Research Article, Med Microbiol Rep Vol: 1 Issue: 1
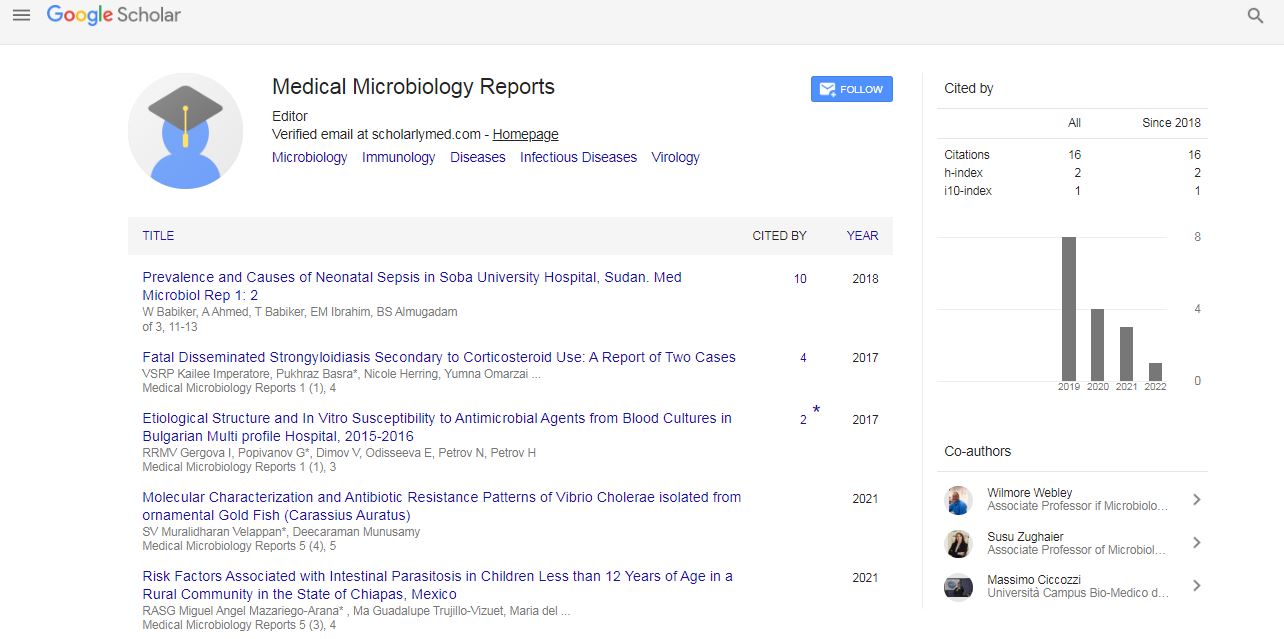
Etiological Structure and In Vitro Susceptibility to Antimicrobial Agents from Blood Cultures in Bulgarian Multi profile Hospital, 2015-2016
Gergova I1, Popivanov G2*, Dimov V3, Odisseeva E3, Petrov N3, Petrov H2, Ribarov R4 and Mutafchiyski V2
1Department of Military Epidemiology and Hygiene, Military Medical Academy, Sofia
2Clinic of Endoscopic, Endocrine surgery and Coloproctology, Military Medical Academy, Sofia
3Department of Anaesthesiology and Critical Care, Military Medical Academy, Sofia
4Faculty of Public Health, Medical University, Sofia
*Corresponding Author : Popivanov G
Department of Clinic of Endoscopic, Endocrine surgery and Coloproctology, Military Medical Academy, Sofia, Bulgaria
Tel: +359 885 521 241
E-mail: gerasimpopivanov@rocketmail.com
Received: July 27, 2017 Accepted: August 09, 2017 Published: August 16, 2017
Citation: Gergova1 I, Popivanov G, Dimov V, Odisseeva E, Petrov N, et al. (2017) Etiological Structure and In Vitro Susceptibility to Antimicrobial Agents from Blood Cultures in Bulgarian Multiprofile Hospital, 2015-2016. Med Microbiol Rep 1:1.
Abstract
During the period 2015-2016, a total of 1490 haemocultures were tested, 24.4% of which were positive. Among the 363 isolated microbial agents, 224 (62% or 15% of all) were considered clinically significant with equal distribution of Gram-positive (48.2%) and Gram-negative bacteria (47.8%). This finding differs from European
and US practice where Gram positive bacteria are dominant. Fungi were isolated in 4%. The etiological structure was as follows:Coagulase Negative Staphylococcus – 20.1%, E. coli - 14.3%, Enterococcus spp. - 14.3%, Klebsiella spp. - 11.2%, S. aureus - 10.3%, Acinetobacter baumannii - 9.4%, Enterobacter spp. - 5.8%, P. aeruginosa – 4.9%. A trend toward increase of Klebsiella spp, E.coli, S. aureus и Candida spp. and decrease of coagulase-negative Staphylococci, Enterococcus spp. and Acinetobacter baumannii was observed. Regarding “ESKAPE” pathogens – we had a similar rate of Enterococci, and lower rates for the rest compared to USA practice, but in contrast to European data we had lower rate of S. aureus, similar rates of Enterobacter and P. aeruginosa, and higher rates of Enterococci, Klebsiella and Acinetobacter. Multidrug resistance was found in 11% of Gram positive and 47% of Gram negative flora. Resistance rates were similar to the European, but higher in Gram negative and lower in Gram positive when compared to USA. Owing to failure of the other approaches we introduced a stronger stewardship and restrictive policy regarding prescription of antibiotics.
Keywords: Blood stream infections; Haemocultures; ESKAPE pathogens; Multi drug resistance
Introduction
Despite the recent advance in medicine bloodstream infections (BSI) leading to severe sepsis and septic shock represent a major source of morbidity and are still associated with a high mortality exceeding 50% [1]. According to population-based studies, which are claimed to be the best of defining epidemiology in non-selected population, the rate of BSI is 140-160 per 100 000 in high-income countries [2]. The estimated rates for North America and Europe are up to 67,7 000 and 1.4 million episodes per year with case-related mortality 12-18% (94,000 deaths) and 13-20% (27,6 000 deaths) respectively [3]. The annual cost in USA is estimated at 24 $ billion [1].
Moreover, we are witnesses of a dramatic increase of multidrug resistant organisms (MDR), especially in a hospital setting [4]. Particularly, it is valid for the so-called „ESKAPE“ pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacteriaceae), which increasingly become a major health care problem worldwide. The infections caused by MDR are associated with up to 30,000$ increase of the additional hospital costs per case [5]. Commonly, MDR strains differ between the different health care providers and geographical areas, so evaluation of their etiologic structure and type of resistance for any particular instituttion and geographical area is of a paramount importance for the successful management. BSI often require starting of empiric antimicrobial therapy before the final microbiological analysis along with removal of the primary source and supportive care. According to the US Center for Disease Control (CDC), the rate of inadequately prescribed antimicrobial agenst is approximatelly 50% [1]. Delayed and/or inadequate antimicrobial therapy is associated with poorer outcome and an increased rate of MDR. In this light, the analysis of the etiological structure and type of resistance are of a paramount importance to guide the initial empiric therapy. The aim of the present study was to determine the etiological structure and type of resistance to antimicrobial agents of the pathogens isolated form blood cultures in order to actualize the guideline for empiric therapy and to compare our data with the current trends worldwide.
Material and Methods
The study was conducted in a Multiprofile hospital for active treatment with 840 beds, average 36,000 admissions annually and serving as a tertiary center for the whole country. Since 2015 a strict antimicrobial stewardship and restrictive antibiotic policy were implemented into our practice. A total 1490 blood cultures during 2015-2016 were tested. All repeated isolates from any given patient were excluded from the analysis.
All specimens were taken only in the presence of clinical indications through aseptic technique according to the good clinical practice rules. The volume of blood taken (18-20 ml) was distributed equally in two sets for aerobic and anaerobic cultivation. The cultivation was performed through BACTEC 9050 (Becton Dickinson) and BacT/ALERT 3D® (Select Link) according to the instructions of manifacturer. The positive cultures were stained by Gram and were subcultivated by conventional methods [6]. The identification of the isolated pathogens was performed conventionaly [6] and/or by VITEK® 2 (bioMerieux) [7,8]. The antimcrobial susceptibility was examined through the method of Bauer-Kirby or by VITEK® 2 (bioMerieux). Examining of phenotypes of resistance was performed according to recommendations of the European Committee on Antimicrobial Susceptibility Testing (EUCAST). In Enterobacteriaceae spp. extended spectrum β-lactamase (ESBL) screening was performed by double-disk test [9]. Criteria for MDR were resistance to more than three groups of antibiotics for both Gram positive and negative flora or methicyllin resistance of Staphylococci (MRSA). All results were analyzed according to the criteria of EUCAST [7,8].
Results and Discussion
Etiological structure
The results are given on Table 1. Overall 24.4% (363/1490) of a total 1490 haemocultures were positive. However, only 62% of them (n=224) or 15% of all were assessed as clinically significant. Thirty eight percent (139/363), mainly coagulase-negative Staphyloccoci (CNS), were considered a contamination of skin flora which is similar to others reported CNS as the main contaminant (75%) [5,10]. The positive culture rate is similar to the ICU survey conducted in innercity hospital in New York (12.6%) [5] European rate (15.5%) [11] and others (17-20%) [12,13], but significantly higher than reported for the rest country (7.5-11%) [14-16]. There was almost equal rate of Gram positive and Gram negative flora – 48.2% vs. 47.8%. This finding differs sifnificantly from other large bulgarian hospitals data indicating preponderance of Gram positive flora (62-72%) [14-16], from a recent US survey and a large study, encompassing 112 European hospitals, reporting rates 59% vs. 31% [5] and 53% vs. 41% [11], respectively. However, a large US survey of National Healthcare Safety Network (NHSN), evaluating only central line-associated BSI (CLABSI), reported significantly higher rate of Gram positive versus Gram negative bacteria (51% vs. 26%) [17].
| Isolates | 20151 (n=106) |
20161 (n=118) |
Total1 (n=224) |
|---|---|---|---|
| Bacteria | |||
| Gram negative | |||
| Escherichia coli | 12.3 (13) | 16.1 (19) | 14.3 (32) |
| Klebsiella spp. | 5.7 (6) | 16.1 (19) | 11.2 (25) |
| Enterobacter spp. | 6.6 (7) | 5.1 (6) | 5.8 (13) |
| other Enterobacteriaceae | 0 | 0.8 (1) | 0.4 (1) |
| Acinetobacter baumannii | 12.2 (13) | 6.8 (8) | 9.4 (21) |
| Pseudomonas aeruginosa | 6.6 (7) | 3.4 (4) | 4.9 (11) |
| other non-fermentative | 0.9 (1) | 2.5 (3) | 1.8 (4) |
| Total | 44.3 (47) | 50.8 (60) | 47.8 (107) |
| Gram positive | |||
| Coagulase negative Staphylococcus (CNS) | 26.4 (28) | 14.4 (17) | 20.1 (45) |
| Staphylococcus aureus | 8.5 (9) | 11.9 (14) | 10.3 (23) |
| Enterococcus spp. | 17.0 (18) | 11.9 (14) | 14.3 (32) |
| Other Gram positive | 0.9 (1) | 5.9 (7) | 3.6 (8) |
| Total | 52.8 (56) | 44.1 (52) | 48.2 (108) |
| Fungi | |||
| Candida spp. | 2.8 (3) | 5.1 (6) | 4.0 (9) |
Table 1: Etiological Structure of Bloodstream Infections in MMA, 2015-2016.
In the present series, CNS was the leading Gram positive pathogen (20%), followed by Enterococcus spp. (14%) and S. aureus (10%). The proportion of CNS leading to clinically manifested infection was significantly lower when compared to the average for our country 34-50% [14-16], but is comparable with the reported rates for the European Union and US [10,17]. The rate of S. aureus was lower than the other Bulgarian studies (15%) [14,15], Europe [11] and USA [5]. Despite the drop of Enterococcus spp. (from 17% to 12%) it still represents a major challenge due to frequent MDR. Our rate is similar to USA (17-18%) [5,17], but higher than Europe (4.6%) [11].
Most of the Gram negative isolates in our series were Enterobacteriaceae spp. (31% of all isolated strains), which is confirmed by some institutions [14], although other reported preponderance of non-fermentive Gram negative flora at national level [15].
A major concern for our Institution are Acinetobacter baumannii, Klebsiella spp. and P. Aeruginosa, although the rate is similar to other reports [14,18,19]. There was significant increase of Klebsiella spp., while A. baumannii and P. aeruginosa dropped significantly. European study reported lower rates of these pathogens [11], whereas the single center US report showed significantly higher rate of Klebsiella and A. baumannii [5]. NHSN reported lower rates of Klebsiella (8%), A. baumannii (2%) and P. aeruginosa (4%), but significantly higher Candida spp. (14.6%) in CLABSI [17]. The rate of fungi was 4% in the present series, with increase from 2.8% to 5.1%, versus 5% and 10% in European and US series [5,11].
Resistance to antimicrobial agents
MDR appears to be the major problem of the contemporary health care system leading to increased morbidity, mortality and hospital costs. This was the reason Infectious Diseases Society of America (IDSAS) to initiate the 10×′20 initiative for development of ten new antibiotics by 2020 [20]. The resistance rate for β-lactams of S. aureus (MRSÐ) was 11% and was significantly lower in comparison to the average for all hospital isolates (40%), and similar to other Bulgarian authors – 7-31% [14,15]. Our rate is similar to other European reports, but is significantly lower than reported rates in Canada (22%) and USA (53-55%) [5,17]. Enterococcus spp. was characterized with a high level of gentamycin resistance (HLR-gentamicin) (89% of all), which is significantly higher than the average for our country [14,15], but is comparable with other centers (74%) [21]. There were no S. aureus и Enterococcus spp. resistant to glycopeptides (VRE) and Linezolid in contrast to Orsini et al. who reported VRE in 67% of the Enterococci [5] and 83% rate reported by Sievert et al. [17]. Enterococcus spp became particularly problematic, especially as a cause of nosocomial infections. VRE appeared in USA and Europe during the late 1980-ies. It was the first bacteria developed acquired Vancomycin resistance and could be a great threat due to its ability to transfer resistance genes to other Gram positive and negative species [22,23]. Actually, the rate of MDR among Gram positive flora was 11% compared to 19% in others [5].
Among Enterobacteriaceae, ESBL-producers were widespread, frequently with resistance to other antimicrobial groups. ESBL and MDR were 31% of E. coli and 36% of K. pneumoniaе, which is similar to the literature data [5,14-16,18]. In fact, 46.7% of Gram negative flora in our series were MDR. Orsini et al. showed MDR in 34% of Gram negative organisms with ESBL in 92% [5]. All A. Baumannii and P. aeruginosa strains in our series were MDR, including carbapenems, aminoglycosides, quinolones and Piperacilin/Tasobactam, but susceptible to colistin. There were no carbapenem-resistant Klebsiella strains. The multicenter US survey reported Carbapenem resistance in 63%, 26% and 13% for these pathogens without significant difference between ICU and non-ICU [17]. However, the single center study including all hemocultures, showed Carbapenem resistance in 75% of the Gram negative organisms, all of them A. baumannii and K. pneumoniae [5]. In an US survey spanning 2006-2008, Kallen et al. reported MDR rates for A. Baumannii P. aeruginosa and K. pneumoniae – 60%, 10% and 15%, respectively [5].
Conclusion
The empiric therapy of severe infections should be based on upto- date reports of the etiological structure at institutional and national level. A trend toward increase of Klebsiella spp., E. coli, S. aureus и Candida spp. and decrease of coagulase-negative Staphylococci, Enterococcus spp. and Acinetobacter baumanni was observed for our Institution. Regarding “ESKAPE” pathogens – we had similar rate of Enterococci, and lower rates for the rest compared to USA practice, but in contrast to the European data we had lower rate of S. aureus, similar rates of Enterobacter, P. aeruginosa and higher rates of Enterococci, Klebsiella and Acinetobacter.
MDR was observed in 11% of Gram positive and 47% of Gram negative organisms. MDR rates were similar to the European, but higher in Gram negative and lower in Gram positive when compared to USA. We consider that is the incorrect use of the antimicrobial drugs. Owing to failure of the other approaches we introduced a stronger stewardship and restrictive policy regarding antimicrobiological prescription.
References
- Scerbo M, Kaplan H, Dua A, Litwin D, Ambrose C, et al. (2016) Beyond blood culture and Gram stain analysis: A review of molecular techniques for the early detection of bacteriemia in surgical patients. Surg Infections 17: 294-302
- Laupland K (2013) Incidence of bloodstream infections: a review of population-based studies. Clin Microbiol Infect 19: 492-500
- Goto M, Al-Hasan M (2013) Overll burden of bloodstream infection and bloodstream infection in North America and Europe. Clin Microbiol Infect 19: 501-509.
- Basseti M, Righi E (2015) Development of novel antimicrobial drugs to combat multiple resistant orgaisms. Langenbecks Arch Surg 400: 153-165
- Orsini J, Mainardi C, Muxylo E, Karki N, Cohen N, et al (2012) Microbiological profile of organisms causing bloodstream infection in critically ill patients. 4: 371-377
- Forbes B, Sahm D, Weissfeld A (2007) Bailey & Scott's Diagnostic Microbiology
- European Committee on Antimicrobial Susceptibility Testing (2015) European Society of Clinical Microbiology and Infectious Diseases. V5.0.
- European Committee on Antimicrobial Susceptibility Testing (EUCAST) (2016) European Society of Clinical Microbiology and Infectious Diseases. V6.1.
- Jarlier V, Nicolas M, Fournier G, Philippon A (1988) Extended broad-spectrum β-lactamases conferring transferable resistance to newer β-lactam agents in Enterobacteriaceae: hospital prevalence and susceptibility patterns. Rev Infect Dis 10: 867-878.
- Mirrett S, Weinstein M, Reimer L, Wilson M, Reller L (2001) Relevance of the number of positive bottles in determining clinical significance of Coagulase-negative staphylococci in blood cultures. J Clin Microbiol 39: 3297-3281.
- Bouza E, Peres Molina J, Minoz P (1999) Cooperative Group of the European Study Group on Nosocomial Infections Report of RSGNI-001 and ESGNI-002 Studies. Bloodstream infections in Europe. Clin Microbiol Infec 5: 1-12.
- Budak A, Filip E, Wodzinski P (2002) Microbiologic analysis of results from blood cultures. Med Dosw Microbiol 54: 75-86.
- Masaki H, Ide M, Yoshimine H, Matsumoto K (1994) Clinical significance of positive blood cultures in the Nagasaki Rosai Hospital durimg the past 6 years. Kansenshogaku Zasshi 68: 617-624
- Bojkova K, Stoeva T, Kaludova V, Kamenova V, Rusev V (2005) The clinical isolates of blood cultures and their in vitro susceptibility to antimicrobial agents. Infectology 4: 21-23.
- Rukanova D, Rachkova K, Djeneva H, Boicheva M, Teneva M, et al. (2014) Species affiliation and antibiotic resistance of the clinical isolates of haemocultures. Trakia J of Sci 3: 227-232.
- Rukanova D, Staikova E, Rachkova K, Dukova I, Djeneva H, et al. (2008) Species affiliation and antibiotic resistance of the clinical isolates from haemocultures. Trakia J of Sci 6(2): 138-141.
- Sievert D, Ricks P, Edwards J, Schneider A, Patel J, et al. (2013) Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Center for Disease Control and Prevention, 2009-2010. Infect Control Hosp Epidemiol 34: 1-14.
- Bauer A, Kirby W, Sherris J, Turck M (1963) Antibiotic susceptibility testing by a standardized single disc method. Am J Clin Pathol 45: 493-496.
- Ibrachim E, Sherman G, Ward S, Fraser V, Kollef M (2000) The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest 118: 146-155.
- Infectious Diseases Society of America (2010) The 10 × '20 initiative: pursuing a global commitment to develop 10 new antibacterial drugs by 2020. Clin Infect Dis 50: 1081-1083.
- Li W, Li L, Wei Q, Hu Q, Lin X, et al. (2015) Characterization of aminoglycoside resistance and virulence genes among Enterococcus spp. isolated from a hospital in China. Int J Envirom Res Public Health 12: 3014-3025.
- Murray B. Diversity among multidrug-resistant Enterococci (1998) Emerg Inf Dis 4: 37-47.
- Moellering R. Vancomycin-resistant enterococci (1998) Clin Infect Dis 26: 1196-1199
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi