Case Report, Int J Ophthalmic Pathol Vol: 11 Issue: 6
Internal Ophthalmomyiasis: A Case Report
Shams Mohammed Nomana*, Murtuza Nuruddin
Department of Ophthalmology, Eye Infirmary and Training Complex, Chittagong, Bangladesh
*Corresponding Author: Shams Mohammed Nomana Department of Ophthalmology, Eye Infirmary and Training Complex, Chittagong, Bangladesh, Tel: 1715299695; E-mail: drshams_noman@yahoo.com
Received date: 22 May, 2020, Manuscript No. IOPJ-20-11267; Editor assigned date: 27 May, 2020, Manuscript No. IOPJ-20-11267 (PQ); Reviewed date: 10 June, 2020, QC No. IOPJ-20-11267; Revised date: 30 November, 2022; Manuscript No. IOPJ-20-11267 (R); Published date: 28 December, 2022, DOI: 10.4172/2324-8599.11.6.112
Citation: Nomana SA, Nuruddin M (2022) Internal Ophthalmomyiasis: A Case Report. Int J Ophthalmic Pathol 11:6.
Abstract
Purpose: To report a rare case of unilateral internal ophthalmomyiasis with complete visual loss.
Methods: An otherwise healthy 12 years old boy presented with redness and painful rapid loss of vision in his right eye for the past 12 days. There was no history of associated trauma. On examination, there was no perception of light in his right eye and normal vision in left eye. There was severe anterior and posterior segment inflammation which prevented the view of fundus.B-scan of the right eye showed diffuse choroidal and optic nerve thickening. Routine blood count and X-ray chest did not reveal any significant findings.In the midst of uncertainity regarding diagnosis and to relieve the patient from severe pain, enucleation of right eye was performed and histopathological examination of the specimen was done to confirm the diagnosis.
Results: Histopathology report showed gross irregular inflammatory thickening of the choroid with severe granulomatous inflammation. There was an infective agent in the choroid having an outer cuticle and an irregular hyaline branching innner tube. These features were suggestive of ophthalmomyiasis of the choroid.
Conclusion: Although rare, ophthalmomyiasis should be considered in the differential diagnosis of panuveitis. Early recognition of this condition, when tumour and other conditions are suspected, would avoid invasive surgical procedures, such as enucleation.
Keywords: Ophthalmomyiasis; Enucleation; Panuveitis;
Choroid; Histopathology
Keywords
Ophthalmomyiasis; Enucleation; Panuveitis; Choroid; Histopathology
Introduction
The clinical diagnosis, treatment management, and epidemiology of a case of unilateral posterior Ophthalmomyiasis in a university farm manager are announced. Subretinal tracking was prominent, leading to vision abnormalities, which initially prompted the patient to explore medical evaluation. Identification of the organism based on study of photographs was considered to be a first-instar larva of a Cuterebra (rodent bot fly), although recognition of first-instar (stage) myiasisproducing fly larvae is impossible. Inasmuch the patient was a herdsman, it is likely that the larva is of the genus Hypoderma (cattle grub) or possibly Gasterophilus (horse bot). Laser treatment was adequately used to destroy and immobilize the organism. Subsequently, the patient's health remains satisfactory, and his vision has upgraded.
The infestation of living vertebrate animal tissues by fly larvae (maggots) is known as myiasis. Ophthalmomyiasis (Ophthalmic myiasis) is the infestation of the human eye, by the maggot of certain flies from the order of diptera [1]. Numerous different causative agents may be found, e.g., Cochliomyia macellaria, Oestrus bovis, Gastrophilus species, Hypoderma species [2]. The most common reported organism in the literature is Oestrusbovis, a boat fly highly prevalent in sheep herdening and farming. Cattle, sheep, deer and rodents are the host animal. By penetration through skin, orbit or nasal cavities, human infestation occurs. Eggs and larvae are transported to the eye surface by vectors such as ticks, mosquito’s and also by patient’s hands [3]. Less than 5% of human myiasis causes involvement of the eye. Classification of ophthalmomyiasis is based on the portion of the eye and ocular adnexa affected. External myiasis occurs in the lid and conjunctiva. Larvae within the globe is called internal myiasis. Although rare, orbital myiasis may also take place. Because of lower mechanical resistance of sclera to maggot’s penetration, ophthalmomyasis interna is more frequent in children [4]. Maggots enter or exit the eye through the sclera, blood stream or optic nerve. The larva destroys the tissues with toxins and produces protein. Proteolytic bacteria carried by maggots destroy these proteins. Enzymatic digestion, in turn provides suitable proteins for the maggot. Myiasis of the eye lid has been reported from Cutebra larva and D. hominis causing puncture of the skin and extrude ova beneath the surface or deposits their eggs on open wounds resulting furuncular, boil like lesions [5].
Case Presentation
Mr. Md. Faisal age 12 yrs. Begumgonj, Noakhali came to CEITC with the complaints of redness and loss of vision in R/E for 8 days. He had no history of trauma.On examination there was no perception of light in his right eye and 6/6 vision in his left eye.
Right eye examination also revealed oedematous lid., congested conjunctiva in a ciliary pattern, hazy and oedematous cornea. Severe inflammation with organised fibrin in the anterior chamber. Pupil was irregular with posterior synechia. Lens was cataractous posterior segment was not visible. No abnormality was detected in his left eye (Figure 1) [6].
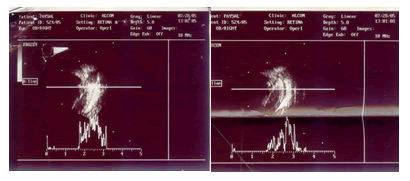
Figure 1: Image showing eye examination.
B-scan showed diffuse choroidal and optic nerve thickening. The provisional diagnosis was right sided choroidal growth with pan uveitis. He was admitted and treated conservatively. His blood picture, biochemical analysis and urine analysis was normal. Within this time he developed continuous severe pain in his right eye.
Enucleation of right eye was done as indication of painful blind eye and the globe was sent for histopathological examination (Figures 2-10) [7].

Figure 2: Rt. enucleation done and the whole globe has sent to department of histopathology of Sheffield teaching hospitals of United Kingdom.
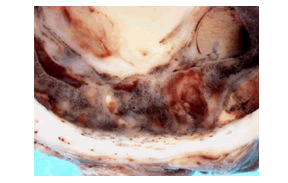
Figure 3: Macroscopic image of cut surface of eye. This shows gross irregular thickening of the choroid.
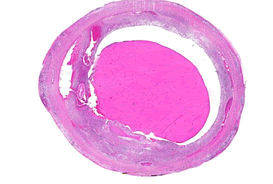
Figure 4: Low power haematoxylin and eosin (H and E) stained image of the eyeball. There is a central eosinophilic exudates and inflammatory thickening of the choroids
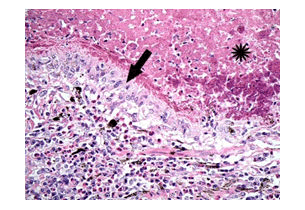
Figure 5: Higher power H and E of the choroid shows a necrotic tract (asterisk), cuffed by granulomatous inflammation (arrow).
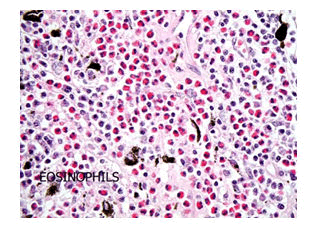
Figure 6: H and E-The granulomatous inflammation is in turn cuffed by a dense eosinophilic inflammatory response.
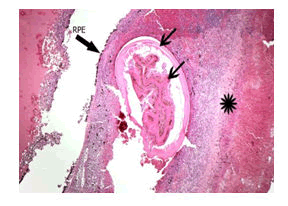
Figure 7: Low power H and E shows an infective agent in the choroid (arrowed). PE=retinal pigment epithelium.
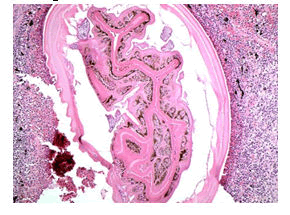
Figure 8: Higher power H and E showing an agent with an outer cuticle and an irregular hyaline branching inner tube.
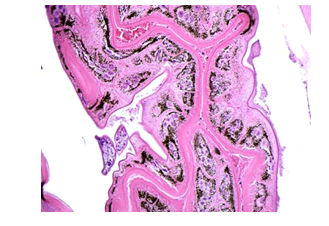
Figure 9: Higher power H and E of the inner irregular hyaline branching tube.
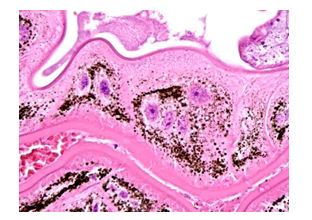
Figure 10: The lining cells of the inner tube are multinucleate and contain brown pigment.
Results and Discussion
According to histopathological evidence, the patient was diagnosed as Ophthalmomyiasis of choroid (The exact genus and species of the fly is not ascertainable). Ophthalmic reactions to maggots have different types. The larva may remain in the eye without inducing significant inflammation. After the death of maggots it may cause mild uveitis or severe inflammation. Usually, inflammation is painless but in our case it caused painful severe panuveitis. Criss-cross pattern faint curvilinear grey white line secondary to disturbed retinal pigment epithelium is pathognomec. This sub retinal track is called railroad track [8].
Visual loss may be the result of severe inflammation and extension of railroad tracks through the macula, retinal detachment, haemorrhage or invasion of the optic nerve. In our case visual loss may be due to severe panuveitis and optic nerve involvement. Due to severe inflammation thorough intraocular examination and photography was not possible [9-12].
Conclusion
Management depends upon the location of the maggot and severity of inflammation. A maggot within the vitreous cavity with mild or no inflammation could be left alone. Steroid therapy is indicated in case of mild to moderate uveitis. Photocoagulation of subretinal maggots should be performed promptly to prevent further decrease in vision due to continued tunneling. Parsplana vitrectomy can be performed.
Removal of larva from anterior chamber by aspiration or with forcep.
In case of external ophthalmomyiasis, normal forcep removal of the larvae is ideal. Ophthalmic ointment or ethyl ether can be used to block the larvae’s respiratory pore, thereby suffocating the organism to facilitate manual removal. Although rare, ohthalmomyiasis may be presented as panuveitis. Early recognition with a detailed external and internal ophthalmic examination is necessary to save the eye with early appropriate treatment.
References
- Ziemianski MC, Lee KY, Sabates FN (1980) Ophthalmomyiasis interna. Archiv Ophthalmol 98: 1588-1589.
- Doxanas MT, Walcher JR, Ludwig RA (1992) Ophthalmomyiasis externa: A case report. Maryland Med J 41: 989-991.
- Mason GI (1981) Bilateral ophthalmomyiasis interna. Am J ophthalmol 91: 65-70.
- Vine AK, Schatz H (1981) Bilateral posterior ophthalmomyiasis. Ann Ophthalmol 13: 1041-1043.
- Jakobs SM, Adelberg DA, Lewis JM (1997) Ophthalmomyiasis interna posterior, report of a case with optic atrophy. Retina 17: 310-314.
- Helmut Beuttmer, MD (2002) Ophthalmomyiasis Interna Arch ophthalmology 120: 598-1599.
- Noman SM, Nuruddin M (2021) A case history of internal ophthalmomyiasis, a rare and devastating disease. Int J Ophthalmol Visual Sci 6: 154.
- Huynh N, Dolan B, Lee S, Whitcher JP, Stanley J (2005) Management of phaeniciatic ophthalmomyiasis externa. Br J Ophthalmol 89: 1377-1378.
- Laborde RP, Kaufman HE, Beyer WB (1988) Intracorneal ophthalmomyiasis. Case report. Arch Ophthalmol 106: 880-881.
- Perry HD, Donnenfeld ED, Font RL (1990) Intracorneal ophthalmomyiasis. Am J Ophthalmol 109: 741-742.
- Newman PE, Beaver PC, Kozarsky PE, Waring GO (1986) Fly larva adherent to corneal endothelium. Am J Ophthalmol 102: 211-216.
- Spirn MJ, Hubbard GB, Bergstrom C, Harris L, Aaron MM, Broocker G (2006) Ophthalmomyiasis associated with Fuchs heterochromic iridocyclitis. Retina 26: 973-974.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi 