Case Report, Jrgm Vol: 9 Issue: 1
Intradiscal Injection of Dehydrated Human AmnionChorion Membrane for Treatment of Chronic Discogenic Low Back Pain: A Case Series
Sean A. Lacey1*, Steven P. Cohen2 and Michael B. Jacobs3
1Walter Reed National Military Medical Center, 8901 Rockville Pike, Bethesda, MD 20889
2Johns Hopkins Hospital, 1800 Orleans St, Sheikh Zayed Tower, Baltimore, MD 21287
3Uniformed Services University of the Health Sciences, 4301 Jones Bridge Rd, Bethesda, MD 20814
*Corresponding Author: Sean A. Lacey, Lake Erie College of Osteopathic Medicine, Walter Reed National Military Medical Center, Bethesda, USA E-mail: sean.lacey.do@gmail.com
Received: January 30, 2020 Accepted: March 17, 2020 Published: March 24, 2020
Citation: Lacey SA, Cohen SP, Jacobs MB (2020) Intradiscal Injection of Dehydrated Human Amnion Chorion Membrane for Treatment of Chronic Disco genic Low Back Pain: A Case Series. J Regen Med 9:1.
Abstract
Discogenic Low Back Pain (DLBP) is a common condition with an unfavourable prognosis and limited treatment options. After experiencing insufficient response to standard conservative care of physical therapy, non-steroidal anti-inflammatory medications andactivity modification, three patients with chronic DLBP were treated with intradiscal injection of dehydrated Human Amnion Chorion Membrane (dHACM). Diagnosis was established by Magnetic Resonance Imaging (MRI) revealing disc disease with anatomically concordant pain.results indicated a trend toward reduced pain as measured by the Numerical Rating Scale for pain (NRS-Pain) and increased function as measured by the Oswestry Disability Index (ODI).
Keywords: Regenerative medicine; Chronic pain; Low back pain; Interventional pain; Dehydrated human amnion chorion membrane
Keywords
Regenerative medicine; Chronic pain; Low back pain; Interventional pain; Dehydrated human amnion chorion membrane
Disclaimer
The views expressed are solely those of the authors and do not reflect the official policy or position of the US Army, US Navy, US Air Force, the Department of Defence, or the US Government.
Dehydrated Human Amnion Chorion Membrane
Chronic low back pain is a major cause of morbidity worldwide, with a global prevalence of 0.5 billion and a contribution of 57.6 million disability adjusted life years [1].Further, low back and neck pain prevalence and disability have increased over the past 25 years with the aging population [1].In addition, among the U.S. military population, back-related conditions have been associated with the highest 5-year cumulative risk of disability discharge [2].
Patients with low back pain and intervertebral disc lesions identified on advanced imaging or discography are often diagnosed with “discogenic low back pain” (DLBP), which has a prevalence rate among axial low back pain sufferers estimated at 39 to 42% [3].
Typical treatments for chronic low back pain have varied from initial treatment with physical therapy, anti-inflammatory medications, acupuncture, cognitive behavioural therapy, spinal manipulative therapy and activity modifications [4].Some patients eventually opt for surgical treatment to include spine fusion and arthroplasty. Despite these treatments, the prognosis for DLBP is not favourable, with one prospective clinical study containing 279 patients finding that 87% of patients continued to have symptoms at 4 years of follow-up [4,5].
Recently, regenerative medicine techniques, which aim to restore or improve function potentially through the regeneration of injured tissues, have been explored by investigators in a multitude of clinical settings. However, there is limited evidence for the use of these techniques in the treatment of chronic low back pain. One of these products, dehydrated human-amnion chorionic membrane (dHACM), has been used in ophthalmology, plastic surgery and dermatology, with recent studies exploring its use is musculoskeletal medicine [6]. In 2013, Bhattacharya, et al. published a randomized prospective cohort study which demonstrated statistically significant improvements in visual analog pain scale and walking distance in meters in patients treated with C-arm guided intradiscal injection of amniotic fluid as compared to intradiscal long acting steroids [7].
The basis for the clinical application of dHACM lies in the physiology, anatomy and cell biology of development. During development of the fetus, part of the amniotic membrane (AM) differentiates into the bilaminar embryonic disc, which gives rise to ectoderm, endoderm and mesoderm. This pluripotency of the AM during development underlies the proposed ability of dHACM to stimulate differentiation of stem cells into specific tissues when injected into the body. AM has been demonstrated to provide a matrix for cellular migration and proliferation; provide anti-inflammatory, antimicrobial and analgesic effects; enhance wound-healing; serve as a natural biologic barrier; and has been shown in cell culture studies to be pluripotent, with one study documenting differentiation into a tenocyte phenotype when co-cultured with tenocytes [6,8,9].In vitro and in vivo experiments have established that dHACM contains one or more soluble growth factors capable of stimulating mesenchymal stem and progenitor cell migration and recruitment [9].These mechanisms could theoretically be leveraged to improve pain and function in patients with chronic DLBP. To that end, some physicians have begun using dHACM as an off-label treatment for chronic DLBP for patients who have not responded favourablyto standard-of-care treatments. While this drug is FDA approved, it has not yet been evaluated for use in treatment of chronic DLBP.
The purpose of this report is to provide further preliminary cases of patient response to the use of dHACM as a treatment for chronic DLBP. All data presented in the article was gathered retrospectively
Case Description
Case 1: A 36-year-old female active duty National Guard officer with a history of post-traumatic stress disorder presented with a 6-year history of non-radiating low back pain following a lifting injury. Her pain was not significantly improved despite conservative treatment that included medications, several integrative therapies, and spine injections. Her pain was worse with sitting or strenuous activities and improved with rest. The pain intensity was rated from 2-8/10.
Case 2: A 48-year-old female dependent of a military service member presented with a 7-year history of axial low back pain associated with paresthesias in her feet and mid-anterior thighs bilaterally. Her pain was described as a continuous, dull ache made worse by lumbar flexion, sit-ups, and prolonged sitting. The pain did not improve with medications, physical therapy, or multiple spine injections. Neurosurgery recommended against operative management.
Case 3: A 37-year-old male active duty Marine presented with a long history of intermittent low back pain with occasional radiation into his left anterior thigh. His pain was rated as 9/10 severity. The pain was worse with prolonged sitting and relieved by lying flat. His pain was refractory to conservative care including physical therapy, integrative medical treatments, and multiple procedural interventions
Investigations
Case 1: Physical examination was significant for pain with forward bending and diffuse tenderness to palpation of the lumbar paraspinal muscles, without neurological abnormalities. Lumbar spine MRI revealed a disc bulge and facet disease at the L5-S1 level (Figure 1), with the disc height approximately 50% of normal. The patient was given a presumptive clinical diagnosis of L5-S1 DLBP

Figure 1: T2 weighted sagittal lumbar MRI demonstrating disc bulge and facet disease at L5-S1.
Case 2: Physical exam was significant for lumbar paraspinal tenderness but without neurological deficits. MRI revealed degenerative facet and disc disease from L2/3 to L4/5 without evidence of nerve root compression (Figure 2). Discs at these affected levels showed only bulge or protrusion, and all had disc height >50% of normal. The patient declined discography and was given a clinical diagnosis of L2-L5 DLBP.
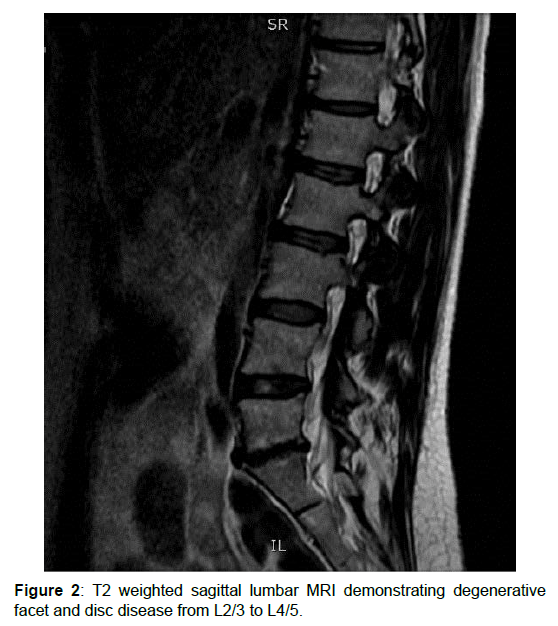
Figure 2: T2 weighted sagittal lumbar MRI demonstrating degenerative facet and disc disease from L2/3 to L4/5.
Case 3: Physical exam was significant for loss of lumbar lordosis, pain on left lateral flexion, and tenderness along the left lumbar paraspinal muscles, without focal neurological deficits. MRI showed focal disc protrusion at L5-S1, disc height at approximately 50% of normal, and moderate left lateral recess narrowing but not displacing the left S1 nerve root (Figure 3). Provocative discography supported a diagnosis of L5/S1 DLBP.

Figure 3: T2 weighted sagittal lumbar MRI demonstrating focal disc protrusion at L5-S1 without displacement of the S1 nerve root.
Treatment
All patients provided written consent and received pre-procedure intravenous antibiotics. Under fluoroscopic guidance, 22-gauge spinal needles were advanced using an extra-pedicular, double-needle approach into the affected disc. Needle position was confirmed with < 0.5 ml of contrast dye in antero-posterior and lateral views. 100 mg of dHACM (under the trade name Amniofix) reconstituted with 1.5 ml of preservative free normal saline was then injected into the affected disc(s). A lower volume was used if a firm endpoint was reached during injection. For case #2, in which 3-disc levels were treated, the 100 mg of dHACM was reconstituted in 3 ml of preservative free normal saline, with 1 ml injected into each disc. There were no complications aside from procedure-related discomfort. After the procedure, patients were instructed to discontinue nonsteroidal antiinflammatory drugs and corticosteroids for two weeks and to avoid high impact activity for four weeks. A lumbosacral orthosis was provided for 2 weeks to use when out of bed. Oral acetaminophen and tramadol were provided for post-procedure pain. No repeat lumbar spine MRI imaging was obtained.
Outcome and Follow-Up
Follow-up visits were performed at 6 weeks and 3 months after the injections, at which time Oswestry Disability Index (ODI) and 0-10 Numerical Rating Scale (NRS) “current” and “worst pain” scores were recorded. The NRS is a subjective measure in which individuals rate their pain from 0 to 10, with 0 being no pain at all and 10 being the worst pain imaginable
In this case series, three patients from a military or dependent of military service member background with DLBP received intradiscal dHACM. Results seem to indicate a trend toward decreased pain on NRS and increased function as measured by the ODI, although a larger, controlled trial would be required to determine effectiveness.
Discussion
Additional areas that warrant further investigation would include selection criteria, dosage per disc, and potential adverse effects. Our case series has obvious limitations, including its small sample size, retrospective design, lack of a control group, and its application in a unique (military) patient population. Therefore, efficacy and generalizability are not possible but are hypothesis-generating for future studies.
This case series provides documentation of the clinical response to intradiscal dHACM for treatment chronic DLBP in individuals from the military population. Multiple publications are available in the area of regenerative medicine applications for discogenic low back pain, including a prospective, double-blind, trial included 47 subjects who were randomized to receive either intradiscal platelet rich plasma (PRP) or contrast dye. Statistically significant improvements in “best” pain (P=0.02), functional rating index (P=0.03) and the North American Spine Society Outcome Questionnaire (P=0.01) were found over an 8-week period, although “current” and “worst” pain did not improve [10]. Pettine et al. performed a prospective observational study of 26 patients who received intradiscal autologous bone marrow concentrate injections. The average ODI and Visual Analog Scale scores improved from a baseline of 56.5 and 79.3, respectively, to 22.8/29.2 at 3 months, 24.4/26.3 at 6 months, and 25.0/33.2 at 12 months [11,12]. These studies, as well as the findings from our case series, suggest that regenerative treatments for DLBP warrant further investigation.
Based on our experience and in consideration of other published studies on treatments for DLBP, we postulate that certain patients are more likely to have success with intradiscal regenerative medicine injections. These would include younger individuals [13], those with preserved disc height (>50% of normal) [14,15] pain limited to 1 or 2-disc levels confirmed by discography [14,15], and an absence of high-dose opioids [16]or psychopathology [17]. Each of these factors should be studied further.
Chronic DLBP is a common condition that often results in long term disability. Interventional and surgical treatments have been shown to provide only modest benefit to a small subset of patients, and for many, the risks may outweigh the benefits. Regenerative medicine treatments, such as intradiscal injection of dHACM as noted in this small case series of patients, may help to decrease pain, improve function and possibly decrease the need for opioids or surgery in carefully selected patients. This case series provides critical preliminary knowledge and support for the use of dHACM for chronic DLBP. Randomized studies with large sample sizes are needed to identify the optimal dose regimen, refine selection criteria, and determine effectiveness.
Learning Points
-Discogenic low back pain is common condition with an unfavourable prognosis and limited treatment options.
-Regenerative medicine techniques represent an emerging area of medicine which may have applications in chronic low back pain.
-In these three patients from a military background, intradiscal injection with dHACM was associated with decreased pain on NRS and increased function as measured by the ODI.
-Randomized studies with large sample sizes are needed to investigate the potential role of dHACM in treatment of chronic DLBP.
Acknowledgements
This work was supported in part by the Uniformed Services University, Department of Physical Medicine & Rehabilitation, Musculoskeletal Injury Rehabilitation Research for Operational Readiness (MIRROR) (HU00011920011).
Conflicts of interest
None
References
- Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, et al .(2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Glob Health390:1211-1259
- Lincoln AE, Smith GS, Amoroso PJ, Bell NS (2002) The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work 18:99-113
- Manchikanti L, Benyamin RM, Hirsch JA, Falco FJ, Calodney AK, et al (2013) An update of the systematic appraisal of the accuracy and utility of lumbar discography in chronic low back pain. Pain Physician 16:55-95
- Sandbrink F, Bevevino A, Tillisch K, Konitzer L, Sall J (2017) VA/DiD Clinical Guideline for Diagnosis and Treatment of Low Back Pain. J Gen Intern Med 34:2620-2629
- Peng B, Fu X, Pang X (2012) Prospective clinical study on natural history of discogenic low back pain at 4 years of follow-up. Pain Physician 15:525-532.
- Riboh JC, Saltzman BM, Yanke AB, Cole BJ (2016) Human Amniotic Membrane-Derived Products in Sports Medicine: Basic Science, Early Results, and Potential Clinical Applications. Am J Sports Med 44:2425-2434.
- Bhattacharya N, Stubblefi P (2013) Amniotic Fluid Cell Therapy to Relieve Disc-Related Low Back Pain and Its Efficacy Comparison with Long-Acting Steroid Injection, Human FetalTissue Transplant 251-264
- Barboni B, Curini V, Russo V ( 2012) Indirect co-culture with tendons or tenocytes can program amniotic epithelial cells towards stepwise tenogenic differentiation. PLoS One 7:e30974
- Brown MN, Shiple BJ, Scarpone M ( 2016) Regenerative Approaches to Tendon and Ligament Conditions. Phys Med RehabilClin N Am 27:941-984
- Koob TJ, Rennert R, Zabek N (2013) Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J.;10:493-500.
- Tuakli-Wosornu YA, Terry A, Boachie-Adjei K (2016) Lumbar Intradiscal Platelet-Rich Plasma (PRP) Injections: A Prospective, Double-Blind, Randomized Controlled Study. PM R 8:1-10
- Pettine, KA, Murphy MB, Suzuki RK, Sand TT (2015) Percutaneous injection of autologous bone marrow concentrate cells significantly reduces lumbar discogenic pain through 12 months. Stem Cells 33:146-56
- Anderson JT, Haas AR (2015) Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers’ compensation subjects. Spine 40:748-756
- Cohen SP, Larkin TM (2005) Lumbar discography: a comprehensive review of outcome studies, diagnostic accuracy, and principles. RAPM 30:163-183.
- Pauza KJ, Howell S (2003) A randomized, placebo-controlled trial of intradiscalelectrothermal therapy for the treatment of discogenic low back pain. Spine J 4:27-35.
- Desai MJ, Kapural L (2016) A prospective, randomized, multicenter, open-label clinical trial comparing intradiscalbiacuplasty to conventional medical management for discogenic low back pain. Spine 4:1065-1074.
- Jain N, Phillips FM (2018) Pre-operative chronic opioid therapy: a risk factor for complications, readmission, continued opioid use and increased costs after one- and two-level posterior lumbar fusion. Spine 43:1331–1338.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 