersonalization: score more than 12
Low personal unaccomplishment: score more than 40
Moderate personal unaccomplishment: score between 34-39
High personal unaccomplishment: score lower than 33
For severity instruction scores are as follows:
Low emotional exhaustion: score lower than 25
Moderate emotional exhaustion: score between 26-39
High emotional exhaustion: score more than 40
Low depersonalization: score lower than 6
Mpderate depersonalization: score between 7-14
High depersonalization: score more than 15
Low personal unaccomplishment: score more than 44
Moderate personal unaccomplishment: score between 37-43
High personal unaccomplishment: score lower than 36
Results
Most of the personels are between 35 to 45 years old and 10.3% of them are more than 45. Among the personals, only 0.4% of them are lose weight and most of them about 54% have normal weight, but 37.6% of them are a little over weight and 8% of them are excessive overweight with a BMI higher than 30. Most of them (81.3%) are married and 18.3% of them are single. Most of married staff (34.4%) has only one child and 29.5% of them don’t have any child. Official and contractual staff with 61.2% and 25% have the largest number, in which most of them have bachelor and only 3.1% of them have master degree or higher. Most of the personals (54.5%) have lower than 10 years’ work experience, that with maximum rate (61.6%) work time lower than 200 hr per month and with maximum rate (41.4%) amount of overtime work lower than 75 hr per month, most of them (66.1%) have normal and also 22.8% have weak and only 11.2% have good economic status. 89.7% are right handed and also because of the type of the job all of them were men. Table 1 shows the descriptive statistics of job burnout dimensions consists: frequency and severity of emotional exhaustion, depersonalization and personal unaccomplishment.
Table 1 represents that job burnout is affected with low severity and frequency of emotional exhaustion 39.7% and 60.7% respectively, and also low severity and frequency of personal unaccomplishment 53.1% and 68.8% respectively, and low severity and frequency of depersonalization under the influence 53.7% and 54.5% respecrively are contributed to reduce job burnout.
| Subscales | Low | Medium | High | Total | |
|---|---|---|---|---|---|
| Emotional exhaustion | Frequency | (39.7)89 | (34.8)78 | (25.4)57 | (100)224 |
| Severity | (60.7)136 | (32.1)72 | (7.1)16 | (100)224 | |
| Depersonalization | Frequency | (52.7)118 | (27.7)62 | (19.6)24 | (100)224 |
| Severity | (54.5)122 | (26.8)60 | (18.8)42 | (100)224 | |
| Personal unaccomplishment | Frequency | (53.1)119 | (22.8)51 | (24.1)54 | (100)224 |
| Severity | (68.80154 | (26.8)60 | (4.5)10 | (100)224 |
Table 1: Descriptive statistics of job burnout dimensions: frequency (%) (n=224).
The Tables 2, 3 and 4 are represent descriptive statistics about general Nordick musculoskeletal disorders questionare consist: neck, shoulders, elbow, wrist and hand, back, lower back, hips and thighs, knees and legs or ankle, including 3 stages:
| Body parts | No | Yes | Yes in right side | Yes in left side | Yes in both sides |
|---|---|---|---|---|---|
| Neck | (52.2)117 | (47.8)107 | - | - | - |
| Shoulder | (61.1)148 | - | (12.1)27 | (11.6)26 | (10.3)23 |
| Elbow | (77.2)173 | - | (8.9)20 | (6.3)14 | (7.6)17 |
| Wrist and hand | (79.1)161 | - | (13.8)31 | (5.4)12 | (8.9)20 |
| Back | (62.5)140 | (37.5)84 | - | - | - |
| Lower back | (34.8)78 | (65.2)146 | - | - | - |
| Hip or thighs | (69.6)156 | (30.4)68 | - | - | - |
| Both knees | (57.1)128 | (42.9)96 | - | - | - |
| Both legs | (82.6)185 | (17.4)39 | - | - | - |
Table 2: Nordick musculoskeletal disorder’s statistic questionnaire. Have you had pain, uncomfortabality or numb in last 12 months in parts below? Frequency: (percent) (n=224).
| Body parts | No | Yes | Yes in right side | Yes in left side | Yes in both sides |
|---|---|---|---|---|---|
| Neck | (75.9)170 | (24.1)54 | - | - | - |
| Shoulder | (82.1)84 | - | (4)9 | (7.1)16 | (7.6)15 |
| Elbow | (88.4)198 | - | (3.6)8 | (2.7)6 | (5.4)12 |
| Wrist and hand | (88.4)198 | - | (4)9 | (2.2)5 | (5.4)12 |
| Back | (72.2)173 | (22.5)51 | - | - | - |
| Lower back | (57.6)129 | (42.4)95 | - | - | - |
| Hip or thighs | (84.4)198 | (15.6)35 | - | - | - |
| Both knees | (73.2)164 | (26.8)60 | - | - | - |
| Both legs | (91.4)2.4 | (8.9)20 | - | - | - |
Table 3: Nordick musculoskeletal disorder’s statistic questionnaire. Have you had pain, uncomfortabality or numb in last 7 days in parts below? Frequency: (percent) (n=224)
| Body parts | No | Yes | Yes in right side | Yes in left side | Yes in both sides |
|---|---|---|---|---|---|
| Neck | (76.8) 172 | (23.2) 52 | - | - | - |
| Shoulder | (84.4) 189 | - | (4.9) 11 | (4.9) 11 | (5.8) 13 |
| Elbow | (88.4) 198 | - | (3.6) 8 | (4.5) 10 | (3.6) 8 |
| Wrist and hand | (87.5) 196 | - | (4.5) 10 | (1.8) 4 | (6.3) 14 |
| Back | (82.1) 184 | (17.9) 40 | - | - | - |
| Lower back | (59.8) 134 | (40.2) 90 | - | - | - |
| Hip or thighs | (85.3) 191 | (14.7) 33 | - | - | - |
| Both knees | (79.9) 179 | (20.1) 45 | - | - | - |
| Both legs | (92.9) 208 | (7.1) 16 | - | - | - |
Table 4: Nordick musculoskeletal disorder’s statistic questionnaire. Have you been failed in doing house works, hobbies, work activities or daily activities in past 12 months because of musculoskeletal disorder? Frequency: (percent) (n=224).
1) Have you had pain, uncomfortabality or numbness in last 12 months in parts below?
2) Have you had pain, uncomfortabality or numbness in 7 passed days in parts below?
3) Have you been failed in doing house works, hobbies, work activities or daily activities in passed 12 month because of musculoskeletal disorder?
Descriptive statistical analysis showed that in past 12 months most of the muscular disorders was in lower back with 65.2% and the least was in their legs with 17.4%.
In past 7 days most of the muscular disorders was in their lower back, too (42.4%) and also the least was in their legs (8.9%).
In past 12 months they have been failed doing daily works or hobbies, job and tasks mostly because of pain in their lower back (40.2%) and rarely because of pain in legs (7.1%).
The amounts of F factor showing that there was no significant difference between three elements of job burnout due to the different levels of age, BMI, children quantity, employment status, education, economical status, work time and different levels of overtime work. Table 5 shows the job burnout rate due to marital status; according to amounts of F, there was no significant difference between two elements of depersonalization, and personal unaccomplishment, among the various levels of marital status (single, married and other), but in the element of emotional exhaustion there is a significant difference due to averages in levels of marital status (P>0.05); and staff with status of “other”, “married” and “single” respectively feel the emotional exhaustion more than others.
| Variable | Levels | Average | SD | F | Significance level |
|---|---|---|---|---|---|
| Emotional exhaustion | Single | 18.66 | 12.56 | 3.055 | 0.049 |
| Married | 22.31 | 12.04 | |||
| Other | 43 | - | |||
| Depersonalization | Single | 6.56 | 6.21 | 0.842 | 0.432 |
| Married | 8 | 6.32 | |||
| Other | 3 | - | |||
| Personal unaccomplishment | Single | 24.63 | 13.35 | 1.355 | 0.26 |
Table 5: Comparative investigation of emotional exhaustion with emphasis on marital status.
Table 6 presents the job burnout ratio due to work shifts. The amounts of F factor represented that there is no significant difference between two elements of emotional exhaustion, personal unaccomplishment and different levels of work shifts (fixed and alternative work shifts), but in depersonalization averages, there is a significant difference with levels of work shifts (p>0.05); and staff with alternative and fixed shifts feel more depersonalization respectively.
| Variable | Levels | Average | SD | F | T | Significance level |
|---|---|---|---|---|---|---|
| Emotional | Fixed | 20.42 | 12.11 | 0.186 | -0.896 | 0.371 |
| Alternative workshift | 22.14 | 12.29 | ||||
| Depersonalization | Fixed | 6.21 | 5.83 | 1.437 | -2.081 | 0.039 |
| Alternative workshift | 8.25 | 6.37 | ||||
| Personal accomplishment | Fixed | 24.4 | 12.89 | 0.002 | -1.54 | 0.125 |
Table 6: Burnout comparative investigation with emphasis on work shifts.
Table 7 represents job burnout ratio among work experience; due to the amount of F there is no significant difference between two element of job burnout: emotional exhaustion, depersonalization with various levels of work experience (less than 10 years, between 10 to 20 years, more than 20 years). But there is a significant difference between “personal accomplishment” and averages in levels of work experience (p>0.05); and staff with work experience between 10 to 20 years, less than 10 years, more than 20 years respectively feel more personal accomplishment.
| Variable | Levels | Average | SD | F | Significance level |
|---|---|---|---|---|---|
| Emotional exhaustion | <10 | 21.07 | 12.43 | 1.907 | 0.151 |
| 20-Oct | 23.5 | 12.31 | |||
| >20 | 18 | 9.76 | |||
| Depersonalization | <10 | 7.21 | 5.9 | 2.03 | 0.134 |
| 20-Oct | 8.83 | 6.86 | |||
| >20 | 6.56 | 5.74 | |||
| Personal accomplishment | <10 | 25.02 | 12.78 | 4.526 | 0.012 |
| 20-Oct | 29.56 | 12.59 | |||
| >20 | 21.56 | 14.48 |
Table 7: Burnout comparative investigation with emphasis on work experience (year).
Table 8 investigate the averages of job burnout elements with musculoskeletal disorders in past 12 months, demonstrates that elbow in level of 0.05%, and shoulders in level of 0.01% have a significant difference with depersonalization.
| Organ | Emotional exhaustion | Depersonalization | Personal unaccomplishment | |||
|---|---|---|---|---|---|---|
| Amount of F | Significance level | Amount of F | Significance level | Amount of F | Significance level | |
| Neck | 0.942 | 0.58 | 0.983 | 0.491 | 0.764 | 0.853 |
| Shoulders | 0.936 | 0.593 | 1.126 | 0.316 | 1.757 | 0.006 |
| Elbow | 1.142 | 0.268 | 1.688 | 0.026 | 1.291 | 0.126 |
| Wrist and hand | 0.922 | 0.616 | 0.755 | 0.794 | 0.975 | 0.524 |
| Back | 1 | 0.482 | 0.772 | 0.774 | 1.103 | 0.322 |
| Lower back | 1.122 | 0.294 | 1.221 | 0.224 | 0.847 | 0.738 |
| Hip and thighs | 0.903 | 0.65 | 0.881 | 0.632 | 0.904 | 0.945 |
| Both knees | 0.845 | 0.746 | 1.043 | 0.415 | 0.944 | 0.575 |
| Both legs | 0.884 | 0.681 | 1.089 | 0.358 | 0.88 | 0.684 |
Table 8: Burnout comparative investigation with staffs’ musculoskeletal disorders in 12 passed months.
Table 9 represents the comparative investigation between demographic features and musculoskeletal disorders in past 12 months. AS the results showed, neck and ‘married’ in maritual status have significant relationship in level 0.05%. Shoulders with employment status and number of children in 0.05% and with marital status in 0.01% have significant difference. Elbow with marital status in 0.01%, wrist and hand with marital status in 0.05%, back with age, employment and economic status in 0.05% and with marital status and number of children in 0.01%, lower back and age in 0.05% and with marital status, number of children and work experience in 0.01% has significant difference.
| Organ | Age | BMI | Employment status | Mrrital status | Child NO. | Education | Shift work | Economical level | Work rate | Over time | Work antecedent |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Neck | 1.128 | 0.675 | 1.791 | 3.995 | 1.717 | 1.122 | 0.046 | 0.368 | 1.45 | 1.242 | 1.468 |
| Shoulders | 1.111 | 1.013 | 2.853* | 5.540** | 3.734* | 1.454 | 0.093 | 2.042 | 1.920** | 0.994 | 1.206 |
| Arm | 0.925 | 0.587 | 0.769 | 5.787** | 1.002 | 0.56 | 2.122 | 2.359 | 1.391 | 1.012 | 1.079 |
| Hand and wrist | 1.337 | 1.565 | 0.099 | 4.312* | 0.452 | 0.59 | 2.898 | 1.421 | 0.846 | 0.52 | 0.913 |
| Back | 1.625* | 1.066 | 3.206* | 6.524** | 4.793** | 0.414 | 0.358 | 3.584* | 1.197 | 0.957 | 1.491 |
| Low back | 1.560* | 0.668 | 1.176 | 5.385** | 7.808** | 1.164 | 0.701 | 1.861 | 0.838 | 1.461 | 1.851** |
| Hip and thighs | 1.191 | 0.391 | 0.729 | 0.234 | 0.455 | 0.569 | 0.507 | 1.642 | 1.199 | 0.786 | 0.845 |
| Both knees | 0.862 | 0.993 | 1.072 | 1.402 | 0.282 | 0.321 | 0.008 | 0.294 | 1.303 | 0.881 | 1.029 |
| Both feet | 1.219 | 0.639 | 0.191 | 0.108 | 1.352 | 1.361 | 0.102 | 0.886 | 1.093 | 1.456 | 1.788 |
Table 9: Comparative investigation between demographic features and musculoskeletal disorders in past 12 months, *: Meaning level of 0.05 **: Meaning level of 0.01.
Table 10 shows the amount of job burnout due to the element of neck disorders. According to the amount of F factor, there was no significant difference between two elements of job burnout (personal inadequacy and depersonalization) due to different levels of neck (yes, and no).But in the element of emotional exhaustion there is a significant difference due to gained averages in levels of neck (p>0.05). Staff with average of more pain in neck feels emotional exhaustion more.
| Variable | Answers | Average | Deviation | F | Meaning fullness |
|---|---|---|---|---|---|
| Emotional exhaustion | No | 20.13 | 12.12 | 4.098 | 0.044 |
| Yes | 23.42 | 12.21 | |||
| Depersonalization | No | 7.17 | 5.97 | 2.178 | 0.141 |
| Yes | 8.4 | 6.58 | |||
| Personal unaccumplishment | No | 25.32 | 13.05 | 1.747 | 0.188 |
| Yes | 27.62 | 12.99 |
Table 10: Comparative investigation of job burnout with emphasis on neck.
According to the gained amount of F factor there was no significant difference in job burnout items (emotional exhaustion, personal unaccomplishment and depersonalization) due to body elements’ (shoulders, lower back, wrist and hand) levels: yes, or no.
Discussion
There was a significant difference in amount of depression between single and married individuals in this investigation which was sympathetic with the investigation of Khamseh et al. [32]. Since the results showed, the depression of emergency staff has a positive relation with pain around their neck. Although the individuals don’t feel and take care about this pain, but if the pain gets chronic, it would influence their work moralethus would make them boring and tired [33]. Injustice in organizations will have affected their job stress and also would be effective on the incidence of depression. On the other hand, job satisfaction may be affected by financial satisfaction. The staff with higher job situations (e. g. managers and physicians) have lower physical pressures because of their job nature and financially supported, also will keep them away from injustice as in results they feel more job satisfaction that would cause less job burnout. All the staff working in emergency have more anxity because of their job nature [34].
Result showed that individuals with different employment status suffer from various stages of job burnout that shows the effect of job security on this subject. In other words, the higher job security, the less job burnout gets. Pompeii et al. [35] in a study on hospital staff in 2009 showed that 40% of physical damages arise because of picking up things and hand moving patients which could be done easier by instruments. Also 32% of damages happen by rotating or replace or tacking patients up to their beds. So using instruments to move patients and things is advised. The results of the investigation show that MSDs’ signs are more prevalent between emergency staff. During 12 passed months, 84% of studied staff had MSDs’ signs atleast in one of nine studied organs.
Lower Back Pain (LBP) was the most prevalent musculoskeletal discomfort between studied staff (65.2%) which is the same between nurses and health care personnel’s. The results of present study and mentioned studies showed that work related LBP and neck disorders are the most prevalent. It seems that educational intervention is necessary for emergency staff. Also the results showed that there is a significant relationship between age, and work experience with prevalent of MSDs’ signs in last year at least in one of nine studied organs. Age is one of the effective factors in increase of prevalent of MSDs’ sign, as the older age, the most probability it has. The results of present study are sympathetic with the study of Choobineh et al. [36] in ergonomic risk assessment of MSDs on a sugar factory. They have represented that older staff reports more MSD signs.
In the study of [37] has been proved that there is a significant relationship between age and prevalent of MSDs’ signs. The more work experience increases the exposure to MSD risk factors. The results of the study of Choobineh et al. [36] in ergonomic risk assessment of MSD with QEC in a suger factory showed the increase of MSD symptoms on the workers with more work experience. There was no significant relationship between height and weight with prevalent of MSD signs during last year atleast in one of nine studied organs. Marras [37] mentioned MSDs affected with the individual factors. In the investigation of musculoskeletal risk factors on 1162 Japanese nurses during a year long, results showed that prevalent of these disorders in shoulders is 71.9%, lower back is 71.3%, neck is 57.7% and in upper back is 33.9% which is sympathetic with current study [38]. In the study presented by Trinkoff et al. [39] on 1163 nurses, reported the amount of musculoskeletal prevalence in neck, shoulders and lower back as: 1.8%, 35.45%, 47% respectively in which is not sympathetic with current study.
In the investigation of Abedini et al. [40] that was about health care staff and nurses’ musculoskeletal disorders, most of the participants reported lower back pain (71.5%), leg pain (68.2%), wrist and hand pain (64.5%), and neck pain (42.2%), that is not similar to current investigation. Mäntyselkä et al. [41] reported that repetitive pain in shoulders and neck is the cause of depression in adults. The study by Haghdoost et al. [42] resulted that 81% of participants had LBP at least once in last year, 29.5% had pain in wris, 50% pain on neck; 35% had pain on shoulders, and 63.5% had pain on knee that is not sympathehtic with current study. Also Blozik et al. [43] explained that incidence of anxiety and depression has a significant relation with increase of pain in neck. Many epidemiological studies had shown that activities which needs frequent changes on body posture, picking up heavy loads, bendings and frequent twists can cause lower back pain because body is not balanced and the pressure is mostly on lower back. People who work in emergencies and ICUs are facing bigger chance of getting lower back pain because of their job’s special circumstances [44]. Also they would face decrease in their work power, sleep duration and cause mental pressure because of irregular shifts at morning, noon and night and irregular asleep and awake rhythm [45]. Anyway there are not many studies about health care staff and technicians, and their workplace and its connection with frequency of musculoskeletal disorders.
The wide range of risk factors of MSDs in EMS personnel also shows complex and numerous causes. EMS job related factors such as bending, patients transferring, picking up and moving things, raising hands higher than shoulders for long time, and long stressful driving, and also physical pressures like picking up heavy loads, undesirable posture, static status, repetitive motions, applying force by hands and fingers and intense physical effort, increase in physical activities in shift works, obesity, age and sex are most important musculoskeletal disorders factors. It means, in first step, corrective actions must be done to control ergonomic risk factors of these parts of the body.
Beau-doing in his study reports that nurses and EMS personnel’s’ job is one of the most important parts of the health and treatment team of the health care system and subsequently they are under different mental and physical pressure that work compaction in all day can be its reason however they are responsible to take care of such duties simultaneously in all working days which may cause carelessness to the safety manners during work time and subsequently cause musculoskeletal disorders. In the other hand according to gender have to response to their family and personal activities thus this damages and exhaustions caused by their job can affect their emotional behavior in family and their activities and in accordance to it may cause reduction in life quality and even reluctance to their daily activities like sports or etc [46].
The findings gained from this study shows that most of the Mazandaran’s EMS’s personnel report medium levels of frequency and severity in emotional exhaustion and personal accomplishment and seveir levels of depersonalization. To confirm the findigs of this investigation we can refer to the studies of [47,48] Khatibian et al. [18] in Hamedan that also reported medium level of frequency and severity of job burnout. Franca et al. [49] and Cicchitti’s et al. [50] showed higher level of job burnout in pre-EMS staff. To correspond the investigations in other health care areas we can refer to studies of Momeni et al. [51], in Mashhad’s hospital staff [52], Soleimani et al., in health care staff of Roozbeh hospital [53,54] that all shows medium or higher job burnout in staff. In the present study 19.6% of staff had depersonalization that is 2.4 times more than Talaeei’s study [52].
Lopez et al. [55] reported higher emotional exhaustion and depersonalization in and lower personal accomplishment, in which the dimensions of depersonalization was sympathetic with this investigation. In the study of Bernard et al., on 101 nurses, reported medium level of emotional exhaustion and depersonalization and lower personal accomplishment as emotional exhaustion’s dimention is closed to present study [56]. Finding of such studies were not similar or sympathetic to this investigation. For example, Miraabzadeh Ardakani et al., reported slight level of job burnout in Razi hospital staff which it was more severe among health care staff in comparison of office workers [57].
Cicchitt et al. [50] found that the level of job burnout in pre-EMS nurses was lower than EMS nurses. Also in França et al., in 2011, showed that pre-EMS staff had reported high level and severity of job burnout elements. It should be mentioned that the difference in this study, are becase of cultural and general differences in the mentioned investigation [58].
The causes of job burnout in pre-EMS staff are such as: hard circumstances of work, working in an unsafe place, high work load, continus work shifts and 48-hours shifts, low income, doing no sports, lack of recreational facilities, non EMS duties, lack of job security because of employment status, direct connection with most of the hospital units like general practitionars and specialists, cops, all of the health care units and etc, the ambiguity of the role and defects in the duties of the staff, the weak support by the managers, low job opportunities for promotion, feeling lack of progress and etc. Burn out has undesireable effects on work satisfactory and it would cause impressive drop in quality of given services [59]. Generally, pre-EMS staff had high level of severity in depersonalization and medium in emotional exhaustion and lack of personal fatigue.
Conclusion
As there is no complete and regular education in using body parts in correct ways at works and because of lack of retraining courses for nurses, supervisors, health care staff and other groups more musculoskeletal disorders can occure; so educational programs and retraining courses for staff and managers seems essential to learn how to use correcting solutions. Due to high prevalence of MSDs in the participated population, ergonomic interventions, performing occupational health solutions, seat adjustment during car driving, setting work and rest hours along the work, minimizing repetition of movements by reducing the work speed, appropriate nutrition diets, increasing diversity in work positions and adopting appropriate physical conditions during work, perform regular exercise and sport activities to prevent and mitigate disorders seems essential. At the end it is suggested to the managers and humanitarian planners to help these staff with their job damages by increasing the number of workers and setting the work-hour especially for EMS personnel. Also it is suggested to pay attention to the organizational justice and take care of their income, so, try to increase the motivation of the employees to the desired level.
References
- Barzideh M, Choobineh A, Tabatabaee H (2014) Job stress dimensions and their relationship to musculoskeletal disorders in Iranian nurses. Work 47: 423-429.
- Smith DR, Mihashi M, Adachi Y, Koga H, Ishitake T (2006) A detailed analysis of musculoskeletal disorder risk factors among Japanese nurses. J Safety Res 37: 195-200.
- Burdorf A, Sorock G (1997) Positive and negative evidence of risk factors for back disorders. Scandinavian J Work Environ Health 243-256.
- Li G, Buckle P (1999) Current techniques for assessing physical exposure to work-related musculoskeletal risks, with emphasis on posture-based methods. Ergonomics 42: 674-695.
- Punnett L, Wegman DH (2004) Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyography Kinesiology 14: 13-23.
- Bulduk EÖ, Bulduk S, Süren T, Ovali F (2014) Assessing exposure to risk factors for work-related musculoskeletal disorders using Quick Exposure Check (QEC) in taxi drivers. Int J Industrial Ergonomics 44: 817-820.
- Van Rijn RM, Huisstede BM, Koes BW, Burdorf A (2010) Associations between work-related factors and specific disorders of the shoulder: A systematic review of the literature. Scandinavian J Work Environ Health 2010: 189-201.
- Bongers P, Ijmker S, Van den Heuvel S, Blatter B (2006) Epidemiology of work related neck and upper limb problems: psychosocial and personal risk factors (part I) and effective interventions from a bio behavioural perspective (part II). J Occupational Rehabilitation 16: 272-295.
- Durmus D, Ilhanli I (2012) Are there work-related musculoskeletal problems among teachers in Samsun, Turkey? J Back Musculoskeletal Rehabilitation 25: 5-12.
- Hughes LE, Babski-Reeves K, Smith-Jackson T (2007) Effects of psychosocial and individual factors on physiological risk factors for upper extremity musculoskeletal disorders while typing. Ergonomics 50: 261-274.
- Menzel NN (2007) Psychosocial factors in musculoskeletal disorders. Critical Care Nursing Clinics of North America 19:145-53.
- Devereux J (1999) Work-related neck and upper limb: musculoskeletal disorders: European Agency for Safety and Health at Work.
- Widanarko B, Legg S, Devereux J, Stevenson M (2015) Interaction between physical and psychosocial work risk factors for low back symptoms and its consequences amongst Indonesian coal mining workers. Applied Ergonomics 46: 158-167.
- Mollart L, Skinner VM, Newing C, Foureur M (2013) Factors that may influence midwives work-related stress and burnout. Women Birth 26: 26-32.
- Akkasheh G, Sepehrmanesh Z, Ahmadvand A (2010) Prevalence of burnout in senior medical students of Kashan University of Medical Sciences in 2008. Qom University of Med Sci J 4: Pe37-Pe41.
- Torres V, Galbraith CS, Merrill GB (2012) Academic and work-related burnout: A longitudinal study of working undergraduate university business students. Journal of College Student Development 53: 453-463.
- Borritz M, Christensen KB, Bültmann U, Rugulies R, Lund T, et al. (2010) Impact of burnout and psychosocial work characteristics on future long-term sickness absence. Prospective results of the Danish PUMA Study among human service workers. J Occupational Environ Med 52: 964-970.
- Khatibian M, Hosseini S, Baikmradi A, Roshanaei GH (2012) Burnout in medical emergency personnel. The Scientific J Hamadan Nursing Midwifery Faculty 20: 5-11.
- Moshtagh Eshgh Z, Peyman A, Amirkhani A, Taghinejad F (2014) The relationship between occupational stresses with job burnout in pre-hospital emergency staff. Jorjani 2: 33-41.
- Moradi Z, Eslami AA, Hasanzadeh A (2015) Job burnout status among pre-hospital emergency technicians. Iranian J Emergency Medicine 2: 28-32.
- Masoudi R, Etemadifar S, Afzali M, Kheiri F, Ali H (2008) Factors that affecting burnout among nurses working in private hospitals in Tehran. Nursing Research J 3: 47-58.
- Mahmoudi G, Rouhi G, Mojerlu M, Sheikh H, Rahmani H (2006) The relationship between nurses’ burnout with Physical conditions and specialized facilities of work place. Gorgan University of Medical Sciences J 8: 40-46.
- Honkonen T, Ahola K, Pertovaara M, Isometsä E, Kalimo R, et al. (2006) The association between burnout and physical illness in the general population-results from the Finnish Health 2000 Study. J Psychosomatic Research 61: 59-66.
- Langballe EM, Innstrand ST, Hagtvet KA, Falkum E, Gjerløw Aasland O (2009) The relationship between burnout and musculoskeletal pain in seven Norwegian occupational groups. Work 32:179-188.
- Sorour AS, El-Maksoud MMA (2012) Relationship between musculoskeletal disorders, job demands, and burnout among emergency nurses. Advanced Emergency Nursing J 34: 272-82.
- Eelen S, Bauwens S, Baillon C, Distelmans W, Jacobs E, et al. (2014) The prevalence of burnout among oncology professionals: Oncologists are at risk of developing burnout. Psycho-Oncology 23: 1415-1422.
- Abdulghafour, Yasmin A, Bo-Hamra, Anwar M, Al-Randy, et al. (2011) Burnout Syndrome among Physicians Working in Primary Health Care Centers in Kuwait. Alexandria J Medicine 47: 351-357.
- Sotodeh AN, Bakhtiari AH (2006) Occupational exhaustion and its related factors in nurses and midwives of Semnan University of Medical Sciences. Scientific J Kurdistan University Med Sci 11: 77-83.
- Escribà-Agüir V, Martín-Baena D, Pérez-Hoyos S (2006) Psycho-social work environment and burnout among emergency medical and nursing staff. Int Archives Occupational Environmental Health 80: 127-133.
- Bos J, Mol E, Visser B, Frings-Dresen M (2004) Risk of health complaints and disabilities among Dutch firefighters. Int Archives of Occupational Environ Health 77: 373-382.
- Harkin M, Melby V (2014) Comparing burnout in emergency nurses and medical nurses. Clin Nurs Stud 2: 152-163.
- Khamseh F, Rouhi H, Ebady A, Hajiamini Z, Salimi H, et al. (2011) Survey relationship between demographic factors and stress, anxiety and depression in nurses working in selected hospitals in tehran city. J Holist Nurs Midwifery 21: 13-21.
- Sharifnia S, Haghdoust A, Ghorbani M, Haji Hf, Nazari Roghayeh Hh, et al. (2010) The relationship of low back pain with psychosocial factors and psychological stress in nurses in amol hospitals. Knowledge Health 4: 27-33.
- Mardani Hamooleh M, Ebrahimi E, Mostaghasi M, Taghavi Larijani T (2013) Relationship between organizational justice and job stress among hospital personnel. Iranian J Medical Ethics and History of Medicine 6: 64-71.
- Pompeii LA, Lipscomb HJ, Schoenfisch AL, Dement JM (2009) Musculoskeletal injuries resulting from patient handling tasks among hospital workers. American J Industrial Med 52: 571-578.
- Choobineh AR, Tabatabaei H, Behzadi M (2009) Musculoskeletal problems among workers of an Iranian sugar-producing factory. Int J Occup Saf Ergon 15: 419-24.
- Ferguson SA, Marras WS (1997) A literature review of low back disorder surveillance measures and risk factors. Clin Biomech 12: 211-226.
- Smith DR, Mihashi M, Adachi Y, Koga H, Ishitake T (2006) A detailed analysis of musculoskeletal disorder risk factors among Japanese nurses. J Safety Res 37:195-200.
- Trinkoff AM, Lipscomb JA, Geiger-Brown J, Brady B (2002) Musculoskeletal problems of the neck, shoulder, and back and functional consequences in nurses. American J Industrial Med 41: 170-178.
- Abedini R, Choobineh A, Hasanzadeh J (2013) Ergonomics Risk Assessment of Musculoskeletal Disorders Related to Patient Transfer Operation among Hospital Nurses Using PTAI Technique Iran J Nursing 25: 75-84.
- Mäntyselkä P, Lupsakko T, Kautiainen H, Vanhala M (2010) Neck-shoulder pain and depressive symptoms: A cohort study with a 7-year follow-up. European J Pain 14: 189-193.
- Haghdoost AA, Hajihosseini F, Hojjati H (2011) Relationship between the musculoskeletal disorders with the ergonomic factors in nurses. Koomesh 12: 372-378.
- Blozik E, Laptinskaya D, Herrmann-Lingen C, Schaefer H, Kochen MM, et al. (2009) Depression and anxiety as major determinants of neck pain: A cross-sectional study in general practice. BMC musculoskeletal disorders 10: 13.
- Fege AM, Herbison P (2000) The role of physical and psychological factors in occupational low back pain: a prospective cohort study. Occupational Environmental Medicine 57: 116-20.
- Jebreily M (2004) Survey of the sleep deprivation on quality of nurses' work and its solution plans. Iranian J Med Sci 3: 6-4.
- Burdorf A, Sorock GS (1997) Positive and negative evidence of risk factors for back disorders. Scandinavian J Work Environ Health 23: 243-256.
- Moradi Z, Eslami1 AA, Hasanzadeh A (2015) Job Burnout status among Pre-Hospital emergency technicians. Iranian J Emer Med 2: 28-32.
- Ebrahimi H, Navidian A, Ameri M, Sadeghi M (2014) Burnout, dimensions and factors related to the operational staff and emergency medicine. Health Promotion Management J 3: 16-26.
- França S, Martino M (2014) Current correlations of stress and burnout in the work of pre-hospital nursing. J Nursing 8: 4221-4228.
- Cicchitti C, Cannizzaro G, Rosi F, Maccaroni R, Menditto VG (2014) Burnout syndrome in pre-hospital and hospital emergency. Cognitive study in two cohorts of nurses. Recent Progress in Medicine 105: 275-280.
- Momeni H, Salehi A, Seraji A (2009) The Comparison of Burnout in nurses working in clinical and educational sections of Arak University of Medical Sciences in 2008. Arak Medical University J 12: 113-123.
- Talaei A, Mokhber N, Mohammad Nejad M, Samari A (2008) Burnout and associated factors among employees of university hospitals in Mashhad in 2006. Koomesh 9: 237-245.
- Soleimani K, Sharifi V, Tehrani Dost M (2005) Burnout in staff Roozbeh psychiatric hospital. New Cognitive Sci 7: 36-42.
- Moghadasi J, Aslani Y, Etemadifar Sh, Masoudi R Ravaghi K (2012) Burnout in nurses working in chronic disease care medical centers. University Hospitals Jundishapur 1: 25-35.
- Lopez FM, Rodriguez NA, Fernandez SM, Marcos AS, Martinon TF, et al. (2005) Burnout syndrome among health workers in pediatrics. An Pediatr (Barc) 62: 248-251.
- Barnard D, Street A, Love AW (2006) Relationships between stressors, work supports, and burnout among cancer nurses. Cancer Nurs 29: 338-45.
- Mirabzadeh Ardakani A, Samii M, Faizzade G, Irani Sh (2007) Burnout and related factors on hospital staff Razi Psychiatric. Iranian Rehabilitation J 8: 64-70.
- França SPDS, De Martino MMF, Aniceto EVdS, Silva LL (2012) Predictors of burnout syndrome in nurses in the prehospital emergency services. Acta Paul Enferm 25: 68-73.
- Delpasand M, Raeissi P, Begdeli F, Shahabi M (2011) The impact of job rotation on nurses’ burnout in Ayatollah Kashani hospital, Tehran: A case study. Iran Occup Health 7: 1-12.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi