Review Article, J Spine Neurosurg Vol: 12 Issue: 2
Hindi Translational and Modification of Modified JOA for Cervical Myelopathy and its Validation for Indian Population
Nishant Nishant*
Department of Spine Services, Rameshwaram Orthopedic and Spine Clinic, Patna, India
*Corresponding Author: Nishant Nishant
Department of Spine Services, Rameshwaram Orthopedic and Spine Clinic, Patna, India
Tel: 919560265449
Email: nishantspine@gmail.com
Received date: 17 March, 2022, JSNS-22-57638; Editor assigned date: 21 March, 2022, PreQC No. JSNS-22-57638 (PQ); Reviewed date: 04 April, 2022, QC No. JSNS-22-57638; Revised date: 16 May, 2022, Manuscript No. JSNS-22-57638 (R); Published date: 23 June, 2022, DOI: 10.4172/2325-9701.1000131
Citation: Nishant N (2022) Hindi Translational and Modification of Modified JOA for Cervical Myelopathy and its Validation for Indian Population. J Spine Neurosurg 11:7
Abstract
Cervical myelopathy is due to cervical spinal canal narrowing which creates cascade of events leading to spinal cord dysfunction. It refers to a disease affecting the spinal cord with constellation of symptoms, signs, and imaging findings demonstrating the cervical spinal cord compression. The exact incidence of CSM still remains unknown. These cultural adaptations and differences have been reported and scoring system modified to accurately assess the outcome measures. Hindi version was comparable to their findings with good response, reliable, convergent construct validity, and acceptability. The JOA had excellent translation with all individual components motor, sensor and sphincter disturbances correlated strongly at first and second visit and the English version which is already validated tool. In prospective study performed the translation with validation of the Hong Kong (Chinese) version of questionnaire of the JOA which was reliable, and valid. Except for two patients, all cohorts were treated conservatively and the JOA-H score showed good clinical correlation with nurick scale as in the above study. The ease of adaptation, acceptability and comprehensibility reflected that patients focused clearly of the cervical spine symptoms and accurately related them in the questionnaire. The limitation of our study was that it was a single center study with not wide spectrum of the disease severity.
Keywords: Cervical myelopathy; Radiculopathy; Spinal trauma; cervical spondylosis
Introduction
Cervical myelopathy is due to cervical spinal canal narrowing which creates cascade of events leading to spinal cord dysfunction [1]. It refers to a disease affecting the spinal cord with constellation of symptoms, signs, and imaging findings demonstrating the cervical spinal cord compression [2]. The exact incidence of CSM still remains unknown. Wu et al in a national database among Taiwanese population reported an incidence of 4.04 per 100,000 person-years diagnosed with CSM based on hospitalization database [3]. In North America, the incidence and prevalence of DCM was 41 and 605 per million, respectively as reported by Nouri, et al. and 1.6 per 100,000 from Netherlands by Boogaarts, et al. [4,5].
The first scoring system for evaluation of cervical myelopathy was given by Japanese Orthopedic society in 1971 and had been widely used in Japan [6]. Hirabayashi, et al. first reported the patient reported outcomes in OPLL patients which were operated upon using this first JOA version [7]. However, one of the shortcomings of the original score was use of chopsticks because it is not used widely in all cultures. These cultural adaptations and differences have been reported and scoring system modified to accurately assess the outcome measures [8,9]. Different modifications to the original JOA scores reported as “modified JOA (mJOA) scores [10-18]. Benzel, et al. modified the original version of this scale in English language to match the cultural adaption in their native country, popularly known as mJOA.
Ideally, at regional level, it has to be translated and adapted culturally, in the native language of regional population for applying this scale for accurate clinical assessment. In Indian subcontinent, the daily activities include eating our daily food with hands, use the Indian styled toilet in rural areas, and certain religious practices integral to faith where squatting or sitting cross legged is routine. Therefore, such modifications are deemed necessary and have been reported in English language by Revappana, et al. (In-JOA-E) [19,20].
In Northern part of India where majority are Hindi speaking, a validation of Hindi version of the In-JOA-H will have huge impact on patient reported outcomes in planning for surgical intervention for patients suffering from cervical myelopathy. This will make it easier to translate and adapt to other Indian vernacular languages. The Aim of this study was to validate the Hindi version of the In-JOA-H for cervical myelopathy. Our other objectives were to translate, perform the back translation, acceptability, reliability, stability, response and equivalence of the In-JOA-H questionnaire.
Literature Review
This was a cross-sectional study of 193 patients, from November 2020 to May 2021 with ethical committee approval from the University Institutional review board in the out-patient Orthopedic Department of Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh, India. Patients with cervical myelopathy or neck pain with radiculopathy, satisfying the inclusion criteria are examined and with inclusion criteria of informed written consent from patients, diagnosis of myelopathy or radiculopathy as established by spine surgeon or the primary investigator using history, physical examination and/or radiological criteria and adults as per WHO definition (19 years and above) were included [21]. The exclusion criteria included those patients who had previous spine surgery, who had history of spinal trauma and history of recent external injury. 193 patients with cervical myelopathy or neck pain with radiculopathy were included in the study. The respondent to item ratio is 10:1 for validation and hence for a total of 19 questions, ten times the total is equivalent to 190, has been taken for our study [22,23].
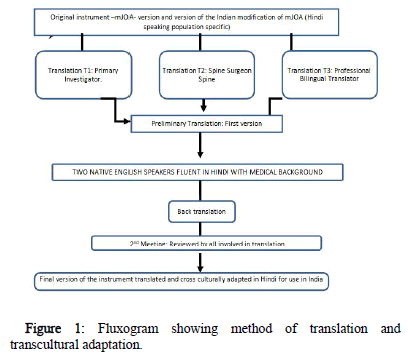
The steps of translations comprised of four stages translation-based Guillemin et al. method, (Figure 1) which included, stage 1 which involved translation (first version), back translation (second version), group meeting and the final version [24].
Stage 2 involved a pilot study of 19 patients to conduct a participant pretest of our final version of the Hindi version of the In-JOA-H questionnaire, to establish the acceptability of the translation (instructions, items, and response choices) in a face to face interviews to decide whether the participant had any trouble in comprehending the questionnaire. Any disparity in the interpretation is noted down for each question. The stage 3 involves the three evaluators fill the English version of the questionnaire, including the modified Nurick scale by spine surgeon. Stage 4 involved statistical analysis by SPSS 23.0 for Windows (IBM Corp., Armonk, New York, USA) was done for the psychometric parameters like acceptability, responsiveness, reliability, reproducibility (test-retest), validity (construct, concurrent, divergent, and discriminant) along with internal consistency of the Hindi version.
Results
The cultural adaptation: The Hindi version of In-JOA-H questionnaire was established by conducting a pilot study on 19 health individuals to ascertain, if there was any discrepancy in understanding, filling and regarding the comprehensibility of the content as mentioned in the fluxogram (Figure 1). There were no difficulty either in comprehension or the content of the Hindi questionnaire as encountered in the pilot study and the final outcome during all the patients enrolled (Table 1).
| Variables | Mean ± SD |
|---|---|
| Time to Fill Questionnaire (Minutes) In Hindi- | 3.37 ± 0.44 |
| Time to Fill Questionnaire (Minutes) In Hindi-After 7 Days | 2.87 ± 0.23 |
| Modified Nurick Scale (0-5) | 0 ± 0 |
| Modified Nurick Scale (0-5) after one week | 0 ± 0 |
| mJOA-E scoring system | 19 ± 0 |
| mJOA-E scoring system after one week | 19 ± 0 |
| mJOA-H scoring system | 19 ± 0 |
| mJOA-H scoring system after one week | 19 ± 0 |
| Upper limb | 6 ± 0 |
| Lower limb | 8 ± 0 |
| Sensory upper limb | 3 ± 0 |
| Sphincter dysfunction | 3 ± 0 |
| Upper limb | 6 ± 0 |
| Lower limb | 8 ± 0 |
| Sensory upper limb | 3 ± 0 |
| Sphincter dysfunction | 3 ± 0 |
| Upper limb | 6 ± 0 |
| Lower limb | 8 ± 0 |
| Sensory upper limb | 3 ± 0 |
| Sphincter dysfunction | 3 ± 0 |
| Upper limb | 6 ± 0 |
| Lower limb | 8 ± 0 |
| Sensory upper limb | 3 ± 0 |
| Sphincter dysfunction | 3 ± 0 |
Table 1: Pilot study data of 19 patients hindi version.
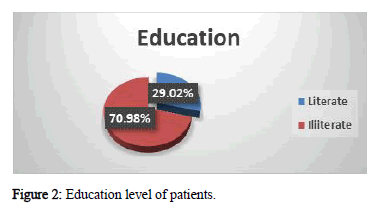
A total of 193 participants were included in the study the mean age was 41.89 ± 14.56 (range, 19-85). There were 78 male and 115 females. 56 out of the 193 (29%) were illiterate (Figure 2) and gave thumb impression for consent and were helped by a trained nurse for the oral translation of the Hindi version of the questionnaire.
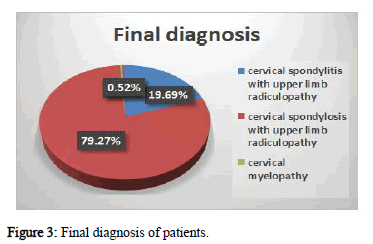
40 out of 193 were manual labour class, 102 were housewives, 26 farmers, 7 students, 2 businessmen, 1 teacher and 1 retired each, 3 nurse and 1 each were “anganwadi” worker, army man, dairy farmer, dentist, driver clerk, electrician, software engineer and vendor. We recorded 100% response rate and every patient completed the questionnaires on both visits one week apart. In terms of final diagnosis, one patient was diagnosed with cervical myelopathy and prolapsed intervertebral disc each. 2 patients were diagnosed with cervical spondylosis with upper limb radiculopathy and 38 patients were diagnosed with cervical spondylitis with upper limb radiculopathy, 153 with cervical spondylosis with upper limb radiculopathy and one patient each with myelopathy and prolapsed intervertebral disc (Figure 3).
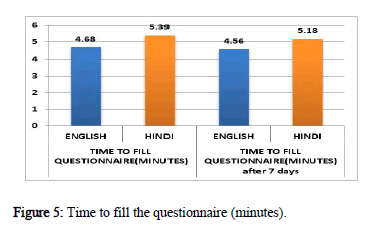
Acceptability, Responsiveness of the Hindi version of In-mJOA questionnaire and modified Nurick scale and correlation with English version of In-JOA scores (Tables 1-4): This was measured by recording the time to fill the questionnaire for both English and Hindi version of In-JOA. In our study, the mean time to fill questionnaire at first visit in English version was 4.68 ± 1.33 minutes and the mean time to fill questionnaire in Hindi version was 5.39 ± 1.44 minutes. The mean time was less in English version as compare to Hindi version to fill questionnaire at first visit and there was significant difference in mean time (Table 2).
| First Visit | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Group | N | Mean Rank | Sum of Ranks | P-Value | ||||
| Time to Fill Questionnaire (Minutes) | English | 193 | 164.9 | 31826 | <0.001* | ||||
| Hindi | 193 | 222.1 | 42865 | ||||||
| Time to Fill Questionnaire (Minutes) After 7 Days | English | 193 | 169.98 | 32805.5 | <0.001* | ||||
| Hindi | 193 | 217.02 | 41885.5 | ||||||
| Modified Nurick Scale (0-5) | English | 193 | 193.5 | 37345.5 | 1 | ||||
| Hindi | 193 | 193.5 | 37345.5 | ||||||
| Modified Nurick Scale (0-5) after one week | English | 193 | 193.5 | 37345.5 | 1 | ||||
| Hindi | 193 | 193.5 | 37345.5 | ||||||
| mJOA-E scoring system | English | 193 | 196.4 | 37905.5 | 0.285 | ||||
| Hindi | 193 | 190.6 | 36785.5 | ||||||
| mJOA-E scoring system after one week | English | 193 | 195.92 | 37813.5 | 0.379 | ||||
| Hindi | 193 | 191.08 | 36877.5 | ||||||
| Upper limb | English | 193 | 193.05 | 37258 | 0.839 | ||||
| Hindi | 193 | 193.95 | 37433 | ||||||
| Lower limb | English | 193 | 195.01 | 37637.5 | 0.532 | ||||
| Hindi | 193 | 191.99 | 37053.5 | ||||||
| Sensory upper limb | English | 193 | 194.48 | 37535.5 | 0.592 | ||||
| Hindi | 193 | 192.52 | 37155.5 | ||||||
| Sphincter dysfunction | English | 193 | 193.5 | 37345.5 | 1 | ||||
| Hindi | 193 | 193.5 | 37345.5 | ||||||
| Upper limb after one week | English | 193 | 194.01 | 37444.5 | 0.818 | ||||
| Hindi | 193 | 192.99 | 37246.5 | ||||||
| Lower limb after one week | English | 193 | 195.01 | 37637.5 | 0.532 | ||||
| Hindi | 193 | 191.99 | 37053.5 | ||||||
| Sensory upper limb after one week | English | 193 | 193.99 | 37440.5 | 0.782 | ||||
| Hindi | 193 | 193.01 | 37250.5 | ||||||
| Sphincter dysfunction after one week | English | 193 | 193.5 | 37345.5 | 1 | ||||
| Hindi | 193 | 193.5 | 37345.5 | ||||||
| Construct Validity: First Visit to After 7 Days Comparison of English and Hindi Version of mJOA: | |||||||||
| Variables | Group(N=193) | Mean | Std. Deviation | P-Value | |||||
| Time to fill questionnaire (Minutes) | English | 4.68 | 1.33 | <0.001* | |||||
| Hindi | 5.39 | 1.44 | |||||||
| Time to fill questionnaire (minutes) after 7 days | English | 4.56 | 1.25 | <0.001* | |||||
| Hindi | 5.18 | 1.45 | |||||||
| Modified Nurick scale (0-5) | 0.15 | 0.65 | 1.000# | ||||||
| Modified nurick scale (0-5) after one week | 0.15 | 0.65 | 1.000# | ||||||
| mJOA - scoring system | English | 18.7 | 1.33 | 0.626# | |||||
| Hindi | 18.63 | 1.38 | |||||||
| mJOA- scoring system after one week | English | 18.69 | 1.33 | 0.680# | |||||
| Hindi | 18.64 | 1.38 | |||||||
| Upper limb | English | 5.84 | 0.7 | 1.000# | |||||
| Hindi | 5.84 | 0.74 | |||||||
| Lower limb | English | 7.82 | 0.86 | 0.476# | |||||
| Hindi | 7.75 | 0.99 | |||||||
| Sensory upper limb | English | 2.95 | 0.28 | 0.720# | |||||
| Hindi | 2.94 | 0.29 | |||||||
| Sphincter dysfunction | English | 2.99 | 0.1 | 1.000# | |||||
| Hindi | 2.99 | 0.1 | |||||||
| Upper limb after one week | English | 5.83 | 0.76 | 0.796# | |||||
| Hindi | 5.81 | 0.81 | |||||||
| Lower Limb after one week | English | 7.82 | 0.86 | 0.476# | |||||
| Hindi | 7.75 | 0.99 | |||||||
| Sensory upper limb after one week | English | 2.95 | 0.28 | 0.856# | |||||
| Hindi | 2.95 | 0.28 | |||||||
| Sphincter dysfunction after one week | English | 2.99 | 0.1 | 1.000# | |||||
| Hindi | 2.99 | 0.1 | |||||||
| #-not significant; *-significant | |||||||||
Table 2: Construct validity: By mann-whitney test on first and second visit.
The mean time to fill questionnaire after 7 days in English version was 4.56 ± 1.25 minutes and the mean time to fill questionnaire in Hindi version was 5.18 ±1.45 minutes (Table 3). Inter-observer reliability to determine consistency among observer for the whole questionnaire and for each item, kappa value was 0.771 which indicate that both observers i.e. English version (In-JOA-E) and Hindi (In- JOA-H) version both has almost same as upper limb (Table 4).
| Symmetric Measures | |||||
|---|---|---|---|---|---|
| Value | Asymptotic Standardized Errora | Approximate Tb | Approximate Significance | ||
| Measure of Agreement | Kappa | 0.771 | 0.081 | 18.526 | 0 |
| N of Valid Cases | 193 | ||||
Table 3: Inter-observer reliability to determine consistency among observer for the whole questionnaire and for each item, kappa statistic was used.
| Variables | Variables | P-Value |
|---|---|---|
| Time to fill questionnaire (Minutes) | Time to fill questionnaire (Minutes) After 7 Days | |
| 4.68 ± 1.33 | 4.56 ± 1.25 | <0.001* |
| mJOA-scoring system | mJOA-scoring system after one week | |
| 18.70 ± 1.33 | 18.69 ± 1.33 | 1 |
| Upper limb | Upper limb 1 wk | |
| 5.84 ± 0.7 | 5.83 ± 0.76 | 1 |
| Lower limb | Lower Limb 1 wk | |
| 7.82 ± 0.86 | 7.82 ± 0.86 | 1 |
| Sensory Ul | Sensory Ul 1 wkk | |
| 2.95 ± 0.28 | 2.95 ± 0.28 | 1 |
| Sphincter dysfunction | Sphincter dysfunction 1 wkk | |
| 2.99 ± 0.1 | 2.99 ± 0.1 | 1 |
| Hindi version | ||
| Variables | Variables | P-Value |
| Time to fill questionnaire (Minutes) | Time to fill questionnaire (Minutes) after 7 days | |
| 5.39 ± 1.44 | 5.18 ± 1.45 | <0.001* |
| mJOA-scoring system | mJOA-scoring system after one week | |
| 18.63 ± 1.38 | 18.64 ± 1.38 | 1 |
| Upper limb | Upper limb after one week | |
| 5.84 ± 0.74 | 5.80 ± 0.81 | 0.158 |
| Lower limb | Lower limb after one week | |
| 7.75 ± 0.99 | 7.82 ± 0.86 | 1 |
| Sensory upper limb | Sensory upper limb after one week | |
| 2.94 ± 0.29 | 2.95 ± 0.28 | 0.319 |
| Sphincter dysfunction | Sphincter dysfunction after one week | |
| 2.99 ± 0.1 | 2.99 ± 0.1 | 1 |
| *statistically significant | ||
Table 4: Reproducibility (test-retest reliability): English version.
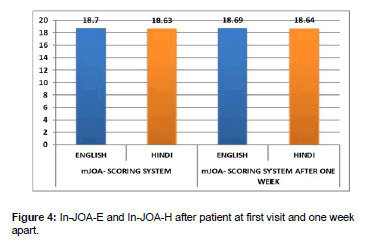
The mean In-JOA-E scoring system score after 7 days was 18.69 ± 1.33 and 18.64 ± 1.38 in the In-JOA-H, and there was no significant contrast in both versions (Figure 4).
Reproducibility (Test-Retest Reliability) and validity: Hindi Version: The mean time to fill questionnaire at first visit in the Hindi version In-JOA-H was 5.39 ± 1.44 minutes and after 7 days was 5.18 ± 1.45 minutes. The mean time was less after 7 days to fill questionnaire as compare to first visit (Table 5).
| Authors | Findings of the study | Conclusion | Our findings | |
|---|---|---|---|---|
| 1971. | Japanese orthopedic society | It had set questions addressing the cervical spine and cord functions | No validation data was available. | Our Hindi version of mJOA met our entire requirement to be used as a validation tool by establishing, acceptability, equivalence, reproducibility, reliability, responsiveness, construct validity, divergent validity, concurrent validity, discriminant validity and Internal consistency. Our Hindi version of mJOA met our entire requirement to be used as a validation tool by establishing, acceptability, equivalence, reproducibility, reliability, responsiveness, construct validity, divergent validity, concurrent validity, discriminant validity and Internal consistency. Our Hindi version of mJOA met our entire requirement to be used as a validation tool by establishing, acceptability, equivalence, reproducibility, reliability, responsiveness, construct validity, divergent validity, concurrent validity, discriminant validity and Internal consistency. Our Hindi version of mJOA met our entire requirement to be used as a validation tool by establishing, acceptability, equivalence, reproducibility, reliability, responsiveness, construct validity, divergent validity, concurrent validity, discriminant validity and Internal consistency. |
| 1981 | Hirabayashi, et al. | First Japanese version of the mJOA translation and also first mJOA score introduced in cervical spine. Proposed the original mJOA score with chopsticks showing good correlation | The authors concluded that JOA score could be used for cervical pathology but need of validation was required | |
| 1991 | Benzel, et al. | First English version of myelopathic score in USA. Preoperative mJOA had good correlation with postoperative mJOA in English version.18 point scale was validated and responsive | The reported it to be an accurate scale but the benefits of laminectomy with dentate ligament section could not be fully established. | |
| 1994 | Japanese orthopedic Society | JOA first revision for shoulder elbow function for cervical lesions; first officially translated into English (In Japanese with English translation | No validation data was available. | |
| 2002 | Jain et al. | First Indian modification of JOA scale in patients with Congenital Atlanta-Axial Dislocation with an associated Chiari malformation in English. Authors did not provide the data regarding validation or inter-observer correlation with the original JOA score. | The review of congenital AAD in the management should be based on personal expertise. However, the surgery did not always show clinical improvement or the score. | |
| 2007 | Fukui, et al. | Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire-Part 1. The first part of the JOA score was established. | This was the first part of JOA score in Japanese but lacked reliability advocated next study to establish its reliability. | |
| 2007 | Fukui, et al. | Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire-Part 2. Validate the first part of the JOA score including a minor modification. excellent reliability of the questionnaire along with high spearmen correlation and proved to be a reliable tool to be used worldwide | This was the second part of the study which established its reliability. | |
| 2007 | Fukui, et al. | Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire-Part 3. Determination of reliability. Further reliability was tested with 24 questionnaire showed excellent reliability with kappa coefficient ≥0.4. | This third part of the study evaluated further reliability with good correlation. | |
| 2007 | Fukui et al. | Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire-Part 4. Establishment of equations for severity scores. 24 questions, divided into 5 different components all factors shoed correlation but lack of validation data future studies were proposed. | The fourth part of the study established its reliability and still was not validated. | |
| 2010 | Bartels, et al. | The mJOA version described by Benzel et al and translated into the Dutch version in patients with spinal disorders. The total numbers of patients, initially, recruited were only 7 which showed a kappa correlation of 0.56 ± 0.11 but after including 18 more patients the kappa correlation increased to 0.78 ± 0.5 which reflected a statistically significant correlation. | The authors reached the conclusion that despite the small number of patients. The study had achieved good translation but needed further study with wider spectrum of patients from mild, moderate and severe diseased patients as the score was a subjective interpretation with varied response from patients. | |
| 2014 | Chien, et al. | Validated the Chinese version of mJOA (JOACMEQ). Among The 5 components of mJOA only two components showed (upper and lower) showed significant correlation with sensitivity and specificity. Responsiveness was not part of the study. NDI had moderate correlation with mJOA. Concurrent validity was weak to moderate Discriminant validity was established. Construct validity along with reproducibility and internal consistency was acceptable for all components. | The authors concluded that Chinese JOACMEQ retained the psychometric properties of the Original JOACMEQ with established valid tool as diagnostic and patient reported outcome measure. | |
| 2014 | Augusto, et al. | Established the Portuguese version of mJOA. The NDI scale was used to compare with mJOA. The translation was reliable, with acceptable comprehension. Internal consistency displayed strong correlation between mJOA-Br and NDI-Br (spearmen-coefficient was 0.752 and 0.615). Highly specific and validated tool for CSM | The authors concluded that mJOA in Portuguese language had some minor variations and regional differences spoken in other countries which needed further analysis. | |
| 2015 | Revanappa, et al. | Indian modification of mJOA and Nurick scale include certain culture specific practices in English language. showed 0.737 compared to 0.679 correlation (Spearman’s quotient) lower limb mJOA and total mJOA scores | Modified Nurick grade and lower limb mJOA had good correlation with 11.8% with discord for moderate and serve myelopathy. The reason for discord was they measure separate domains. | |
| 2016 | Longo, et al. | Italian (mJOA-IT) translation and modification of the mJOA score. The convergent construct validity showed moderate association with mJOA-IT. The divergent validity was not correlated with SF-36. The pre and post-operative mJOA-IT was responsive at end of one year. | The authors of Italian version of mJOA was reliable and valid tool for CSM assessment tool. | |
| 2018 | Cheung, et al. | The translation with validation of the Hong Kong (Chinese) version of questionnaire of the JOA (JOACMEQ). Scale was reliable; valid translated JOACMEQ had excellent internal consistency with lower limb function and QOL with Cronbach’s α> 0.9 | The authors concluded that the translated version was effective and reflects the quality of life in CSM with good correlation with treatment outcomes. JOACMEQ was sensitive in differentiating between CSM and patients with neck pain or shoulder pain. |
Table 5: Summary of different studies with their outcome.
Construct validity: The construct validity was recorded by applying non parametric test, Mann-Whitney which was significant first visit and after 7 days comparing the English and Hindi version showed significant difference with p value <0.001 (Table 2). The Questionnaire has good construct validity and test-retest reliability in people with the stage involves patient filling the Hindi version of the questionnaire (Table 2).
Divergent validity: As there are no standard for definition of CSM, there are no such criteria which strictly defines CSM measurement. Henceforth, we measured the mean score of both versions (In-JOA-E and In-JOA-H) at first visit and second visit and compared it with Nurick scale (Table 2) to establish the divergent validity.
Concurrent validity: This is also known as the clinical validity which was calculated by Spearman coefficient. This coefficient is required to study the association between In-JOA-E, English version with modified Nurick scale and the association between In-JOA-H, Hindi version with modified Nurick scale. The spearmen co-efficient was 0.792 and 0.791 for the first visit between In-JOA-, English version with modified Nurick scale and for Hindi version, In-JOA-H at first visit was 0.656 and after 7 days was 0.654.
Discriminant Validity: The Hindi version, In-JOA-H accurately differentiate between patients with clinically diagnosed CSM or those suffering with neck pain along with radiculopathy of other causes by calculating the Mann Whitney score showed significant difference with p value <0.001(Table 2). Inter-observer reliability to determine consistency among observer for the whole questionnaire and for each item, kappa value is 0.771 which indicate that both observers i.e. English version and Hindi version both has almost same as upper limb (Table 2).
Discussion
Revision of the original JOA by Benzel, et al. (mJOA) was based on the eating food habit using chopsticks, which may not be widely used in many parts of the world [25]. Hence, such modifications are deemed necessary. The Indian modification of In-JOA-H has a total of 19 components. The upper limb extremity has 6 grades, an additional modification of grade 5. The rest of the components are same as In- JOA-H established by Revanappa et al. to include certain culture specific practices like squatting, eating bread or chapatti with hand albeit in English language. Jain et al have reported the only previous Indian modification to JOA in Hindi language with eating rice was allocated a higher function (score of 2) while lower grade was attributed to holding or griping a pen for writing [26]. The authors classified the upper limb activities by ability to eat with spoon, eat rice with fingers and ability to write. The authors did not provide the data regarding validation or inter-observer correlation with the original JOA score.
Our goal was to differentiate between different regional pathologies by asking questions in the local language and guide towards specifically spinal intervention. One such example was especially asking patients was eating with hand and getting up from sitting position. The JOA score after one week of did not show any difference in the score. This could be due to short course of treatment as the disease process doesn’t change in a week’s time and was mandatory to establish its validity, acceptability and responsiveness. The English version of Revappanaal depicted good correlation with severity score. Henceforth, as the English and Hindi version of In-JOA-E and InJOAHhad similar correlation, we could indirectly state that it would be similar for moderate and severe category following surgical intervention as well (Figure 5).
Chiles, et al. used changes in the JOA scale by replacing the chopsticks with the use of a knife and fork [27]. The mJOA score by Benzel, et al. was highly responsive along with convergent validity. The Nurick scale was predictive of the outcome measures and was also predictive tool of outcome. We excluded QoL scores due their consistent lack of correlation in literature and focused on the Nurick scale correlation with Indian modification of In-JOA-E and InJOA-H [28]. Chien, et al. validated the Chinese version of mJOA as a valid, pertinent assessment tool for CSM10. This was based on the self reporting questionnaire by Beaton, et al. However, none of individuals involved in these studies suffered from CSM similar to our study with only one patient with CSM10. Chien et al adopted Betaon, et al. guidelines unlike our study which was based on Guillemin, et al. method of translation. However, the authors lacked responsiveness of the translation as the clinical trials had not yet begun. The authors pointed out that it was a valid tool since they established the construct validity which is the most important psychometric property for a valid questionnaire. Augusto, et al. established the Portuguese version of JOA, (mJOA-Br) used NDI scale to evaluate myelopathic following the Guillemin, et al. to establish the Brazilian Portuguese (mJOA-Br). The divergent validity was strong and showed high specificity of the mJOA-Br for SCM and correlated strongly with NDI scores. There is disparity in correlation to NDI compared to Chien, et al. due to their small sample size; any concrete conclusion cannot be derived. Longo, et al. conducted a study of the Italian (mJOA-IT) translation and modification of the mJOA score [29]. The Italian translation and modification was deemed reliable and its validity was established when compared to Nurick scale but showed no association with either NDI or SF-36 but was responsive. The translation had good acceptability with average time required to fill the questionnaire was 5 min (range 3-10 min). The average time to fill the questionnaire was in InJOA-H, Hindi version was 5.39 ± 1.44 minutes (range 2-9 minutes) with only 2 patients had multiple answers and recorded 100% response rate. Hindi version was comparable to their findings with good response, reliable, convergent construct validity, and acceptability. The In-mJOA had excellent translation with all individual components motor, sensor and sphincter disturbances correlated strongly at first and second visit and the English version which is already validated tool. Cheung, et al. in prospective study performed the translation with validation of the Hong Kong (Chinese) version of questionnaire of the JOA which was reliable, and valid [30]. Except for two patients, all cohorts were treated conservatively and the InJOA-H score showed good clinical correlation with Nurick scale as in the above study. A review of studies done on mJOA translations in various languages worldwide is illustrated in the Table 5. In-JOA proved to be valid functional evaluation tool in patients with CSM or those who are pre-stage of CSM as in cervical spondylosis. The ease of adaptation, acceptability and comprehensibility reflected that patients focused clearly of the cervical spine symptoms and accurately related them in the questionnaire. The limitation of our study was that it was a single center study with not wide spectrum of the disease severity.
Conclusion
Nurick and mJOA measure separate domains on the functional scale and despite the minor disagreement have good correlation. We recommend continuing using modified Nurick and Indian specific JOA scales, InJOA-H for our population to meet the cultural adaptations. We strongly recommend such patient reported outcomes in the local language and encourage to be translated in other vernacular languages.
References
- Salemi G, Savettieri G, Meneghini F, Di Benedetto ME, Ragonese P, et al. (1996) Prevalence of cervical spondylotic radiculopathy: a door-to door survey in a Sicilian municipality. Acta Neurol Scand 93:184-188. [Googlescholar] [Crossref] [Indexed]
- Barnes MP, Saunders M (1984) The effect of cervical mobility on the natural history of cervical spondylotic myelopathy. J Neurol Neurosurg Psychiatry 47:17-20. [Googlescholar][Crossref][Indexed]
- Wu JC, Ko CC, Yen YS, Huang WC, Chen YC, et al. (2013) Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: a national cohort study. Neurosurgical focus 35:E10. [Googlescholar][Crossref][Indexed]
- Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG (2015) Degenerative cervical myelopathy: epidemiology, genetics and pathogenesis. Spine 40:E675-693. [Googlescholar][Crossref][Indexed]
- Boogaarts HD, Bartels RH (2015) Prevalence of cervical spondylotic myelopathy. Eur Spine J 24:139-141. [Googlescholar][Crossref][Indexed]
- Fukui M (1975) Japanese Orthopaedic Association Score for cervical spondylotic myelopathy. J Jpn Orthop Assoc 99.
- Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K (1981) Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine 6:354-64. [Googlescholar][Crossref] [Indexed]
- Denaro V (1991) Classification of Stenoses. InStenosis of the Cervical Spine 5-28. Springer, Berlin, Heidelberg.
- Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, et al. (2008) Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 4. Establishment of equations for severity scores. J Orthop Sci 13:25-31. [Googlescholar] [Crossref][Indexed]
- Chien A, Lai DM, Cheng CH, Wang SF, Hsu WL (2014) Translation, cross-cultural adaptation, and validation of a Chinese version of the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire. Spine 39:963-970. [Googlescholar] [Crossref] [Indexed]
- Carreon LY, Glassman SD, Campbell MJ, Anderson PA (2010) Neck Disability Index, short form-36 physical component summary, and pain scales for neck and arm pain: the minimum clinically important difference and substantial clinical benefit after cervical spine fusion. Spine J 10:469-474. [Googlescholar][Crossref][Indexed]
- Bartels RH, Verbeek AL, Benzel EC, Fehlings MG, Guiot BH (2010) Validation of a translated version of the modified Japanese orthopaedic association score to assess outcomes in cervical spondylotic myelopathy: an approach to globalize outcomes assessment tools. Neurosurgery. 66:1013-6. [Googlescholar][Crossref][Indexed]
- Benzel E (2001) Deformity prevention and correction: component strategies. Biomechanics of Spine Stablization. Rolling Meadows, IL: AANS Publications: 357-74.
- Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K (2001) Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy. Spine 26:1890-1894. [Googlescholar] [Crossref][Indexed]
- Fukui M, Chiba K, Kawakami M, Kikuchi SI, Konno SI, et al. (2007) An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1. J Orthop Sci 12:227-40. [Googlescholar][Crossref][Indexed]
- Fukui M, Chiba K, Kawakami M, Kikuchi SI, Konno SI, et al. (2007) Japanese orthopaedic association cervical myelopathy evaluation questionnaire (JOACMEQ): Part 2. Endorsement of the alternative item. J Orthop Sci 12:241-8. [Googlescholar] [Crossref][Indexed]
- Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, et al. (2007) Japanese orthopaedic association cervical myelopathy evaluation questionnaire: part 3. Determination of reliability. J Orthop Sci 12:321-326. [Googlescholar][Crossref][Indexed]
- Benzel EC, Lancon J, Kesterson L, Hadden T (1991) Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spinal Disord 4:286-295. [Googlescholar][Crossref][Indexed]
- Revanappa KK, Rajshekhar V (2011) Comparison of Nurick grading system and modified Japanese Orthopaedic Association scoring system in evaluation of patients with cervical spondylotic myelopathy. Eur Spine J 20:1545-1551. [Googlescholar] [Crossref] [Indexed]
- Revanappa KK, Moorthy RK, Jeyaseelan V, Rajshekhar V (2015) Modification of Nurick scale and Japanese Orthopedic Association score for Indian popupperlimbation with cervical spondylotic myelopathy. Neurol India 63:24-29. [Googlescholar][Crossref] [Indexed]
- Canêo LF, Neirotti R (2017) The Importance of the Proper Definition of Adulthood: What is and What is Not Included in a Scientific Publication. Braz J Cardiovasc Surg. 32:60-61. [Googlescholar] [Crossref] [Indexed]
- Gorsuch RL (1983) Factor Analysis. 2nd edition Hillsdale NJ (eds): Lawrence Erlbaum Associates, p425.
- Osborne JW, Costello AB (2004) Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval 9:11. [Googlescholar] [Crossref]
- Guillemin F, Bombardier C, Beaton D (1993) Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 46:1417-1432. [Googlescholar][Crossref][Indexed]
- Jain VK, Behari S (2002) Management of congenital atlanto axial dislocation: Some lessons learnt. Neurol India 50:386-397. [Googlescholar][Crossref][Indexed]
- Chiles III BW, Leonard MA, Choudhri HF, Cooper PR (1999) Cervical spondylotic myelopathy: patterns of neurological deficit and recovery after anterior cervical decompression. Neurosurg 44:762-769. [Googlescholar] [Crossref] [Indexed]
- Augusto MT, Diniz JM, Dantas FL, de Oliveira MF, Rotta JM (2018) Development of the Portuguese Version of the Modified Japanese Orthopaedic Association Score: Cross Cultural Adaptation, Reliability, Validity and Responsiveness. World Neurosurg 116:e1092-1097. [Googlescholar] [Crossref] [Indexed]
- Longo UG, Berton A, Denaro L, Salvatore G, Denaro V (2016) Development of the Italian version of the modified Japanese orthopaedic association score (mJOAIT): cross -cultural adaptation, reliability, validity and responsiveness. European Spine Journal. Sep 1;25:2952-2957. [Googlescholar][Crossref][Indexed]
- Cheung PW, Wong CK, Lau ST, Cheung JP (2018) Psychometric validation of the adapted traditional Chinese (Hong Kong) version of the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ). Spine 43:E242- 249.[Googlescholar] [Crossref] [Indexed]
- (1994) Revised Japanese Orthopaedic Association scores for cervical myelopathy. J Jpn Orthop Assoc 68:490–503.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi