Review Article, J Liver Dis Transplant Vol: 4 Issue: 1
Gut Flora in the Development and Progression of Nonalcoholic Fatty Liver Disease
| Vera Okwu1*, Ammar Matloob1 and Naim Alkhouri1,2* | |
| 1Department of Pediatric Gastroenterology and Hepatology, Cleveland Clinic, Cleveland, Ohio, USA | |
| 2Digestive Disease Institute, Cleveland Clinic, Cleveland, Ohio, USA | |
| Corresponding author's : Naim Alkhouri, Digestive Disease Institute, Cleveland Clinic Foundation, 9500 Euclid Avenue, Cleveland, Ohio 44195, USA, Tel: 216-444-9000 Fax: 216-444-2974; E-mail: alkhoun@ccf.org Vera Okwu, Department of Pediatric Gastroenterology and Hepatology, 9500 Euclid Ave, Crile Building A111, Cleveland, Ohio 44195, USA, Tel: (216) 444-9000; Fax: 216-444-2974; E-mail: OKWUV@ccf.org |
|
| Received: February 06, 2015 Accepted: July 01, 2015 Published: July 07, 2015 | |
| Citation: Okwu V, Matloob A, Alkhouri N (2015) Gut Flora in the Development and Progression of Nonalcoholic Fatty Liver Disease. J Liver: Dis Transplant 4:1. doi:10.4172/2325-9612.1000128 |
Abstract
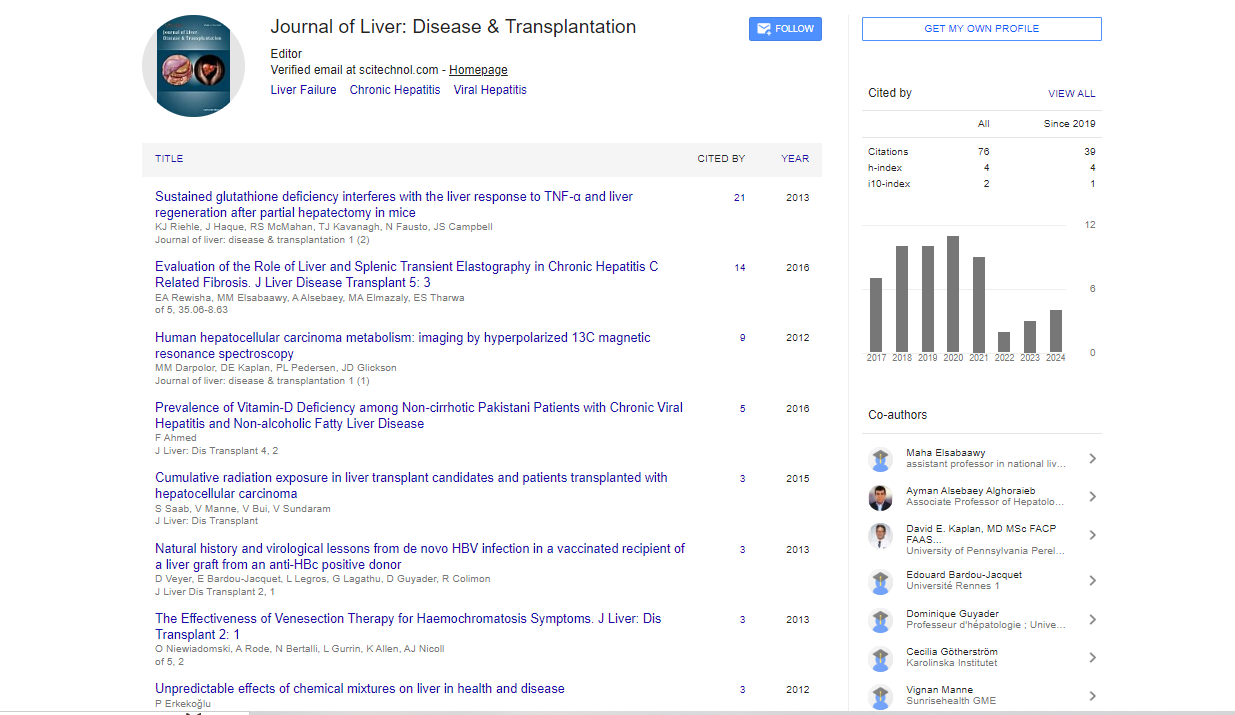
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the United States. There is an increased prevalence noted among individuals with morbid obesity and type 2 diabetes. The prevalence of NAFLD is expected to continue to rise given the current global obesity epidemic. The pathogenesis of NAFLD is not clearly understood, but there is emerging evidence to suggest that the gut microbiota plays an important role. The gut microbiota is involved in dietary energy extraction, bile acid metabolism, endogenous alcohol production, choline metabolism, modulation of the host’s immune system and alteration of intestinal permeability. This review focuses on the potential pathways through which the gut microbiota is linked to the development and progression of NAFLD. Figure 1 is our proposed schematic representation of the role of the gut microbiota in NAFLD.
Keywords: Nonalcoholic fatty liver disease; Nonalcoholic steatohepatitis; Gut microbiota; Obesity
Abstract |
|
| Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in the United States. There is an increased prevalence noted among individuals with morbid obesity and type 2 diabetes. The prevalence of NAFLD is expected to continue to rise given the current global obesity epidemic. The pathogenesis of NAFLD is not clearly understood, but there is emerging evidence to suggest that the gut microbiota plays an important role. The gut microbiota is involved in dietary energy extraction, bile acid metabolism, endogenous alcohol production, choline metabolism, modulation of the host’s immune system and alteration of intestinal permeability. This review focuses on the potential pathways through which the gut microbiota is linked to the development and progression of NAFLD. Figure 1 is our proposed schematic representation of the role of the gut microbiota in NAFLD. | |
| Figure 1: Schematic representation of the role of gut microbiota in the development and progression of NAFLD. Ingestion of the typical American diet which consists of refined grains, added sugars, fats and red meat with decreased activity likely leads to obesity. Obesity results in gut dysbiosis with increased energy extraction and storage of SCFA and FFA in the liver leading to simple steatosis. Gut dysbiosis also results in increased production of pro-inflammatory cytokines, decreased choline bioavailability and increased production of endogenous alcohol leading to disease progression from simple steatosis to NASH. | |
Keywords |
|
| Nonalcoholic fatty liver disease; Nonalcoholic steatohepatitis; Gut microbiota; Obesity | |
Introduction |
|
| The human gastrointestinal tract is sterile at birth but is rapidly colonized by microorganisms that form a dense stable microbial population at the time of weaning [1]. This microbial population is composed of thousands of bacterial species that belong to a small number of phyla, with significant variability between individuals with regards to the relative ratios of the dominant phyla and variation in the genera and species found in an individual host [2]. There is evidence to suggest that the composition of this microbial population in individuals is shaped by several environmental and genetic factors [3]. This stable microbial population is referred to as the gut microbiota, and plays a key role in several complex metabolic processes and human diseases. | |
| The central location of the liver along with its unique vasculature makes it crucial for digestion, detoxification and host immunity [4]. The liver and the gastrointestinal tract communicate very closely through bile, hormones, inflammatory mediators and products of digestion and absorption. Therefore, the composition, quantity and quality of the gut microbiota would be expected to affect both the physiology of the liver and the progression of liver disease [5]. Hoefert explored this relationship between the liver and the gut microbiota more than 80 years ago when he described alterations in gut microbiota of patients with chronic liver disease [6]. | |
| Nonalcoholic fatty liver disease (NAFLD) occurs on a spectrum that ranges from hepatic steatosis to nonalcoholic steatohepatitis (NASH) which is histologically characterized by hepatocyte ballooning, inflammation, necrosis and fibrosis (NASH) [7]. It is the most common etiology of chronic liver disease in the United States and affects about 23% of the general population [8]. The prevalence of NAFLD and NASH among morbidly obese patients is estimated to be about 91% and 37% respectively [9-11]. In patients with type 2 diabetes, the prevalence of NAFLD and NASH is estimated to be about 60-76% and 22% respectively [12,13]. The increased prevalence of NAFLD and NASH among patients with morbid obesity and type 2 diabetes indicates that these two conditions are major risk factors for the development and progression of NAFLD. Individuals with NASH, the more severe form of NAFLD are at an increased risk of hepatic cirrhosis, hepatic decompensation and hepatocellular carcinoma [14-17]. | |
| Given the current global obesity epidemic, the prevalence of NAFLD and NASH is expected to continue to rise. The association between NAFLD, insulin resistance and metabolic syndrome makes NAFLD a major public health concern. The intimate relationship between the liver and the gut has led to recognition of the importance of the gut microbiota in NAFLD. This review article aims to summarize what is currently known about the role of the gut microbiota in the pathogenesis of NAFLD. | |
Microbiota and Obesity |
|
| Microbiota effect on energy harvest and deposition | |
| The gut microbiota is important in the digestion of resistant starch and dietary fibers that are incompletely degraded in the small intestine [18]. The main byproducts of this process include short chain fatty acids (SCFAs), acetate, propionate and butyrate which can be further utilized for lipid or glucose de novo synthesis [19]. The SCFAs that result from bacterial degradation of dietary fiber in the large intestine provide an additional energy source for the body. | |
| The composition of the gut microbiota is important in this process of energy extraction and deposition. A study by Eckburg, examining the composition of the gut microbiota in healthy subjects found that most of their gut microbiota was comprised of members of the Firmicutes and Bacteroidetes phyla with large variations noted among the Bacteroidetes phylotypes between subjects [20]. Despite the large variations among the Bacteroidetes phylotypes between subjects, an organism known as Bacteroides thetaiotamicron was found to be present in all subjects. This organism is a known bacterial symbiont which is a dominant member of the intestinal microbiota of humans and other mammals. It plays an important role in the utilization of energy sources from the diet of its host because of its unique ability to acquire, hydrolyze and metabolize complex polysaccharides [21].Another study by Backhed, examining the gut microbiota in mice found that introduction of gut microbiota from conventionally raised mice into germ free mice produced a 60% increase in body fat content and insulin resistance within 2 weeks despite reduced food intake in the germ free mice. The study also showed that the gut microbiota promoted the absorption of monosaccharides from the gut lumen with resultant induction of de novo hepatic lipogenesis [22]. | |
| Emerging studies show there is an underlying difference in the composition of the gut microbiota of obese individuals compared to their lean counterparts. A study by Kalliomaki prospectively evaluated the gut microbiota of human subjects who were of normal weight, overweight or obese from birth to age 7. The study showed that Bifidobacterium species were higher in the gut microbiota of subjects who maintained a normal weight compared to those who became overweight. The study also showed that Staphylococcus aureus species were lower in the gut microbiota of subjects who maintained a normal weight compared to those who became overweight [23]. Another study by Ley et al. examining the microbiota composition of lean and genetically obese mice found that the genetically obese mice had a 50% reduction in Bacteroidetes species and a proportional increase in Firmicutes species when compared to their lean counterparts, suggesting that obesity does affect the diversity of the gut microbiota [24]. | |
| Recent studies show there is a difference in the ability for energy harvest in the gut microbiota of obese individuals compared to their lean counterparts. A study by Turnbaugh characterizing the distal gut microbiota of genetically obese mice and lean mice showed that the obese microbiota had an increased capacity to harvest energy from the diet and that colonization of germ free mice with gut microbiota of obese mice led to significantly greater increase in total body fat compared to colonization with gut microbiota from lean mice [25]. Another study by Ridaura examined the gut microbiota of twin mice discordant for obesity and showed that there was increased total body and fat mass along with obesity associated phenotypes when gut microbiota from twin mice discordant for obesity was transplanted into germ free mice fed a low-fat mouse chow as well as diets representing different levels of saturated fat, fruits and vegetable consumption typical of the U.S diet. The study also showed that co-housing mice containing the obese twin’s microbiota with mice containing the lean co-twin’s microbiota prevented the development of increased body mass and obesity-related metabolic phenotypes in obese cage mates [26]. | |
| There is evidence to suggest that the diet can also alter the gut microbiota over time and potentially contribute to obesity. A study by Ley et al. examining the relationship between gut microbiota and body fat in obese subjects randomly assigned to a fat-restricted or carbohydrate- restricted low calorie diet showed that members of the Bacteroidetes and Firmicutes divisions dominated the microbiota of the subjects involved in the study. The study also showed that obese subjects had fewer Bacteroidetes and more Firmicutes compared to lean controls prior to dietary interventions with noted increased abundance of Bacteroidetes and concurrent decreased abundance of Firmicutes over time irrespective of diet type. Finally, the study showed that over time increased abundance of Bacteroidetes correlated with percentage loss of body weight and not with changes in dietary calorie content [27]. Another study by Turnbargh clearly illustrates this concept [28]. Using humanized gnotobiotic mice Turnbaugh showed that switching from a low-fat plant polysaccharide-rich diet to a highfat, high-sugar “Western” diet shifted the structure of the microbiota within one day, changed the representation of the metabolic pathways in the microbiome and altered microbiome gene expression [28]. The study also found that the colonization history of the mice influences the initial structure of the microbiome community, an effect that can be rapidly altered by diet. Finally, they found that the humanized mice fed the Western diet had increased adiposity a trait that was transmissible through microbiota transplantation [28]. | |
| Finally, studies suggest that there is an underlying difference in the gut microbiota of patients with biopsy-proven NAFLD compared to healthy controls. A prospective cross sectional study by Mouzaki examining the gut microbiota of patients with biopsy proven NAFLD and healthy controls showed that patients with NASH had a lower percentage of Bacteroidetes species independent of diet and BMI compared to patients with simple steatosis and healthy controls [29]. | |
| Microbiota effect on bile acid metabolism | |
| Bile acids are primarily known for their role in the digestion and absorption of fats and fat soluble vitamins in the small intestine as well as their control of cholesterol homeostasis [30,31]. Over the last decade, bile acids have become recognized for their role in several metabolic processes including activation of various metabolic pathways, regulation of their own synthesis, regulation of the enterohepatic circulation and regulation of cholesterol, triglycerides, glucose and energy metabolism [31]. Emerging evidence now suggests that bile acids can also affect the composition and size of the gut microbiota [32]. This is very important because the gut microbiota is shown to be essential in bile acid metabolism and can influence pathways involving lipid and energy metabolism, affecting lipid peroxidation and storage of fatty acids in the liver [33]. | |
| The human liver is the only organ capable of producing all of the enzymes required for de novo synthesis of primary bile acids [34]. Primary bile acids are synthesized in the liver from cholesterol via both the classical and alternate pathways. The classical pathway is considered the major bile acid synthetic pathway in humans and produces cholic acid and chenodeoxycholic acid. Cholesterol 7α-hydroxylase, a microsomal cytochrome p450 enzyme, catalyzes the first and rate limiting step in the classical pathway [35]. The alternate pathway, which accounts for about 10% of the total bile acid synthesis in humans, produces mainly chenodeoxycholic acid. Mitochondrial 27-hydroxylase and oxysterol 7α-hydroxylase are the main catalysts in the alternate pathway [36]. The difference in the amount of bile acids synthesized in each of the above mentioned pathways explains why the classical pathway is typically favored, but in the setting of liver disease will be likely down regulated [37]. | |
| After synthesis, primary bile acids are conjugated with glycine or taurine, excreted and then stored as mixed micelles in the gallbladder for future use [31]. Primary bile acids are actively reabsorbed in the terminal ileum with about 5% entering into the colon daily. Upon entry into the colon, primary bile acids are metabolized through 7α-dehydroxylation into secondary bile acids (deoxycholic acid and lithocholic acid) by anaerobic bacteria in the colon. Deoxycholic acid is partly re-absorbed in the colon and enters the enterohepatic circulation where it is conjugated in the liver and secreted in the bile [38]. The gut microbiota responsible for the process of 7α-dehydroxylation belongs to the genus Clostridium which are gram positive anaerobic spore members of the Firmicutes [39]. The gut microbiota is important in the synthesis of secondary bile acids but there is evidence to suggest that those bile acids are capable of modifying microbiota composition. Several animal models show that increased bile acid levels in the colon select against Actinobacteria and Bacteroidetes while favoring Firmicutes including bile acid 7α dehydroxylating bacteria in vivo [40]. | |
| Bile acids as previously mentioned also function as signaling molecules and bind to cellular receptors like farnesoid X receptor (FXR) and G protein-coupled receptor (GPCR) TGR5 that control bile acid synthesis and transport through a negative feedback system [41]. FXR is activated by primary bile acids and is implicated in impaired glucose homeostasis in obese mice [42]. TGR5 on the other hand is activated by secondary bile acids and promotes glucose homeostasis in obese mice [43]. In mice, bile acid 7α-dehydroxylating bacteria are shown to be capable of controlling bile acid synthesis in the liver by removing FXR antagonist tauro-β muricholic acid in the ileum [44]. In humans, other members of the gut microbiota have been shown to shrink the bile acid pool through inhibition of bile acid synthesis in the liver by inflammation [45]. With liver inflammation, the expression of ileal bile acid transporters increases with resultant decrease in bile acids in the colon likely due to decreased bile salts concentration [46]. | |
Microbiota and NAFLD |
|
| Microbiota and endogenous alcohol | |
| The gut microbiota produces a number of potentially hepatotoxic compounds such as ammonia, acetylaldehyde, benzodiazepines, ethanol and phenols [47]. These compounds are delivered to the liver via the portal circulation and activate Kupffer cells with resultant production of cytokines and nitric oxide [47]. Acetate and acetaldehyde are the two main metabolites of ethanol, with acetate being a substrate for fatty acid synthesis and acetaldehyde possibly leading to the production of reactive oxygen species (ROS). An alteration in the intestinal barrier might facilitate translocation of these compounds to the liver resulting in hepatotoxic changes within the liver. | |
| The hepatotoxic changes that result from endogenous ethanol production are very similar to the changes seen in the setting of alcoholic liver disease (ALD). ALD is the hepatic manifestation of chronic alcohol consumption that includes fatty liver, chronic hepatitis and chronic hepatitis with hepatic fibrosis or cirrhosis [48]. The process that results in liver damage in chronic alcoholic consumption is not entirely clear, but is thought to be secondary to secretion of pro-inflammatory cytokines, oxidative stress, lipid peroxidation and acetylaldehyde toxicity which results in hepatic inflammation, apoptosis and eventually fibrosis [49]. The noted alteration in the composition of the colonic mucosa associated microbiota in alcohol fed mice [50], and the increased incidence of bacterial overgrowth favoring gram negative bacteria in the setting of chronic alcohol consumption [51] implicates the gut microbiota in the pathogenesis of ALD. Although the effect of alcohol consumption on gram positive bacteria is unknown, peptidoglycan (produced by gram positive bacteria) levels are shown to be elevated in mice after prolonged administration of alcohol in their drinking water but interestingly does not result in ALD [52]. | |
| There is evidence that supports the endogenous production of ethanol and a difference in the amount produced in obese individuals compared to lean individuals. A study published in 2000 by Cope et al. evaluated gastrointestinal ethanol production in mice and detected exhaled breath ethanol in both lean and obese mice in the absence of ethanol ingestion [53]. The study also showed decreased exhaled ethanol following use of antibiotics and an age related increase in breath ethanol in obese mice likely reflecting increased production by the gut microbiota [53]. | |
| There is also evidence that suggests a difference in endogenous ethanol production in patients with NASH compared to healthy patients. A study published in 2001 by Nair evaluated breath ethanol concentration in human subjects with biopsy proven NASH found small quantities of ethanol in the breath of subjects without recent alcohol consumption [54]. The study also showed that both obese and female subjects were more likely to have higher breath ethanol concentrations [54]. | |
| Finally there is emerging evidence that suggests a difference in the ethanol producing gut microbiota in patients with NASH compared to healthy patients. A study by Zhu evaluated the gut microbiota of human subjects with and without NASH in obese and healthy individuals. The study showed an increased amount of alcohol producing bacteria in the gut microbiota of children with NASH, along with an elevated alcohol level without dietary alcohol consumption [55]. The study also showed that Escherichia was the only abundant genus that differed between NASH and obese patients without NASH. | |
| Microbiota and choline | |
| Choline is an essential water soluble nutrient found in egg yolks and animal sources of protein [56]. It is an important component of cell and mitochondrial membranes and can also be synthesized in the liver [57]. It plays a key role in lipid metabolism, enterohepatic circulation of bile and cholesterol, signaling through lipid second messengers, methylation-dependent biosynthesis of molecules, activation of nuclear membranes, fluidity of plasma membranes and mitochondrial bioenergetics [58]. . | |
| Choline is synthesized in the liver in the form of phosphatidylcholine through a reaction catalyzed by Phosphatidylethanolamine-NMethyltransferase (PEMT) [58]. Phosphatidylcholine the key choline metabolite in the liver is involved in the processing and export of triglycerides in very low density lipoproteins (VLDL) [59]. Defects in the VLDL mediated secretion of triglycerides play a central role in the process of hepatic steatosis [60]. Choline along with folate and methionine all play key roles in the production of S-adenosylmethionine, the methyl group donor in biological reactions [58]. | |
| The role of the liver in the metabolism and storage of choline has led to a better understanding of the development and progression of NAFLD through the use of choline deficient diets in mice models [58]. Choline deficiency in the diet leads to hepatic steatosis and liver damage [61]. A study by Marcolin in 2011 is one of several studies that show that mice fed a choline deficient diet develop weight loss, significantly elevated hepatic enzymes and histologic findings consistent with NASH. The study also showed increased lipoperoxidation and antioxidant enzyme activity in mice fed a choline deficient diet [62]. The hepatic steatosis that results from choline deficiency in the diet has been shown to be reversible with choline supplementation [63]. | |
| Several mice models using deletion of choline related genes like those important for methyl donation (bhmt [64] and cdht [65]), for endogenous production of choline (pemt [66]) and production of S-adenosylmethionine (Mat1 [67]) have also led to the development of NAFLD. Polymorphisms in pemt in humans have also been shown to be associated with NAFLD [68]. | |
| The gut microbiota plays an important role in the metabolism of choline. It produces enzymes that catalyze the first step in the conversion of dietary choline to dimethylamine and trimethylamine [69]. The two byproducts of choline metabolism are absorbed through microvilli and reach the liver via the portal vein where trimethylamine is cleared by first-pass metabolism before entering the systemic circulation [70,71]. The transformation of choline into methylamines decreases the bioavailability of choline, possibly acting as a trigger for NAFLD in mice [72]. In one study, when the 129S6 mouse was fed a high fat-diet, the increased microbial enzyme activity led to decreased bioavailability of choline, with resultant symptoms that mimicked NAFLD caused by a choline-deficient diet [72]. A recent study at our center investigated the utility of breath volatile organic compounds for the diagnosis of NAFLD in obese pediatric patients. Our study showed that breath trimethylamine (among other compounds) was significantly higher in patients with NAFLD compared to healthy patients [73]. This suggests that there is a close link between choline metabolism/bioavailability and the pathogenesis of NAFLD. | |
| Microbiota and TLRs | |
| Pathogen-Associated Molecular Pattern Molecules (PAMPs), Damage-Associated Molecular Pattern Molecules (DAMPs), Nodlike Receptors (NLRs) and Toll-Like Receptors (TLRs): The gut microbiota is important in the development and maintenance of the host’s immune system [74]. Communication between the host and bacteria at the mucosal surface is responsible for the innate and adaptive immune responses that protect the host [75]. Growing evidence suggests that alterations in the gut microbiota leads to increased activation of the innate immune system with subsequent development of NAFLD in both mice and humans [75]. | |
| The alterations in the gut microbiota responsible for the development of NAFLD include bacterial overgrowth, microbiota disequilibrium and release of gut-derived products into the circulation [76]. These gut-derived products include bacterial lipopolysaccharide (LPS), peptidoglycan and bacterial DNA termed pathogen-associated molecular patterns (PAMPs) [76]. PAMPs are diverse set of microbial molecules that alert the host to intruding pathogens [77]. The most studied PAMP is LPS, which is a component of the cell membrane of gram negative bacteria and the active component of endotoxin [47]. | |
| Toll-like receptors (TLRs) are specific pattern recognition receptors that recognize PAMPs and are important in protection of the host [78]. TLRs act as immune sensors of PAMPs and initiate an adaptive immune response and signaling cascade with resultant activation of pro-inflammatory genes [79]. Some of the proinflammatory genes activated include interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-12 (IL-12) and tumor necrosis factor-α (TNF-α) [80]. The mammalian liver expresses eight TLRs including TLRs 1, 2, 4, and 6-10 with different expression levels in hepatocytes, Kupffer cells, hepatic stellate cells, and endothelial cells [81]. | |
| NOD-like receptors are a specialized group of intracellular pattern recognition receptors that also play a key role in the host innate immune response [82]. NLRs are intracellular sensors of PAMPs and damage-associated molecular pattern molecules (DAMPs). DAMPs are molecules that initiate and perpetuate immunity in response to trauma, ischemia and tissue damage in the absence or presence of a pathogenic infection [83]. NLRs act in conjunction with TLRs to regulate inflammatory and apoptotic response. They are expressed in lymphocytes, macrophages, dendritic cells and epithelial cells [84]. A subset of NLRs assemble and oligomerize into a common structure that collectively activates the caspase-1 cascade and leads to the production of pro-inflammatory cytokines like IL-1B and IL-18. This common multi-molecular structure is called an inflammasome [85]. | |
| LPS binds to lipopolysaccharide binding protein (LBP) which, in turn, binds to CD-14. The complex of LPS-LBP-CD-14 subsequently activates TLR-4, which is present in Kupffer cells, triggering an inflammatory cascade involving mitogen and stress activated kinases, interferon regulatory factor 3, Jun N-terminal kinase, p38 and nuclear factor-κB [47,86]. Nuclear factor-κB subsequently translocates into the nucleus and activates the transcription of multiple proinflammatory genes like IL-1β and TNF-α that can induce liver fibrosis and injury [87]. | |
| Studies using animal models have shown a relationship between the LPS-TLR-4 signaling cascade and the development of insulin resistance and NASH. Cani first described a phenomenon known as metabolic endotoxemia where mice fed a high fat diet for 4 weeks were noted to have moderate elevation in plasma LPS concentration [88]. They also showed that a high fat diet phenotype (insulin resistance, increased hepatic triglyceride content and adipose tissue inflammation), resulted from 4 weeks of continuous infusion of LPS in mice [88]. These effects were found to be dependent on CD-14 and reversed in CD-14 knockout mice [88]. The role of the gut microbiota in this process was shown by a reduction in severity of disease in highfat diet and ob/ob mice treated with antibiotics [84,89]. Other studies using TLR-4 null mice (-/-) have shown that TLR-4 is important in the deposition of hepatic fat and development of NASH [90,91]. Recently, Oregui demonstrated that the TLR4 antagonist, JKB 121, decreased hepatic inflammation in response to LPS challenge in animals with MCD-induced NASH indicating a possible protective effect of JKB 121 against liver injury in endotoxemia [92]. HSCs might also play an important role in the liver inflammatory cascade linked with endotoxinemia. They are shown to be the target through which TLR-4 promotes fibrogenesis via enhanced signaling of the transforming growth factor-β (TGF-β) [93,94]. | |
| TLR2 plays a very controversial role in the pathogenesis of NAFLD. There are some studies that show that TLR2 deficiency protects mice from high fat diet induced hepatic steatosis [95,96]. There are other studies that show that loss of TLR2 increased susceptibility to pathogen associated steatohepatitis in the setting of NASH model induced by a choline-deficient diet [97,98]. A recent study by Miura showed that TLR2 is a crucial molecule that promotes liver injury, inflammation and fibrosis in mice fed a choline-deficient amino acid-defined diet that develop NASH, obesity and insulin resistance [99]. This study also showed that TLR2 signaling led to increased expression of pro-inflammatory cytokines and Nod-like receptor protein 3, which is activated primarily in Kupffer cells when TLR2 acts in concert with palmitic acid the most abundant free fatty acid in the plasma of NAFLD. | |
| TLR5 is involved in the development of NAFLD and alteration of the gut microbiota. A study by Vijay-Kumar showed that mice deficient in TLR5 develop hyperphagia, obesity, insulin resistance and hepatic steatosis. The study also showed that subsequent transfer of the gut microbiota of TLR5 deficient mice into healthy mice led to the development of de novo disease confirming the close relationship between the gut microbiota and TLR 5 [100]. | |
| TLR9 is implicated in the development of insulin resistance, steatohepatitis and fibrosis. A study by Miura showed that when TLR9 deficient mice are fed a choline-deficient amino acid-defined diet they develop less insulin resistance, steatohepatitis and liver fibrosis compared to wild type mice. The study also showed decreased production of the inflammatory cytokine IL-1β in TLR9 deficient mice compared to wild type mice. Table 1 summarizes the key findings on the role of TLRs in the development and progression of NAFLD. | |
| Table 1: Role of TLRs in NAFLD. | |
| Finally NLRs also play a role in the pathogenesis of NAFLD. A recent study by Wree examined the effect of persistent NLRP3 inflammasome activation on the development and progression of NAFLD. Gain of function Nlrp3 knock-in mice and loss of function Nlrp3 knockout mice were placed on a choline-deficient amino aciddefined diet for 4 weeks. The study revealed that mice with NLRP3 loss of function were protected from diet-induced steatohepatitis while mice with NLRP3 gain of function developed early and severe onset diet induced steatohepatitis. Wree also assessed liver biopsies of a well characterized group of patients with the full spectrum of NAFLD during the study. The liver biopsies revealed that patients with severe NAFLD expressed higher levels of NLRP3 inflammasome components [101]. | |
| Microbiota and altered intestinal permeability | |
| The intestinal epithelium acts as a barrier to prevent bacterial translocation but, certain exogenous or endogenous events can alter that protective barrier. Factors theorized to promote increased intestinal permeability include alcohol consumption, diet, immobilization stress and radiation [102]. There is also evidence to suggest that the gut microbiota affects intestinal permeability. | |
| A study by Cani published in 2008 showed that ingestion of a high fat diet leads to modulation of the gut microbiota with resultant increased intestinal permeability, through reduction of expression of genes that code for two tight junction proteins zona occludens 1( ZO- 1) and Occcludin. They also showed that obese and high-fat-fed mice recover their normal intestinal epithelial integrity when administered antibiotics [103]. Another study by Cani showed that selective gut microbiota change, controls and increases endogenous glucagonlike peptide-2 (GLP-2) production and results in improved intestinal barrier function [102]. | |
| There is growing evidence that suggests the alteration of intestinal permeability by the gut microbiota leads to an increase in bacterial translocation and small intestinal bacterial overgrowth (SIBO) with resultant disease progression in NAFLD. A study by Miele clearly illustrated the above mentioned theory. Using patients with biopsyproven NAFLD, untreated celiac disease (model for altered intestinal permeability) and healthy controls they showed that patients with NAFLD had significantly increased intestinal permeability and a higher prevalence of SIBO. They also showed that in patients with NAFLD, both the intestinal permeability and prevalence of SIBO correlated with the severity of steatosis [104]. | |
Targeting Microbiota to Treat NAFLD: Probiotics |
|
| Probiotics are live commensal microorganisms that when consumed in adequate quantities, confer a health benefit to the host (FAO/ WHO, 2001). Probiotics have many beneficial effects in NAFLD through different mechanisms including the modulation of microbiota composition, antibacterial substance production, the modification of intestinal barrier function and immune system [105].The major probiotics currently on the market include Bifidobacteria, Lactobacilli and Streptococci [105]. Multiple animal models have shown that probiotics may decrease the progression of NAFLD [106-110]. | |
| The most studied probiotic used in animal models is the VSL#3 mixture. This is a multi-strain mixture composed of Bifidobacterium breve, Bifidobacterium longum, Bifidobacterium infants, Lactobacillusacidophilus, Lactobacillus casei, Lactobacilli delbrueckii subsp bulgaricus, Lactobacillus plantarum and Streptococci thermophilus. Multiple mechanisms have been proposed for the beneficial effects of VSL#3 on NAFLD. For example, when ob/ob mice fed a high-fat diet are treated with VSL#3 for 4 weeks, there is noted improvement in their liver histology, hepatic fatty acid content and serum alanine aminotransferase levels, which is a surrogate marker of NAFLD [106]. There is evidence that VSL# 3 improves hepatic steatosis and insulin resistance by preventing high-fat diet induced natural killer T-cell depletion [107]. Four weeks of treatment with VSL#3 also decreased the high-fat diet induced inflammatory and oxidative liver damage in the experimental mice model of NASH [110]. | |
| Several strains of Lactobacillus have also shown protective effects in NAFLD. Oral administration of Lactobacillus rhamnosus PL60 showed improved liver steatosis and antiobesity effects in a mouse model of diet induced obesity [111]. Lactobacillus paracasei F19 also significantly decreased liver injury induced by ischemia-reperfusion and methionine/choline deficient diet in mice by reducing inflammation and steatosis and restoring gut microbiota [109]. | |
| Preliminary data from human studies show that both VSL#3 and a symbiotic administered to NAFLD patients for 2-3 months improved liver enzymes, oxidative stress markers and TNF-α [112]. Two recent randomized double-blind placebo-controlled studies in humans also showed significant improvement in serum aminotransferases with use of probiotics in children and adults [106,113]. Table 2 summarizes the key findings from various studies evaluating the efficacy of probiotics in the management of NAFLD. | |
| Table 2: Effect of probiotics in NAFLD. | |
Conclusion |
|
| NAFLD is the most common chronic liver disease in the United States. It is strongly associated with obesity, insulin resistance and the metabolic syndrome. Therefore, the current obesity epidemic makes NAFLD a major public health concern. The etiology of NAFLD is not well understood but, there evidence that suggests the gut microbiota may be involved in the pathogenesis of NAFLD. The gut microbiota indirectly contributes to the development and progression of NAFLD through, its role in dietary energy extraction, bile acid metabolism, endogenous alcohol production, choline metabolism, modulation of the host’s immune system and alteration of intestinal permeability. This means that therapy targeted at modulation of the gut microbiota like probiotics would be beneficial in the management of NAFLD. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi