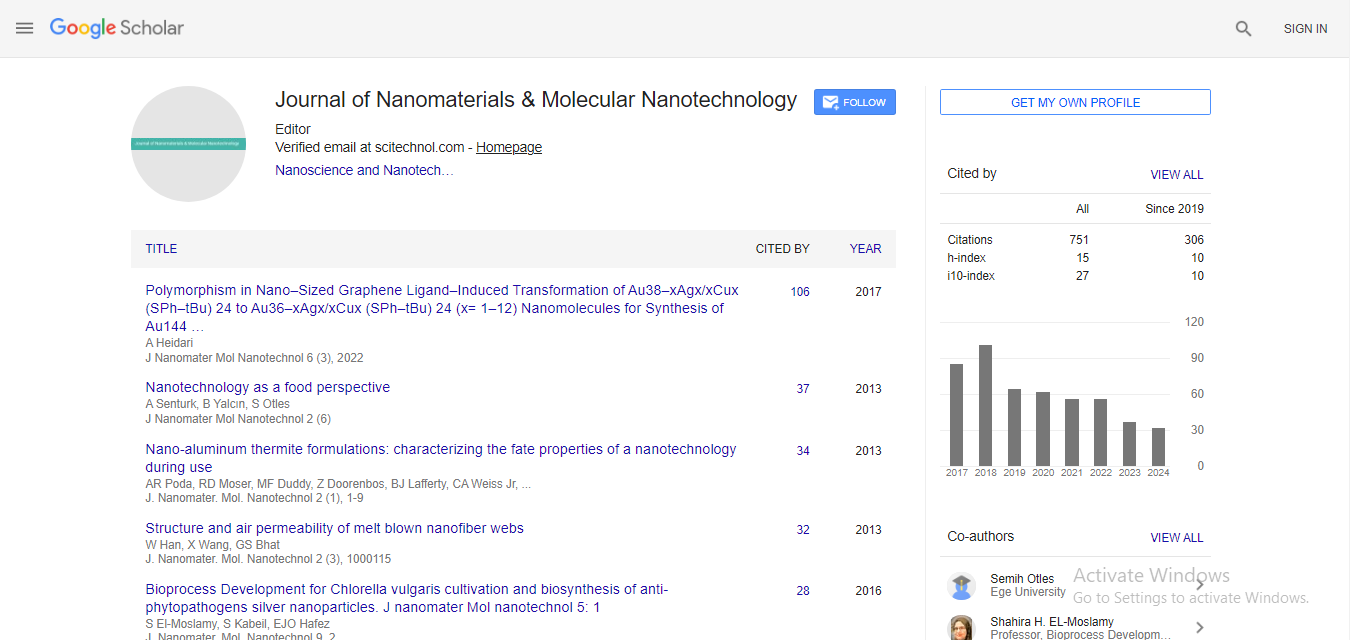
Short Article, J Nanomater Mol Nanotechnol S Vol: 0 Issue: 2
Evaluation of PLGA Nanoparticles Carrying Leukaemia Inhibitory Factor for Stromal-Like Support of Rat Fetal Dopaminergic Cells
| Sean Dyson1, Tarek M Fahmy2, Su M Metcalfe1* and Roger A Barker1 | |
| 1John van Geest Centre for Brain Repair, Addenbrookes Hospital, University of Cambridge, Cambridge, UK | |
| 2Department of Biomedical Engineering, Yale University, Malone Engineering Center, 55 Prospect Street, New Haven, CT 06511, USA | |
| Corresponding author : Dr. Su M Metcalfe John van Geest Centre for Brain Repair, Addenbrookes Hospital, University of Cambridge, Cambridge, UK Tel: 00 4 (0) 1223 570716; Fax: 00 4 (0) 1223 247744 E-mail: smm1001@cam.ac.uk |
|
| Received: April 24, 2014 Accepted: June 16, 2014 Published: June 20, 2014 | |
| Citation: Dyson S, Fahmy TM, Metcalfe SM, Barker RA (2014) Evaluation of PLGA Nanoparticles Carrying Leukaemia Inhibitory Factor for Stromal-Like Support of Rat Fetal Dopaminergic Cells. J Nanomater Mol Nanotechnol S2:003. doi:10.4172/2324-8777.S2-003 |
Abstract
Evaluation of PLGA Nanoparticles Carrying Leukaemia Inhibitory Factor for Stromal-Like Support of Rat Fetal Dopaminergic Cells
After Alzheimer’s disease, Parkinson’s Disease (PD) is the second most common progressive neurodegenerative disease of the CNS. This currently incurable condition is characterised by the loss of dopaminergic neurons in the substantia nigra of the ventral midbrain. New cell-based treatments for PD aim to reintroduce healthy dopaminergic (DA) cells to replace the lost dopaminergic input to the striatum which underlies many of the motor, and some of the cognitive, features of this disease. However, a critical step in this process is the survival and integration of the grafted dopaminergic neurons, and by virtue of the process involved in this therapeutic approach, the cells lack both stromal and growth factor support and are acutely vulnerable to ischaemic stress and an innate immune response: furthermore, endogenous immune tolerance needs to be guided to accept the graft as “self” if rejection is to be avoided. In all these respects, nanotechnologies offer a unique solution and here we outline some fundamental biological considerations relevant to cell based therapies for PD.
Keywords: Parkinson�s Disease; Nanotherapy; LIF
Keywords |
|
| Parkinson’s Disease; Nanotherapy; LIF | |
Introduction |
|
| Nanotechnology holds great promise in therapeutic medicine [1] by enabling three highly desirable therapeutic aims: (i) targeted cargo delivery; (ii) the option to exploit endogenous regulatory and reparative systems via targeted manipulation; and (iii) the potential to create a surrogate biological niche able to support endogenous repair or cell-based therapies, including use of biodegradable synthetic biomaterials as an instructive extracellular microenvironment. For neurodegenerative diseases the need to gain access across the impermeable blood-brain barrier (BBB) is an issue, and similopiodmodification of poly(lactic-co-glycolic acid) (PGLA) nanoparticles (NP) able to transit via the opiod receptor is a option being developed by Tosi and co-workers [2-4]. In Parkinson’s Disease (PD), the disease process critically involves nigrostriatal dopaminergic (DA) neurons resulting in their loss with decreased dopamine levels in the dorsal striatum [5]. It has been shown that clinical transplantation of cells of human fetal ventral mesencephalon (hfVM) tissue, where the dopaminergic precursor cells originate, provides significant long-term benefits in some patients with PD [6]: here the current TransEuro clinical trial aims to improve outcome since results have previously been varied: moreover, the whole approach has significant ethical and practical problems. As an alternative to hfVM, in the future donor DA cells may be derived from human embryonic stem cells; or from dedifferentiated/ re-differentiated pluripotent stem cells [7] where, for clinical use, the numbers of lineage-committed cells will need to be expanded and maintained to retain sufficiency for functional recovery following engraftment. A critical outstanding issue in this regard is the support of these cells both during processing and following grafting. Currently, hfVM-derived DA cell grafting is associated with significant cell death within the cell preparation and especially the midbrain dopaminergic cells of which around 80-90% are lost in the generation of the cells for grafting [6]. In this paper we show that creating a transient surrogate stroma composed of PLGA nanoparticles able to deliver a cargo of the reparative, tolerogenic cytokine leukaemia inhibitory factor (LIF) directly to DA cells is able to improve dopaminergic cell survival. As such, LIF-nano represents a synthetic stroma able to be attached to cells in suspension, and suitable for use as cell/stroma grafts. Specifically, we used rat fetal ventral mesencephalic tissue (that contains the developing nigral dopaminergic cells) to model the clinical procedure, and to test the therapeutic potential of biodegradable PLGA nanoparticles for targeted delivery of LIF. Notably, PLGA is FDA approved and LIF is a naturally occurring cytokine, and our approach is both viral-free and drug-free, with immediate clinical relevance for cell-based therapies for PD. | |
| We selected LIF as the NP cargo because LIF supports tissue repair at physiological doses, and plays a major role in tissue homeostasis by supporting tissue stem cells and progenitor cells [8,9]. In addition clinical trials of recombinant human LIF showed good tolerability without serious side effects [10,11] and also has the added advantage that it can promote Treg [12] which brings with it a level of immune self-tolerance, a desirable property for tissue integration of grafted cells. Since therapeutic exploitation of soluble LIF is hindered by its rapid degradation we had previously developed a nano-particulate PLGA-based formulation “LIF-nano” [13]. Using this LIF-nano we have shown that it can guide immune tolerance to grafted spleen cells in vivo [13] and in the current study we asked if LIF-nano might also be therapeutic for DA cell grafts in PD. We found that LIF-nano targeted to DA cells provided significant pro-survival effects in vitro in the absence of unwanted off-target effects. | |
Materials and Methods |
|
| LIF-Nano | |
| Mouse recombinant LIF (Santa Cruz; SC-4378) was encapsulated in avidin-coated poly(lactic-co-glycolic acid (PLGA) nanoparticles using a modified version of a previously described water/oil/water double emulsion technique [13]. Briefly, 50 μg LIF was dissolved in 200 μL PBS and added dropwise with vortexing to 100 mg PGLA in 2 ml dichloromethane. The resulting emulsion was added to 4 ml of aqueous surfactant solution containing 2.5 mg/ml polyvinyl alcohol and 2.5 mg/ml avidin-palmitate bioconjugate and sonicated to create an emulsion containing nano-sized droplets of polymer/solvent, LIF and surfactant. Solvent was removed by magnetic stirring at room temperature; hardened nanoparticles were then washed three times in deionised water and lyophilized for long-term storage at -80°C. Nanoparticle size and morphology were analyzed via scanning electron microscopy and a Nanosight imaging/sizing system. | |
| Release of LIF was measured by incubating particles in phosphate buffered saline (PBS) at 37ºC and measuring LIF concentrations in supernatant fractions by enzyme-linked immunesorbant assay (ELISA). Total encapsulation was approximated as the amount of LIF released over a seven day period and percent encapsulation efficiency calculated as total encapsulation divided by maximum theoretical encapsulation. | |
| Prior to cell attachment, biotinylated rabbit anti-GFR-α1 antibody (Acris) was incubated with the avidin-coated nano-particles as previously described by Park et al. [13]. Free unbound antibody was removed after centrifuging out the nanoparticles which were then washed once immediately prior to use on cells. To control for potential non-specific effects, empty nanoparticles lacking LIF cargo were used, whilst the effect of targeting antibody was controlled for by use of non-targeted nanoparticles (empty, or with LIF-cargo). | |
| Cell culture | |
| Ventral mesencephalon (VM) differentation medium consisted of DMEM plus 10% fetal calf serum, 2% B-27 supplement; 100 U/ ml penicillin, 100 μg/ml streptomycin and 250 ng/ml amphotericin B. Serum-free proliferation medium for expansion of VM as neurospheres consisted of Neurobasal A, 2% B-27 supplement; 100 U/ml penicillin, 100 μg/ml streptomycin, 250 ng/ml amphotericin B, 2nM L-glutamine, 20ng/ml epidermal growth factor, and 20 ng/ml fibroblast growth factor-2. VM cultures from time mated Sprague- Dawley rats at embryonic gestation day 14 (E14d) were made following the protocol described by Pruszak et al. [14]. | |
| After a single cell suspension was prepared, the fetal VM-derived cells were collected as a crude concentrated cell suspension to which the nanoparticles were added and gently mixed. After at least 30m at room temperature - to allow cell attachment of the nanoparticles - the cells were washed free of unbound nanoparticles prior to plating on laminin-coated coverslips as 50 μl droplets containing 50,000 cells. After 30m for cell adherence, 500 μl differentiation medium was added per well and cultures incubated at 37°C in 5% CO2 in air. Fifty percent of the growth medium was exchanged every 2d using nanoparticle-free differentiation medium replacement. | |
| Cultures were fixed for analyses of (i) total β III-tubulin+ neuronal cells (mouse anti- β III-tubulin Sigma-Aldrich 1/500); (ii) tyrosine hydroxylase (TH)+ DA cells (rat anti-TH: AbCam 1/300); (iii) serotoninergic cells (rabbit anti-SERT: AbCam 1/500); and (iv) glia (rabbit anti-GFAP: Dako 1/500): details for individual experiments are provided in the figure legends. Apoptosis was assessed using caspase-3 release using standard techniques (Cell Signalling Tech). | |
| To measure the time course of any therapeutic effects, replicate cultures were analysed after fixed times in vitro as detailed in the figure legends. All measurements were in triplicate. Statistical analyses are provided in the figure legends. | |
Results |
|
| Figure 1 outlines the rational of this study, where the aim is to improve cell therapy for PD by supporting dopaminergic cell survival by cell attachment of PLGA nanoparticles containing LIF. | |
| Figure 1: Overview of current cell-based therapy for PD. A: For cell-based therapy, a current clinical source of dopaminergic cells for transplantation is from donated primary human fetal tissue, subject to full consent under full ethical approval. During cell harvest and preparation a major proportion of the cells die and multiple donors are required to treat one patient. It is proposed that by attaching nano-LIF (see insert) to the harvested human fetal cells ex vivo - providing a surrogate biodegradable stroma that releases LIF -will significantly reduce cell death and thereby reduce numbers of fetal donors required for therapy. Image sources: Parkinson’s Disease, and cross-section of human brain: Wikipedia; human fetus: http://embryology.med.unsw.edu.au.B: Nano-LIF image with permission from Cell Cycle and C: Left panel shows cargo release data as previously published [13]; right panel cartoon of denuded cell versus cell coated with PLGA nanoparticles to create a surrogate extracellular stroma. | |
| Primary dopaminergic neurons express the LIF receptor | |
| To exploit LIF-nano for cell therapy in PD, we first needed to show that the dopaminergic cells can respond to LIF through their expression of the LIF-receptor (LIF-R). LIF-R is a heterodimer of gp130 (CD130) and gp190 (CD118) and functionally discrete from homodimers of gp130 that mediate IL-6 signalling [15-18] and downstream inflammatory events. Importantly LIF does not recapitulate IL-6 effects in lymphocytes and is anti-inflammatory [19], emphasising a critical role of gp190 in LIF-mediated homeostasis. Staining of primary rat E14 ventral mesencephalon (VM) cultures demonstrated that dopaminergic neurons, identified via tyrosine hydroxylase (TH) staining, co-expressed both gp130 and gp190. Thus LIF is a suitable therapeutic cargo for DA cell-based therapy for PD. | |
| DA cell responsiveness to LIF was confirmed in a dose response experiment where rat fetal E14 VM cells were plated in the presence of 0.1 ng/ml; 1 ng/ml; 10 ng/ml; or 100 ng/ml soluble recombinant mouse LIF: parallel control cultures were identical but lacked LIF addition. Readout was taken upto 5 days in vitro (DIV). Immunocytochemistry demonstrated that 0.1 ng/ml LIF significantly increased the number of tyrosine hydroxylase positive neurons at both 3 and 5 days (Figure 2). | |
| Figure 2: Soluble LIF increases numbers of dopaminergic cells in vitro After first confirming DA cell express both gp130 and gp190 by immunocytochemistry, responsiveness to soluble LIF was tested. Primary E14 VM tissue in monolayer differentiation culture treated with LIF doses from 0.1 to 100 ng/ml. A. TH+ cell numbers at 2 DIV showed no significant effect. At both 3 DIV and 5 DIV (B and C) 0.1ng/ml LIF significantly increased the dopaminergic cell count (one way ANOVAs, F4,14 = 4.55, p< 0.05 and F4,14 = 4.65, p< 0.05 respectively; Post hoc Tukey tests, * p< 0.05). | |
| Primary dopaminergic neurons express GFR-α1 | |
| Having established that dopaminergic precursor cells respond to LIF, we next sought a suitable DA cell surface antigen to which to target the LIF-nano device. Since glial-derived neurotrophic factor (GDNF) is neurotrophic for dopaminergic neurons [19], we looked for expression of the GDNF family receptor α-1 (GFRα-1) in primary rat E14 VM cultures. Co-expression of TH and GFRα-1 was confirmed. Accordingly the LIF-nano device was adapted to target GFRα-1 by surface attachment of biotinylated anti-GFRα-1 to the NP’s avidin-coated surface and shown to be efficacious (Figure 3A). | |
| Figure 3: GFR-α1 expressed on the surface of DA cells is suitable for NP
targeting A suitable target for nano-LIF was required for NP delivery. Figure 3A: left panel of four images shows E14 VM monolayer cultures that were fixed after 3 days in vitro and stained for dual expression of GFR-α1 and tyrosine hydroxylase (TH). The arrow indicates a TH+ cell expressing GFR-α1: other cells were also GFR-α1 positive but not of the DA type. The scale bar represents 25 μm. The right panel shows that nano-LIF targeted to GFR-α1 results in increased TH+ cell numbers at 5 DIV: in parallel, nano-empty targeted to GFR-α1 had no effect. (One way ANOVA, F2,11 = 6.23, p< 0.05. Post-hoc Tukey test, * p< 0.05). Figure 3B: To confirm requirement for both LIF and targeting, monolayer cultures treated with nano-empty of nano-LIF, each with or without targeting, were counted after 5 DIV: only the nano-LIF targeted induced a significant increase in DA numbers. |
|
| The next step was to compare efficacy of soluble LIF with LIFnano targeted to GFRα-1. Rat fetal VM cells were plated in monolayer cultures and treated (per million cells for NP) with (i) GM alone; (ii) 0.1ng/ml non-targeted empty NP; (iii) 0.1mg targeted empty NP; (iv) 0.1 mg non-targeted LIF-nano NP; and (v) 0.1mg targeted LIF-nano NP. After 3 days, targeted LIF-nano had caused a significant 2-fold increase in DA neurons, whilst no effect was seen in any of the other groups (Figure 3B). Thus the results confirmed that LIF was required for the dopaminergic effect, rather than simple cross-linking of the GFRα-1 during targeting of the NP; and that targeting of the LIFnano was required for efficacy. | |
| Nano-LIF therapy is anti-apoptotic for DA cells | |
| DA cells are fragile and readily succumb to stress during handling, with upto 90% cell loss during preparation of hfVM cells for clinical transplantation. The increased yield of DA cells treated with nano-LIF could have been due to either a pro-survival effect, or increased differentiation of the DA precursors in the rat fetal VM cell population - both of potential importance for improving yield of cells for grafting. When apoptosis was measured by caspase 3 staining, both soluble LIF and LIF-nano treatment significantly reduced the proportion of dopaminergic neurons undergoing apoptosis (Figure 4), demonstrating a significant pro-survival effect of LIF that was maintained with use of the NP formulation | |
| Figure 4: Both soluble and nano-LIF reduce apoptosis of DA cells Primary E14 VM cultures treated were (i) untreated, or treated with (ii) 0.1 ng/ml soluble LIF; (iii) 0.1mg/ml LIF-nano; or (iv) 0.1 mg/ml empty-nano. Cleaved caspase-3 staining of TH+ neurons was used to detect apoptotic DA cells. After 2 DIV both soluble and LIF-nano reduced the proportion of apoptotic dopaminergic neurons (One way ANOVA, F3,11 = 14.13, p< 0.01, Post-hoc Tukey tests, * p< 0.05). | |
| Nano-LIF treatment shows selectivity for DA cells | |
| Next we looked for potential off-target effects of nano-LIF, given the complexity of cell populations derived from fetal ventral midbrain. This is of special relevance since there is potential risk of graftinduced dyskinesia (GID) [7]. Dyskinesias are abnormal involuntary movements that may be primed by previous exposure to L-DOPA: indeed long-term L-DOPA therapy is limited since L-DOPA itself eventually induces dyskinesia (LID). The pathogenesis of GIDs is unknown but one theory [20] is that co-grafted serotonergic (5- HT) neurons in the transplant engage in storage of dopamine and its release in a non-physiological manner, termed “false transmitter release”. A graft-derived excess of serotoninergic neurons interacting with the normal dopaminergic neurons may dysregulate dopamine release at the synapse leading to dyskinesia. Thus it is critical that future VM grafts contain the right ratio of DA to 5HT neurons and we therefore explored the possibility that LIF-nano therapy might also induce excessive numbers of serotoninergic cells in grafted fetal ventral midbrain. | |
| We first asked, do serotonergic cells express GFRα1? Co-staining for either serotonin or the serotonin transporter, SERT, plus GFRα1 confirmed dual positivity (Figure 5A) and thus - in addition to DA cells - serotoninergic cells represent targets of the anti-GFRα1- directed NP. Next, E14 rat VM cultures were treated with LIF (0.1ng/ ml); LIF-nano (0.1mg/million cells); or empty nanoparticles (0.1 mg/million cells) and fixed at two, three, or five days post-plating. Following immunocytochemistry, quantification of dopaminergic and serotonergic neurons demonstrated that neither soluble nor nanoparticle encapsulated LIF altered the dopaminergic to serotonergic ratio (Figure 5B). | |
| Figure 5: Nano-LIF does not disproportionately expand the serotonergic cell population A: co-staining for serotonin and GFR-α1 revealed dual positivity: thus serotoninergic cells will be targeted by LIF-nano-anti-GFR-α1 NP. B: Treatment with soluble LIF (0.1 ng/ml), LIF-nano (0.1 mg/ml), or nanoempty NP (0.1 mg/ml), did not alter the ratio of DA to serotonergic cells in monolayer cultures after 2, 3, nor 5 DIV. | |
| Nano-LIF acts on differentiated DA cells | |
| We were also interested in the source of the increase in the DA cell numbers following LIF treatment as this could be due to (i) increased dopaminergic differentiation due to prior precursor expansion, or (ii) increased survival of differentiated dopaminergic neurons, or (iii) a combination of the two. Here, in the first part of the experiment, we used primary E14 VM tissue expanded as neurospheres (ie precursor cells) in proliferation medium in the presence, or absence, of 0.1 ng/ml soluble LIF. There was no effect of LIF on subsequent neural or glial differentiation (data not shown), suggesting that the effect on differentiated cells in monolayer culture was on matured dopaminergic cell survival. | |
| Secondly we asked, is the effect of nano-LIF that results in increased DA cell numbers a direct effect of LIF, or an indirect one, mediated by astrocytes that are known to release neurotrophic factors that are able to support primary VM cultures. Figure 6 shows that primary E14 VM tissue grown as monolayer cultures in the presence of either soluble LIF (0.1 ng/ml); LIF nanoparticles (0.1 mg/million cells); or empty nanoparticles (0.1 mg/million cells) contained similar numbers of astrocytes. Moreover, BrdU incorporation into the GFAP positive astrocytes showed equivalent proliferation in each of the treatment groups. Given that neither soluble LIF not LIFnano induced expansion of the glial astrocytic population in the VM cultures, the data shows that the effect of LIF-nano in increasing DA cell numbers is direct for the DA cells. Therefore, LIF-nano therapy - being independent of astrocytes - would be applicable for isolated populations of DA cells if these were to be used as the source for grafting. | |
| Figure 6: LIF does not affect astrocyte proliferation or the absolute number
of astrocytes Since astrocytes express the LIF receptor in addition to being capable of cell division (unlike mature DA cells) we asked if astrocytes are induced to proliferate by LIF. Monolayer cultures were given a pulse of 15 μM BrdU at 4 DIV and fixed following BrdU washout 24 hours later. Top panel “A” shows that numbers of astrocytes remained unchanged compared to PBS controls, when cultured with LIF or NP as detailed. Lower panel “B” similarly shows no effect on astrocyte proliferation. |
|
Discussion |
|
| Here we address a major issue in regenerative cell-based therapy - that is, how to deliver therapeutic cells denuded of growth factors and stromal support, whilst maintaining their functional therapeutic viability. Use of soluble growth factors fails due in part because they are rapidly degraded in vivo, and in part because in some circumstances growth factors require delivery via an extra-cellular stroma. We had reasoned that a surrogate stroma composed of LIFnano might succeed by the paracrine-type delivery of growth factors directly targeted to DA cells. Thus the potential value of LIF-loaded PLGA nanoparticles in a rat model of cell-based therapy in PD was investigated. We found that this approach produced significant benefit for DA cell survival in vitro, and that this was best seen using NP-mediated delivery of LIF where specific targeting to the relevant neuronal population had relatively specific effects. Given that LIF not only supports endogenous reparative activity, but also is tolerogenic, the value of nano-formulated LIF is compounded in potential to support engrafted cells in the immune competent host. | |
| The study design also has value as a guide on how to assess a candidate nanotherapeutic. A series of rational steps were taken: firstly to demonstrate that that primary rat fetal DA precursor cells are sensitive to exogenous LIF therapy; secondly that these DA cells express a suitable cell surface antigen for targeting; thirdly that nano- LIF therapy exerts prosurvival effects on these cells - a property especially valuable given the fragility of DA cells. Finally we showed minimal off-target effects, implying that the use of nano-LIF promotes DA cell-based therapies whilst reducing the risk of serotoninergic neuronal-induced GIDS.These outcomes, by demonstrating efficacy and apparent safety of nano-LIF, have since led to further work to be reported elsewhere the TransEuro Clinical Trial (http://www.transeuro.org.uk) is using primary human fetal VM transplants into PD patients: in parallel, use of the nano-LIF to promote survival of hfVM under clinical conditions is being tested. | |
Summary |
|
| The current work details the series of rational steps taken to underpin subsequent clinical translation of the LIF-nano therapeutic for use in cell-based therapy for PD. By exploiting the readily available rat fetal VM model to assess nano-LIF, detailed analytical data directly relevant to clinical use was generated. | |
| The effect of PLGA-LIF to support survival of human fetal VM cells is now being tested alongside the clinical trial - see www. transeuro.org.uk - where preclinical evaluation includes use of LIFnano- treated human fetal VM xeno-grafts into the striatum of nude rats. | |
Acknowledgements |
|
| SD was in receipt of an MRC Research studentship; TMF was funded by i4i NIHR Project Grant II-AR-1109-11037 awarded to RAB and SMM. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi