Research Article, J Surg Clin Pract Vol: 1 Issue: 1
Fatal Hyperammonemic Encephalitis Following Gastric Bypass
Hussain AA1*, Abadiano S2 and EL-Hasani SS3
1Department of General Surgery, Doncaster Royal Infirmary, DN2 5LT, Doncaster, UK
2Chelsfeild Park Hospital, Orpington, UK
3Kings College Hospital, London, UK
*Corresponding Author : Dr. Abdulzahra A Hussain
Department of General Surgery, Doncaster Royal Infirmary, DN2 5LT, Doncaster, UK
Tel: 0044-1302366666
E-mail: abdulzahra.hussain@nhs.net
Received: July 18, 2016 Accepted: January 18, 2017 Published: January 26, 2017
Citation: Hussain AA, Abadiano S, EL-Hasani SS (2017) Fatal Hyperammonemic Encephalitis Following Gastric Bypass. J Surg Clin Pract 1:1
Abstract
Background: To report a fatal condition following commonly performed gastric bypass surgery for obesity and metabolic syndrome.
Methods: 62 years old patient underwent gastric bypass surgery in 2014. She had lost significant amount of weight. She had no complications following her surgery. She had been recently admitted to another hospital with coma and died there.
Results: Investigation of her death and post-mortem study confirmed hyperammonemic encephalitis.
Conclusion: Awareness and early treatment of this rare condition may prevent high mortality.
Keywords: Hyperammonemic encephalopathy; Roux en-Y gastric bypass; Bariatric surgery; Ureagenesis; Urea cycle; Intensive care unit
Introduction
Hyperammonemic encephalopathy [HAE] was reported earlier by Mitchell et al. in 1988 [1], and its relation to the blood diseases was confirmed by several authors [2-4]. The association of the syndrome with bariatric surgery was first reported by Ferves et al. in 2008. They reported 5 women, 3 months to 28 years following Roux en-Y gastric bypass (RYGBP) procedures and concluded a combination of hyperinsulinemia and zinc deficiency brought on by RYGBP may have contributed to unmask ornithine trans- carbamylase deficiency in these 5 patients [5]. An additional 22 cases of HAE following bariatric surgery were reported [5-8]. This condition was also diagnosed in children following urinary tract infection with urease-producing organism [9]. Moreover, it was reported following cancer, liver disease, congenital enzymatic deficiency and urea cycle disorders [10-13].
The aim of this paper is to highlight the importance of the syndrome, the spectrum of the problem, how many case reports to date, is it specific for gastric bypass and how to prevent it or screen for it?
Case Summary
62 years female patient underwent laparoscopic Roux en-Y gastric bypass (150 cm alimentary limb and 200 cm bilio-pancreatic limb) in January 2014. Her preoperative weight was 154.2 kgs, BMI 56.9 kg/m2. Last follow up was in September 2014 weight 102 Kg.
And her BMI was 37 kg/m2. She was admitted on November 2015 to another hospital with vague symptoms of weakness, dizziness, confusion, convulsion and subsequent coma. The Haemoglobin was 11.2 gm/dl. Liver function tests were deranged while ultrasound of the abdomen showed fatty liver but it is normal in size and shape and no biliary obstruction.
Results
Results of ammonia level was significantly raised during the admission between 26th and 30th November with levels of 226, 286, 105,92 and 125 recorded against normal level of 0-60 μmol/L. Post mortem histology examination of the brain showed some cerebral oedema, astrocyte swelling and patchy neurone degeneration, all consistent with secondary effects of hyperammonemia. No meningoencephalitis or other evident pathology. The post-mortem study also showed pneumonia and significant level of hepatic steatosis, without any great or significant degree of portal tract fibrosis and no evidence of any other readily identifiable hepatic pathology.
Results: the patient died in spite of supportive intensive care unit measures.
Discussion
Post bariatric surgery HAE is a rare syndrome with 50% mortality [7]. The reason why this syndrome happens after bariatric surgery is yet to be confirmed, and likely to be related to malnutrition or malabsorption mechanisms. Over 75% of carnitine, an important factor in the normal urea cycle is produced by dietary protein [14]. Any protein malnutrition [which could be an aftermath of aggressive bariatric procedures] then is a potential cause. Liver is compensating for inadequate carnitine, however in complex malnutrition status and liver diseases, abnormality in the urea cycle and symptomatic or a symptomatic hyperammonemia may arise. The urea genesis inhibition is found in majority of patients reported by Fenves et al. study [7]. It is therefore logical to assume pre-existing liver disease is to be taken in consideration when decision of bariatric surgery is to be made.
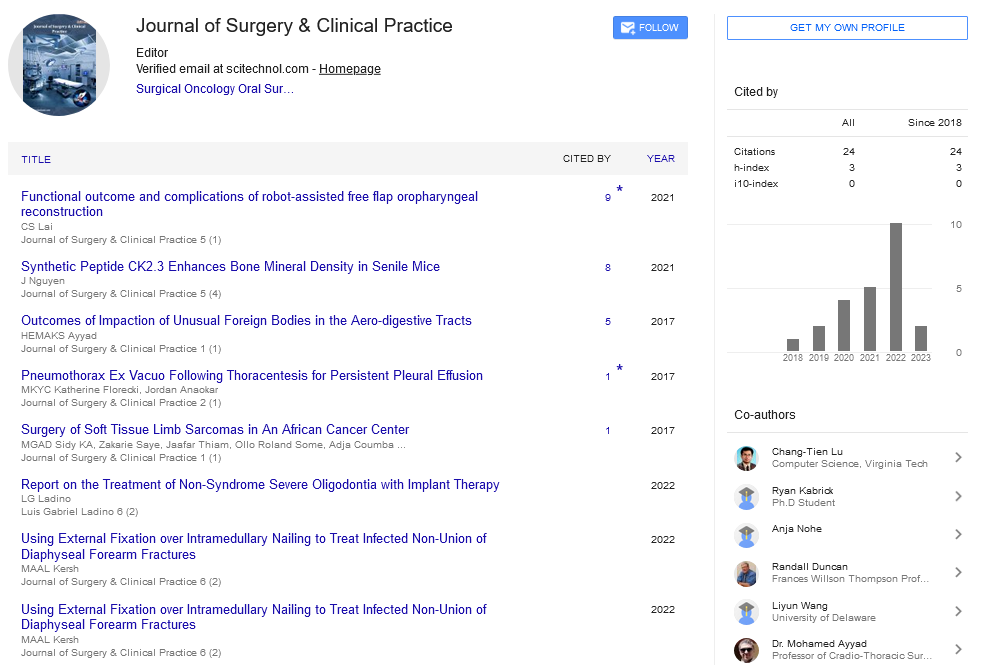
There were 26 previously reported cases of HAE [7], all reported following RYGBP, however the syndrome, may not be specific for RYGBP and possibly caused by other bariatric intestinal diversions that results in protein malnutrition especially biliopancreatic diversion and various ileal bypasses operations that involve short common limb. The unawareness of the condition is probably the reason of under-reporting following these kind of procedures.
The possible predisposing factors for HAE are female gender and successful gastric bypass surgery, but other factors may be associated with the syndrome (Table 1).
| Factor | % of Affected patients |
|---|---|
| Female gender | 96.29% |
| Success of bariatric surgery | 100% |
| Gastric bypass | 100 |
| Pre-existing liver disease including enzymatic deficiency | 22% |
| Hypoglycemia | 37% |
| Low Zinc level | 33% |
Table 1: Predisposing factors for hyperammonemic encephalopathy after bariatric surgery.
The established syndrome is treated with supportive measures [may be at intensive care unit] in addition to oral lactulose, arginine infusion, sodium phenylbutyrate, oral citruline, zinc and caloric and protein intake adjustment [7]. Computarised tomography [CT] scan may show the common imaging finding of symmetric involvement of the cingulate gyrus and insular cortex [15]. In our case no such finding was reported in the CT.
The lesson from this case was patients who are not doing well after aggressive bariatric surgery should be subjected to sophisticated investigations including nutritional parameters, electrolytes and biochemistry, ammonia and urea cycle parameters and carnitine levels. Early detection and treatment may be the only measure to prevent mortality.
Conclusion
Hyperammonemic encephalopathy is a lethal complication following gastric bypass. Patients who underwent gastric bypass and are high BMI and of pre-existing liver disease need follow up investigations including ammonia level.
Reprint Statement
Reprint won’t be ordered.
Financial Support used for the Study
No financial support for this study.
Conflict of Interest Declaration
Authors declare no conflict of interest.
References
- Mitchell RB, Wagner JE, Karp JE (1988) Syndrome of idiopathic hyperammonemia after high-dose chemotherapy: review of nine cases. Am J Med 85: 662-667.
- Kwan L, Levitt L (2002) Hyperammonemic Encephalopathy in Multiple Myeloma. N Engl J Med 346: 1674-1675
- Otsuki T, Yamada O, Sakaguchi H (1998) In vitro excess ammonia production in human myeloma cell lines. Leukemia 12: 1149-1158.
- Martinelli G, Peccatori F, Ullrich B, Ghielmini M, Roggero E, et al. (1997) Clinical manifestation of severe hyperammonaemia in patients with multiple myeloma. Ann Oncol 8: 811-811.
- Andrew Fenves, Richard Boland, Rita Lepe, Paulino Rivera-Torres (2008) Stuart Jon Spechler Internal medicine. Fatal Hyperammonemic Encephalopathy After Gastric Bypass Surgery 121: e1-e2.
- Estrella J, Yee B, Wicken M, Tachan, Mtalbott (2014) Hyperammonemic encephalopathy complicating bariatric surgery. SOARD10: E35-E38.
- Fenves AZ, Shchelochkov OA, Mehta A (2015) Hyperammonemic syndrome after Roux-en-Y gastric bypass. Obesity (Silver Spring) 23: 746-749.
- Hu WT, Kantarci OH, Merritt JL (2007) Ornithine transcarbamylase deficiency presenting as encephalopathy during adulthood following bariatric surgery. Arch Neurol 64:126-128.
- Laube GF, Superti-Furga A, Losa M, Büttiker V, Berger C, et al. (2002) Hyperammonaemic encephalopathy in a 13-year-old boy. Eur J Pediatr 161: 163-164.
- Özçay F, Bar├?┬▒├?┬? Z, Moray G, Haberal N, Torgay A, et al. (2015) Report of 3 Patients With Urea Cycle Defects Treated With Related Living-Donor Liver Transplant. Exp Clin Transplant 3:126-130.
- Lee S, Cheong J, Kim C, Kim JM (2015) Valproic Acid-Induced Hyperammonemic Encephalopathy as a Cause of Neurologic Deterioration after Unruptured Aneurysm Surgery. J Korean Neurosurg Soc 58: 159-162.
- Maruyama M, Miyasaka Y, Takano A, Inoue M, Furuya K, et al. (2015) A case of advanced rectal cancer with rectovesical and ileal fistulae that developed hyperammonemic encephalopathy. Surg Case Rep 24: 1-88.
- Hawkes ND, Thomas GA, Jurewicz A, Williams OM, Hillier CE, et al. (2001) Non-hepatic hyperammonaemia: an important, potentially reversible cause of encephalopathy. Postgrad Med J 77: 717-722.
- Rebouche CJ (2004) Kinetics, pharmacokinetics, and regulation of L-carnitine and acetyl-L-carnitine metabolism. Ann N Y Acad Sci 1033: 30-41.
- U-King-Im JM, Yu E, Bartlett E, Soobrah R, Kucharczyk W (2011) Acute hyperammonemic encephalopathy in adults: imaging findings. AJNR Am J Neuroradiol 32: 413-418.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi