Case Report, J Spine Neurosurg Vol: 12 Issue: 1
Geometric Variability in Radiological Appearance of Third Ventricle in Congenital Hydrocephalus-Is it Really so Pliable? Or Do we Need to Visualize it Differently? A Two-Case Study and Literature Review
Sanjeev Sreenivasan1*, Neha Agarwal2, Prabhu Nath Pandey3 and Gaurav Gupta1
1Department of Neurosurgery, Rutgers University, New Jersey, USA
2Department of Obstetrics and Gynecology, University of Texas McGovern Medical School, Houston, USA
3Department of Neurosurgery, Maulana Azad Medical College, Balmiki Basti, New Delhi
*Corresponding Author: Sanjeev Sreenivasan
Department of Neurosurgery, Rutgers University, New Jersey, USA
Tel: 732-393-2432
E-mail: sa2034@rwjms.rutgers.edu
Received date: 23 August, 2022, Manuscript No. JSNS-22-72662;
Editor assigned date: 26 August, 2022, PreQC No. JSNS-22-72662 (PQ);
Reviewed date: 09 September, 2022, QC No. JSNS-22-72662;
Revised date: 07 February, 2023, Manuscript No. JSNS-22-72662 (R);
Published date: 14 February, 2023, DOI: 10.4172/2325-9701.1000147
Citation: Sreenivasan S, Agarwal NM, Pandey MC, Gupta MDG (2023) Geometric Variability in Radiological Appearance of Third Ventricle in Congenital Hydrocephalus-Is it Really so Pliable? Or Do we Need to Visualize it Differently? A Two-Case Study and Literature Review. J Spine Neurosurg 12:1.
Abstract
Enlargement of third ventricle is seen due to multiple causes, usually associated with hydrocephalus. Raised Intracranial Pressure (ICP) is the most common indication for a cerebrospinal fluid diversion procedure. However, congenital anomalies like Dandy Walker Malformation (DWM) may not always manifest with raised ICP. Identifying neurological delay and neurocognitive parameters and correlating this with existing anatomical features is extremely important. We discuss this report of two cases of patients with DWM where abnormal morphology of the third ventricle was analysed and used to interpret clinical neurological delay.
Keywords: Third ventricle morphometry, Geometric variability, Dandy walker malformation, Hydrocephalus
Introduction
A derivative of the forebrain vesicle, the Third Ventricle (TV) is a slit like region between the two thalami [1]. Superiorly, it communicates with the lateral ventricles through the foramen of Monro and inferiorly with the fourth ventricle via aqueduct of sylvius. Choroid plexus in the TV is the primary source of Cerebrospinal Fluid (CSF) production. Enlargement of TV can see in hydrocephalus due to multiple causes. We present a radiological description and neuro-anatomic correlation of varied appearance of the TV, on Non-Contrast Computed Tomography (NCCT) in two patients with Dandy Walker Malformation (DWM) with hydrocephalus. Through this case study and literature review we intend to highlight the clinical implication of geometric variability, third ventricle morphometry and a potential role for newer imaging modalities in surgical decision making for congenital hydrocephalus. This is the first case study in literature, on morphometry of abnormal third ventricle in DWM.
From October to December 2021, two patients admitted at Maulana Azad medical college and Lok Nayak hospital with radiological diagnosis of DWM were included in this non-interventional study. Informed consent was obtained from the relatives of the infants before inclusion and access to their data. The clinical history like symptoms, duration, neuro-developmental history were recorded. The examination findings were charted and routine preoperative radiological image (NCCT Head) was used for detailed morphometric analysis and description. There was no additional radiation exposure to the patient. The DICOM (Digital Imaging and Communications in Medicine) image was viewed on Radiant DICOM viewer software (Pro Surgical 3D, Medixant, Poland). The screen resolution was kept at minimum 1024 x 768 mm. Third ventricular width, Anteroposterior (AP) length were estimated and recorded. At 3 months follow-up visit in outpatient department, clinical history and neuro-developmental status was recorded again.
Case Presentation
Case 1
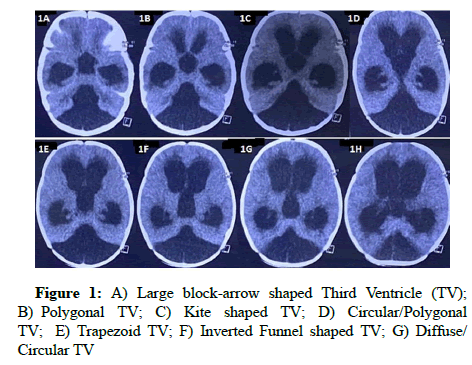
A 6 months male child was admitted with a history of excessive crying for 1 day and multiple episodes of vomiting. Pulse rate was 124/min and blood pressure 92/60 mm Hg. Movement in lower and upper limbs was intact. Anterior fontanelle was tense and bulging. NCCT showed dilated lateral and third ventricles with absence of midline posterior fossa structures and enlarged cisterna magna, suggestive of dandy-walker malformation (Figure 1). He underwent an emergency ventriculo-peritoneal shunt for Cerebrospinal Fluid (CSF) diversion. Symptoms of raised intracranial pressure subsided after shunt procedure. Immediate post-operative NCCT did show any significant change in the dilated TV size or shape. At three month follow up visit, the patient growing at a steady cognitive and functional pace.
Case 2
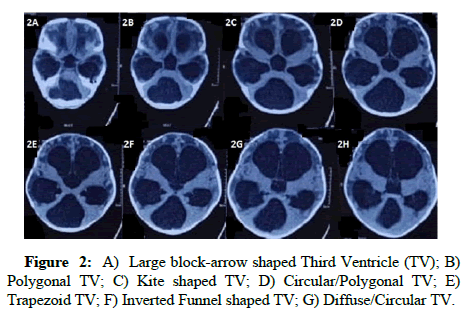
An 8 month male child was admitted with history of incessant vomiting for 2 days. Pulse rate was 101/min and blood pressure was 88/56 mm/Hg. Compared to upper limbs, there was paucity of lower limb movements. The anterior fontanelle was tense. NCCT head showed similar dilatation of bilateral lateral ventricles and third ventricle. Atrophy of bilateral cerebral parenchyma was noticed, along with intense periventricular ooze. Evidence of DWM was seen on the NCCT scan (Figure 2). After a ventricul operitoneal shunt procedure, his symptoms of raised intracranial pressure subsided. At follow up visit, he was neurologically stable with slow and steady clinical progress.
Imaging appearance and neuro-anatomic correlation
In the caudal section of NCCT head, the TV appears like a large block arrow with a triangular head. The anterior wall of TV is formed by Lamina Terminalis (LT). Fibres of Anterior Commissure (AC) cross this structure of gray matter to connect the temporal lobes of both hemispheres. Extreme dilatation of TV seen in subsequent sections of NCCT, represent longitudinal stretching of AC fibres and thinning out of LT. Extension of the anterior recesses of third ventricle into suprasellar cistern causes a rounded contour [2]. Abnormal shape of anterior wall of TV has been reported in malformations of neurohypophysis [3]. The lateral wall of TV is formed by hypothalamus inferiorly and thalamus superiorly. Stretching of the TV causes thinning of hypothalamus and thalamus and medial temporal horn including uncus seem to be affected most. The shape of TV changes from large block arrow in to polygonal shape in 1b and kite/ diamond shape. We notice maximum pliability of the anterior wall as compared to lateral and posterior walls. The lateral wall in its anterior extent seems to be displaced farther than its posterior extent. Proximity to temporal horn and tentorium lower the tendency of deformation of posterior wall and posterior portion of lateral wall of TV. From below upwards, posterior wall of TV is comprised of posterior commissure, pineal recess, pineal body and habenular commissure. The appearance of posterior wall also changes vastly from a rectangular block to butterfly appearance and back to a rectangular block. As part of the DWM, brainstem appears to be thinned (Figure 1).
Superior wall of TV is formed by tela choroidea containing the internal cerebral veins, fornix and corpus callosum. Extreme thinning of corpus callosum represents longitudinal stretching of these callosal fibres. Abnormal contour of the TV has been reported in callosal dysgenesis too. Inferior wall of TV is formed by optic chiasm, tuber cinereum, infundibulum and mammillary bodies. The thinned tegmentum of midbrain lies posterior to these structures. Extension of floor of TV into the prepontine cistern produces a broader appearance at the base.
The NCCT head of case 2 is demonstrated in Figure 2. In order to maintain homogeneity in radiological measurement, all images have been selected at corresponding cut sections in both patients. The morphometric assessment of both patients in highlighted in Table 1. We noticed one measurement could represent the maximum dimension of TV. Two separate dimensions were estimated at the closest and farthest points of lateral wall of TV. The AP length was estimated in all the sections.
Discussion
We notice uniform increase in TV width and length measurements compared to normal patients mentioned in literature. This is attributed to the congenital malformation (DWM) seen in our cases. Patients with DWM usually have delayed neuro-cognitive development which is incompatible with life in many cases. Ocular signs seen in such patients include conjugate gaze palsy, convergence-retraction nystagmus etc. Long tract signs like upper or lower limb weakness arise due to brainstem compression. These are commoner than early onset cognitive dysfunction and hypothalamic disorders. A possible explanation of this clinical disparity could lie in the radiological finding elicited in our study. The TV distance between anterior regions of third ventricle is lesser than that between posterior regions. The pineal recess and posterior third ventricular region are closely associated with midbrain structures. This produces the early ocular and long tract involvement. Lesser compression on hypothalamic and thalamic structures early in the disease course explains the lower incidence of corresponding symptoms. An increase in length of TV in DWM compared to normal needs further evaluation. The anterior wall of TV carries significant temporal interconnecting fibres. These can be analysed through a white matter tractography and there relation to various cognitive and memory deficits need to be studied in detail.
Importance of morphometry: Surgical significance of third ventricle stems from its close relation with fornix and thalamus. The antero-ventral TV receptors play an important physiological role in regulating fluid hemostasis and the TV also contributes to satiety control in infants. There is paucity of literature on significance of morphometric analysis of third ventricle and its relation to clinical and physiological functioning. Patnaik demonstrated non-significant correlation of third ventricle width with age. Third ventricle sylvian fissure index tends to decrease with age and third ventricle width, while there was no correlation between age and third ventricle ratio. No significant gender difference in width of TV could be achieved while antero-posterior length varied significantly between males and females of similar ages [4-6]. It has been seen that increase in size of third ventricle with age is statistically significant among women. It was also noted that third ventricle was larger in men, than women [7-10]. Muller et al reported that width of TV in Multiple Sclerosis (MS) patients increased with age, expandeddisability status scale EDSS, (Spearman rho, r=0.446, p<0.005) and duration of MS (r=0.319, p<0.005). Schimmel et al reported patients with Down’s syndrome had increased width and length of third ventricle despite a small head circumference [11]. They also postulated a link between increased third ventricle dimensions and cognitive and neuropsychological sequelae. However conclusive evidence remains to be found. In literature, the mean width of third ventricle has been reported to vary from 2.25 mm to 9.2 mm [12,13]. In a cadaveric study by Satapara, twenty cadaveric brains were studied by luminal cast plastination method and compared with 63 MRI scans. They concluded that mean width of third ventricle was same (0.52 cm) among males and females and mean width of third ventricle increases with age. In our case study, the width of third ventricle was variable. In maximum width measures 35 mm. TV (min/max) gradually decreases (Table 1).
| Case 1 | Case 2 | |||||
|---|---|---|---|---|---|---|
| Image | Width | AP length | Width | AP length | ||
| 1a | 35 | 48 | 40 | 35 mm | ||
| 1b | 35 | 43 | 37 | 38 mm | ||
| 1c | 35 | 43 | 36 | 38 mm | ||
| 1d | 36 | 47 | 36 | 35 mm | ||
| 1e | 34 | 49 | 37 | 35 mm | ||
| 1f | 32 (min) | 35 (max) | 54 | 33 (min) | 36 (max) | 36 mm |
| 1g | 30 (min) | 34 (max) | 48 | 32(min) | 37(max) | 37 mm |
| 1h | 34 (min) | 34 (max) | 30 | 33 (min) | 37(max) | 35 mm |
| Note: *All measurements are in mm. | ||||||
Table 1: Morphometry of third ventricle in CT scan of our case study.
Geometric variability: We studied the geometric variability of third ventricle in patients with DWM. The appearance of TV depends on the compressibility of surrounding structures. Neurological deficits usually represent a manifestation of compression of these structures. Similar geometric patterns need to be studied in other congenital malformations pertaining to hydrocephalus. This will enable us identify patients which need elective cerebrospinal fluid diversion procedure when signs of raised ICP are absent.
Clinical implication: Neonates with congenital hydrocephalus often have a stormy course after birth. Need of CSF diversion procedures like ventriculo peritoneal shunt and complications associated with shunts are quite common in children. Neurological weakness, gait instability, delayed cognitive development and seizures are some important sequelae of congenital hydrocephalus. We notice thinning and pliability of multiple structures lining the third ventricle wall in anterior, lateral, posterior and inferior aspects. These patients often manifest with cognitive delay, gait instability, thalamic and hypothalamic imbalances. The stretching of periventricular structures may cause possible neuropraxia like effects. A white matter tractography imaging with functional sequencing are required to better identify molecular changes within these pathways surrounding the third ventricle. Reversal of symptoms and radiological changes, following CSF diversion procedure usually depends on the extent of neurological injury present at onset/clinical presentation.
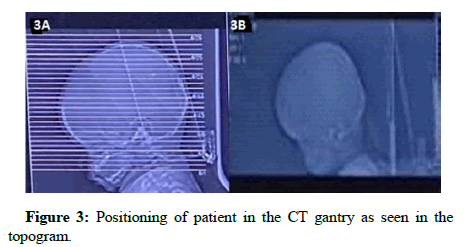
Reason for morphological variability: One of the main reasons for variable appearance of a dilated TV is pliability of peri-ventricular structures. Stretching of the white matter tracts and obliteration of peri-ventricular recesses and cisternal spaces contribute to this phenomena. Another possible mechanism could be the positioning of patient’s head inside the CT gantry. We can note in the direction of cut-section lines used to generate a final tomography image. The trajectory of radiological cut lines as they traverse the periventricular recesses plays a critical role in determining the appearance of TV. The orientation of sagittal and coronal plane of head inside the CT console will determine the shape of any intracranial structure seen on imaging. Aqueductal stenosis may cause dilatation of TV and hydrocephalus. Depending on severity of stenosis, it may manifest at any age. In hydrocephalic adults, 10% of cases are due to aqueductal stenosis. Sellar-suprasellar masses which may be hypothalamic, pituitary or chiasmatic in origin, are the most common pathological processes. Lesions of pineal gland, tectal plate and inferior thalamus may deform the posterior portion of TV (Figure 3).
Clinical correlation: Dilatation of TV can manifest with symptoms of pressure over the adjacent neurological structures or pathological lesions in nearby structure can produce TV dilatation due to aqueductal obstruction. These may manifest with upgaze palsy, convergence retraction nystagmus, absent pupillary light reflex. Involvement of interstitial nucleus of Cajal and rostral interstitial nucleus of medial longitudinal fasciculus produces conjugate upgaze palsy. Involvement of supranuclear fibres of midbrain by the lesion causes persistent irregular jerky nystagmus (convergence retraction). Involement of Edinger-Westphal nucleus causes asymmetric pupillary reaction to light with a preserved accommodation reflex. An occlusion of third ventricular outflow can cause dilatation of periventricular recesses. Dilatation of pineal recesses and compression of posterior commissure may be associated with the above mentioned signs. Dilated suprasellar cistern can compress the optic chiasma and produce visual field deficits. Raised intracranial pressure associated with primary hydrocephalus can produce papilledema in adults and older children with fused fontanelles. The antero-ventral region of TV contains the Organum Vasculum of Lamina Terminalis (OVLT), which is a circumventricular organ. It is responsible for maintaining fluid and electrolyte balance in the body by excreting sodium, modulating thirst and regulating blood volume. Diabetes insipidus has been reported secondary to hydrocephalus from multiple etiologies. The principle mechanism of excretion of dilute urine in this condition is deficiency of vasopressin. The malfunctioning of magnocellular nerve terminals of posterior pituitary is the prime culprit in central diabetes insipidus. It is seen that maintained pressure over pituitary stalk can destroy these magnocellular neurons [14]. Usually, this phenomena is reversible unless 80% of the neurons have been damaged [15]. The close relation of hypothalamus with floor and antero ventral third ventricle wall predisposes to diabetes insipidus in long standing hydrocephalus.
Functional significance: The knowledge of pattern of neurological involvement is important in predicting recovery and thus carries prognostic significance. Since periventricular gray and white matter structure are affected by the pathological process of third ventricular dilatation. Extent of damage of these fibres may be studied by white matter tractography imaging. Certain children may present with tense fontanelles with intermittent self relaxation. This subset of patients may not need immediate CSF diversion procedure. It will be prudent to perform a Magnetic Resonance Imaging (MRI) with white matter tractography in them. Diffusion Tensor Imaging (DTI) has been used to study the changes in corpus callosum and corona radiata in series of hydrocephalic patients. It has been noted that before surgery, diffusion parallel to corona radiata fibres was increased and perpendicular diffusion was decreased. This manifested as an increment in Fractional Anisotropy (FA). The FA values normalized after surgery. In corpus callosal fibres, the FA values were lower in hydrocephalic patients than controls and this remained same after surgery [16]. Since DTI has a potential role in documenting compression changes in white matter tracts, this sequencing needs to be applied to periventricular fibres adjacent to the TV. In patients where hydrocephalus seems arrested or raise in intracranial pressure is intermittent, a plain CT scan may not estimate ongoing neuronal damage.
At some centres, infants with equivocal clinical signs of intracranial pressure may be deferred a cerebrospinal fluid diversion procedure, as they may not have acute raise in ICP or imminent vomiting and headache. However, in the presence of significant changes of white matter tracts on DTI imaging and corroborative FA values, a CSF diversion procedure may be deemed necessary. This can help in early identification of infants with congenital intracranial malformations who need imminent CSF diversion. Raised ICP may not be the only indicator of congenital hydrocephalus. It becomes imperative to identify patients who have neurological sequelae like cognitive deficit, ocular signs and symptoms without impending raised ICP. Since production and absorption of CSF is a dynamic process, a CSF diversion procedure is definitely required at some point of time during the disease. However, other neurological deficits may become irreversible once they cross a certain threshold of quantitative neuronal damage. Timely intervention will abate permanent neuronal damage and this segment of population will benefit from diffusion tensor imaging. Agenesis of several structures contributes to appearance of dilated ventricles on CT scan. As ventriculomegaly in such cases may be an ex-vacuo phenomena and to differentiate between radiological ventricumegaly and pathological hydrocephalus, DTI imaging can very well provide substantiative evidence at a molecular level.
Conclusion
Through this case study and literature review we intend to highlight the importance of third ventricle morphometry, its geometric variability and need of DTI sequencing in subset of patients with congenital hydrocephalus. Hydrocephalus is one of the most perplexing conditions which confront a pediatric neurosurgeon. Several long term sequelae of congenital hydrocephalus have been described. Although timely treatment of raised ICP is imperative in preventing these sequelae, it should not be considered the only indication of CSF diversion in such patients. Apart from clinical judgment and basic (CT) radiological correlation, there are no strict guidelines for time of surgical intervention. DTI of periventricular tracts adjacent to third ventricle may supplement our radiological armamentarium and aid surgical decision making.
Acknowledgements
None
Conflict of Interest
None
References
- Standring S, Borley NR, Coliins P, Crossman AR, Gatzoulis MA, et al. (2008) Gray‚??s anatomy, the anatomical basis of clinical practice; chapter-16 ventricular system and subarachnoid space, chapter-24 development of nervous system. 40th edition. Spain. 237-240.
- Satapara VK, Patel MM, Rathava JK, Trivedi PN, Kukadiya UC, et al. (2014) Morphometry of width of third ventricle of brain by luminal cast plastination and MRI. Int J Ad Res 2:837-842.
- Glastonbury CM, Osborn AG, Salzman KL (2011) masses and malformations of the third ventricle: normal anatomic relationships and differential diagnoses. RadioGraphics 31:1889-1905. [Crossref] [Google Scholar] [PubMed]
- Usman JD, Zagga AD, Tadros AA, Yunusa G, Saidu SA, et al. (2013) Morphological variation of third ventricle using computerized tomography among different gender and age groups: A 5-year retrospective study in Usmanu Danfodiyo University Teaching Hospital, Sokoto, North-West Nigeria. Sahel Med J 16:83-86. [Google Scholar]
- Celik HH, Gurbuz F, Erilmaz M, Sancak B (1995) CT measurement of the normal brain ventricular system in 100 adults. Kaibogaku zasshi 2:107-115. [Google Scholar] [PubMed]
- Muller M, Esser R, Kutter K, Voss J, Muller A, et al. (2013) Width of 3. Ventricle: Reference values and clinical relevance in a cohort of patients with relapsing remitting multiple sclerosis. Open Neurol J 7:11-16. [Crossref] [Google Scholar] [PubMed]
- Mathew L, Paul MM, Bakshi SS (2012) assessment of third ventricle with mri: morphological variations among different gender and age group. Webmed Central Anatomy 3:1-10. [Google Scholar]
- Patnaik P, Singh V, Singh D, Singh S (2015) Gender related differences in third ventricle parameters with correlation to cerebrum size -a study on head ct scans. int J Health Sci Res 5:140-147.
- Usman JD, Zagga AD, Tadros A, Yunusa GH, Saidu SA, et al. (2013) Morphological variation of third ventricle using computerized tomography among different gender and age groups: A 5-year retrospective study in Usmanu Danfodiyo University Teaching Hospital, Sokoto, North-West Nigeria. Sahel Med J 11:83-85. [Crossref] [Google Scholar]
- LeMay M (1984) Radiologic changes of the aging brain and skull. Am J Roentgenol 2:383-389. [Crossref] [Google Scholar] [PubMed]
- Schimmel MS, Hammerman C, Bromiker R, Berger I (2006) third ventricle enlargement among newborn infants with trisomy 21. Pediatrics 117:e928-e931. [Crossref] [Google Scholar] [PubMed]
- Benedict RH, Bruce JM, Dwyer MG, Abdelrahman N, Hussein S, et al. (2006) Neocortical atrophy, third ventricular width and cognitive dysfunction in multiple sclerosis. Arch Neurol 63:1301-1306. [Crossref] [Google Scholar] [PubMed]
- Soininen H, Puramen M, Riekkinen PJ (1982) Computed tomography findings in senile dementia and normal ageing. J Neurol Neurosurg Psychiatry 45:50-54. [Crossref] [Google Scholar] [PubMed]
- Dohanics J, Hoffman GE, Smith MS, Verbalis JG (1992) Functional neurolobectomy induced by controlled compression of the pituitary stalk. Brain Res 575:215-222. [Crossref] [Google Scholar] [PubMed]
- Loh JA, Verbalis JG (2007) Diabetes insipidus as a complication after pituitary surgery. Nat Clin Pract Endocrinol Metab 3:489-494. [Crossref] [Google Scholar] [PubMed]
- Assaf Y, Ben-Sira L, Constantini S, Chang LC, Beni L (2006) Adani Diffusion tensor imaging in hydrocephalus: initial experience. Am J Neuroradiol 27:1717-1724. [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi