Research Article, J Trauma Stress Disor Treat Vol: 10 Issue: 7
Ethnic and Sex Comparison of PTSD Comorbidities in Israel: Anxiety and Depression Rates among Muslims, Druze, and Christians
Chen Hanna Ryder1*,2, Hiba Zaidan3, Darian Ryder4, Carmit Gal5, Karin Beiruti2, Kamal Farhat6, Alexander Mizrukhin7, Radi Shahien2,8
1Department of Criminology, Western Galilee College, Acre, Israel
2Department of Neurology, Faculty of Medicine in the Galilee, Brain Research Laboratory, Ziv Medical Center, Affiliated to Bar-Ilan University’s Safed, Israel
3School of Psychological Sciences and the Integrated Brain and Behavior Research Center, University of Haifa, Haifa, Israel
4Faculty of Education in Science and Technology, The Virtual Reality and Neuro-Cognition Laboratory, Technion Israel Institute of Technology, Haifa, Israel
5Department of Education, Western Galilee College, Acre, Israel
6Department of Psychiatry, Nazareth Hospital EMMS, Nazareth, Israel
7Department of Psychiatry, Ziv Medical Center, Safed, Israel
8Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel
- *Corresponding Author:
- Radi Shahien
Department of Neurology
Faculty of Medicine, Ziv Medical Center
Affiliated to the Azrieli Bar-Ilan University
POB 1008 Safed, 13100, Israel
Fax: (+972)-4-6828648
Tel: (+972)50-8434197
E-mail: radis@ziv.gov.il
Received: May 18, 2021 Accepted: July 16, 2021 Published: July 23, 2021
Citation: Ryder CH, Zaidan H, Ryder D, Gal C, Beiruti K, et al. (2021) Ethnic and Sex Comparison of PTSD Comorbidities in Israel: Anxiety and Depression Rates among Muslims, Druze, and Christians. J Trauma Stress Disor Treat 10:7.
Abstract
Abstract Objective: The Arab population in Israel is comprised of diverse ethnic groups, primarily Muslims, Druze, and Christians, each with unique characteristics. However, previous research involving Posttraumatic-Stress-Disorder (PTSD) and its associated comorbidities regarded the Arab population homogeneously. This study explored the ethnic and sex differences in comorbidity rates among post-war Posttraumatic Israeli Muslims, Druze and Christians. Material and Method: 62 participants; 20 men & 42 women (12 Druze, 40 Muslims & 10 Christians), aged 18-69, were assessed by a Structured Clinical Psychiatric Interview and self-report questionnaires. Results: Women dominated (66.7%) chronic PTSD. Overall comorbidity rates of Generalized Anxiety Disorder (GAD) and Major Depressive Disorder (MDD) were very high (96%). Comorbidities rates comparison between different ethnicities found that Muslim population exhibited the highest comorbidity rates across all comorbidity types. Specifically, Muslim women displayed higher GAD rates than Druze women, while Druze women displayed higher MDD rates than their Muslim and Christian counterparts. Additionally, Muslim women had higher MDD rates than Christian women. Conclusion: Different ethnic groups suffering from PTSD, exhibit distinctive comorbidity distributions of GAD and MDD. We suggest that further studies should take into consideration the groups’ distinctive cultural characteristics and avoid regarding the Arab population homogeneously. Thus, tailored personalized mental health interventions are needed to meet the distinct and unique requirements of each ethnic group in sex-depended manner. Keywords Posttraumatic Stress Disorder (PTSD); Ethnicities; Comorbidity; Major Depression Disorder (MDD); Generalized Anxiety Disorder (GAD); Arabs; Sex differences.
Keywords: Posttraumatic Stress Disorder (PTSD); Ethnicities; Comorbidity; Major Depression Disorder (MDD); Generalized Anxiety Disorder (GAD); Arabs; Sex differences
Keywords
Posttraumatic Stress Disorder (PTSD); Ethnicities; Comorbidity; Major Depression Disorder (MDD); Generalized Anxiety Disorder (GAD); Arabs; Sex differences
Introduction
Israel possesses a unique multicultural diversity, comprised of several ethnic and religious groups. 20.9% are Israeli Arabs, 83% of them are Muslims, 9% Christians and 8% Druze [1]. These groups differ in many aspects, including religious beliefs and practices, traditions as well as lifestyle [2]. The Islam, Christian and Druze religions vary in the nature of their belief (e.g. prophets, holy days, nature of immorality, reincarnation etc.) and practices. The Arab population in Israel has faced unstable political situations, which has set challenges to their complex identity repertoire [3]. The Muslims, Christians, and Druze communities have been exposed to distinct economic and sociopolitical conditions, and their cultures have evolved along somewhat different trajectories. These cultural distinctions are not necessarily the result of merely differences in religious doctrines and precepts [4]. The Christians have different demographic patterns than the Muslims and Druze. They tend to marry at an older age, and have fewer children [5]. The average Christian has attained a higher level of formal education than of the Muslim and Druze. Christians have legitimized women’s employment earlier, and consequently Christian Arab women are much more likely to be employed than other Arab women [4]. The most noticeable feature that distinguishes the Druze in Israel from other Arab groups, is their conscription to military service [6]. The intensified social contact between Druze and Jews due to military service may have facilitated the penetration of Western culture into Druze communities. It was found that in contrast to other Arabs in Israel, religious self-identification seemed to be dominant among the Druze, followed by their Israeli and Arab identities, they consider themselves more integrated in Israeli society [7], and their political trends have been different for decades [2]. Most studies regarding the Arab population examine the different ethnic and religious groups under the simple umbrella of Arabs, as a homogeneous traditional group, assuming their ethnic similarity is sufficient to serve as a common denominator, while the diversity of racial, national, historical, and religious traditions is being ignored. All the aspects stated above indicate that Israeli Arabs are heterogeneous, multi-ethnic citizens.
To date, a limited number of studies have been conducted regarding post-war stress related disorders and comorbid anxiety, depression, or both comorbidities, among Israel’s Arab populations. To our knowledge, chronic PTSD and related comorbidities according to ethnic groups and sex have not yet been investigated among adult Arab population in Israel.
PTSD is the most characteristic psychiatric sequela of traumatic experiences [8]. Among the PTSD general population, comorbidity rates of anxiety range from 39% to 97% [9-12], with depression ranges from 21% to 94% and 11% to 67% of the PTSD participants suffer from a triple comorbidity [8,10,13]. However, for some individuals, the depressed mood associated with PTSD is more salient than the anxiety symptoms [14]. Comorbidity of PTSD and depression is associated with more severe symptoms, as well as higher levels of disability, and is five times more likely to manifest functional impairment as compared to those with PTSD alone [15,16]. They also exhibit higher depression, impulsivity, and hostility scores, and are significantly more likely to attempt suicide as compared to subjects with depression alone [16]. One of the main theories suggests that when PTSD and depression co-occur in the aftermath of trauma, they may represent a single traumatic stress construct, with shared vulnerability and similar predictor variables among chronic PTSD participants [15-17]. Epidemiological surveys in the general population demonstrated that PTSD, like other anxiety disorders, is nearly twice as prevalent among women as in men [18]. In this frame, Generalized Anxiety Disorder (GAD) is also twice as prevalent among women as compared to men [19], also in the Arab population anxiety disorders were found to be more common in women than in men. This phenomenon is supported by cultural studies reporting that “Arab men tend to underreport their experience of psychiatric symptoms and disorders, which is probably related to their perceived stigmatizing impact and exposing men’s vulnerability when they are expected to be resilient and always in control” [20]. The prevalence of Arab men who sought mental health treatment following the 2nd Lebanon War, was relatively low [20]. Moreover, the few men who did eventually apply for treatment, were usually married, and did not come on their own, but in response to their spouse’s entreaties, over a high level of functional impairment and psychological distress (Dr. Kamal Farhat, Dr. Radi Shahien, personal communication, January 11th, 2012). It is assumed that the reason for this phenomenon was mainly cultural. This observation led us to explore, in this study, the sociodemographic characteristics of post-war PTSD Arab minorities seeking psychiatric care and continued by studying their associated comorbidities rates according to ethnic and sex differences.
This study population uniquely experienced the traumatic events of the 2nd Lebanon War, which erupted on July 12th, 2006, and lasted for 34 days [21]. First, the Arab population was surprised to be affected by the long period of rocket attacks, which most thought were not to be aimed at their villages, reminiscent of the past where Arab villages were scarcely hit. Second, following this assumption, this population did not prepare in advance for such a scenario, and did not have shelters or other emergency procedures and equipment most common among the non-Arab population, resulting in a decreased mental and emotional preparedness [22].
Accordingly, this pilot study strives to provide a rare opportunity for studying the differences between Muslim, Druze, and Christian Arabs in the context of PTSD and its associated comorbidities (GAD, MDD, GAD + MDD), while considering each group’s unique sociodemographic characteristics.
We hypothesized that the study population’s comorbid disorders will be differentially characterized by ethnic group and sex, due to differences in religious norms, cultural lifestyle, and sociodemographic characteristics.
Materials and Methods
Participants
62 participants were included in the current study [Muslims (n=40), Christians (n=10), and Druze (n=12)], 20 men & 42 women. Participants ranged in age from 18 to 69, with a mean age of 38.0 (M=38.0, SD=12.9). All participants were treated at the Psychiatric Ward of the EMMS hospital in Nazareth, the only Arab-oriented psychiatric ward in Northern Israel. The initial study population included 75 chronic PTSD participants who were exposed to a high degree of war trauma. All participants electively received psychiatric care following their exposure to traumatic events during the Second Lebanon War.
After receiving a PTSD diagnosis and primary medical treatment, participants were entitled to 18 months of continued ambulatory mental health care services at the Psychiatric Ward, through the support of the Israel Ministry of Health.
Participants met the inclusion criteria of the study if they satisfied the following conditions: (1) First time application for psychiatric treatment due to PTSD first onset following exposure to traumatic war-related events during the Second Lebanon War, with no previous psychiatric hospitalizations; (2) No indication in the clinician’s report of past or present life-threatening physical injuries, including brain injury or mild traumatic brain injury, or any other past psychiatric disorders; (3) Age from 18 to 70 years; (4) Arab citizens, living in Northern Israel, and identifying as Muslim, Christian or Druze. Ten subjects were excluded from the research due to either previous psychiatric disorders or past hospitalizations in the Psychiatric Ward. One subject was excluded due to current diagnosis of schizophrenia, and an additional two were excluded due to previous diagnosis of personality disorders. As a result, 62 chronic PTSD participants participated in the study. This study was approved by the “EMMS” Local Ethics Committee, and informed consent was obtained from all individual participants.
Procedure
The study population included all participants who arrived for psychiatric treatment due to PTSD first onset, and for follow-ups at the Psychiatric Ward from the beginning of the war (July 12th, 2006) [21], up to the end of August, 2007.
Initial screening of the chronic PTSD population for the study, was conducted in the hospital during the continuous mental health care program. The subjects participated in a two-stage procedure that first included a psychiatric diagnostic interview for current PTSD/ GAD/MDD status to classify the participants into the various study groups (see Assessment of PTSD, GAD and MDD). At the second stage, each patient completed the sociodemographic questionnaire under clinician supervision (see Assessment of the sociodemographic characteristics).
Assessment of PTSD, GAD and MDD
PTSD was assessed by section P of the semi-structured Clinical Interview for the DSM-IV (SCID) [23]. Psychiatrists, specifically trained in administering the SCID, assessed the presence, and evaluated the severity of, DSM-IV defined mental disorders.
All participants were diagnosed as suffering from chronic PTSD, and met full PTSD diagnostic criteria, according to Structured Clinical Interview for DSM-IV-TR Disorders, I-Research Version (SCIDI- RV) [23], known for high (k=0.77–0.88) inter-rather reliability [24,25]. Diagnostic inclusionary and exclusionary criteria for GAD among chronic PTSD participants was assessed via the SCID-I-RV [23]. The Standard Clinical Interview for DSM Disorders (SCIDI/ P) [23] was applied to identify participants with elevated anxiety levels who met criteria for GAD. GAD diagnosis based on DSMIV criteria has fair (k=0.63) to good (k=0.75) inter-rater reliability [24,25]. Only Chronic PTSD participants who met full criteria for current GAD without MDD on the SCID classified into the PTSD + GAD group.
Diagnostic inclusionary and exclusionary criteria for MDD were determined using the DSM-IV SCID [23]. MDD diagnosis based on DSM-IV criteria has fair (k = 0.66) to good (k = 0.80) inter-rater reliability [24,25]. Only Chronic PTSD participants who met full criteria for current MDD without GAD were classified into the PTSD + MDD group. Triple comorbidity group classification (PTSD + GAD + MDD) was carried out only when chronic PTSD participants met full diagnostic criteria on SCID for both GAD and MDD, lacking any other comorbid psychiatric disorder.
Assessment of the sociodemographic characteristics:
Individual characteristics were collected via a sociodemographic self-report questionnaire devised specifically for our study’s needs. This questionnaire included eight items, including age, sex, ethnic group, marital status, number of children, years of education, employment status, and type of residence (e.g., city, mixed city, village, mixed village).
Statistical Analysis
The information collected in our study was cross tabulated across several variables and includes descriptive statistics. These variables consist of comorbidity classifications to GAD, MDD, or both, and numerous sociodemographic characterizations applied to the entire population. The comorbidity classifications were cross tabulated with the sociodemographic characterizations. In addition to purely descriptive data, χ2 goodness-of-fit analysis of frequency was performed where possible, to examine intergroup differences. Use of the χ2 analysis was limited to sets where the expected frequency values were larger than 5 (ne ≥ 5) for each of the conditions. Fisher’s exact test was used where applicable. This requisite limitation was imposed to preserve the entire study’s original population, who sought treatment and met criteria, which was relatively small, in the only exclusively Arab speaking Psychiatric Ward in Northern Israel. Therefore, it restricted our ability to add additional participants. Mean values and standard deviations were calculated where applicable, such as for the participants’ age, number of children, and years of education. Additionally, twotailed nonpaired t-tests were used to compare all interval variables between men and women.
Results
Participant’ Sociodemographic characterization
All participants who sought treatment at the EMMS hospital following the war, and met the study inclusion criteria, were included in the study. Of all participants, two-thirds were women and onethird was men. The participants’ sociodemographic characteristics are presented in Table 1.
Table 1: Patients’ sociodemographic characteristics by sex (** Sig. < .001).
| Male (n=20) | Female (n=42) | ||
|---|---|---|---|
| Employment Status | Unemployed** | 20.00% | 57.10% |
| Employed** | 80.00% | 42.90% | |
| Marital Status | Unmarried | 4.80% | 23.80% |
| Married | 95.20% | 76.20% | |
| Type of Residence | Mixed City | 28.60% | 38.10% |
| Mixed Village | 57.10% | 50.00% | |
| Muslim Village | 14.30% | 11.90% | |
| Religious Affiliation | Muslim | 60.00% | 66.70% |
| Christian | 20.00% | 14.30% | |
| Druze | 20.00% | 19.00% | |
| Degree of Religiosity | Secular | 45.00% | 26.20% |
| Traditional** | 35.00% | 59.50% | |
| Religious | 20.00% | 14.30% |
The average age of the participants was 38.0±12.9 years, with the men (42±11) being significantly older than the women (36±14) (t=1.975, α<0.05). As for employment status, men were significantly more employed (80%) than women (42.9%) (χ2 = 7.139; p < 0.01), both men and women have a similar educational background with no significant intergroup difference. All except one in the men’s (95.20%) sub group, were married, compared to 76.19% of women. Roughly half of the participants (52.4%) came from mixed villages, a third (34.9%) from mixed cities, and the rest (12.7%) came from Muslim villages, with no significant difference between men and women (Table 1). The patient’s association with a particular ethnic/religion community determined one’s ethnic group; Muslim, Christian or Druze, regardless of self-reporting as living a secular lifestyle. These corresponded to a population in which two-thirds were Muslim (64.5%), with the remaining third divided between Druze (19.4%) and Christians (16.1%), without any significant differences between men and women (Table 1). Unemployment was higher among the Muslim group (71.42%), as compared to Christian (28.58%) and Druze (0%) groups.
Psychiatric diagnosis of PTSD and comorbidities
Comorbidities by sex: Overall, 62 out of 75 participants diagnosed with chronic PTSD were included in the study. Twenty-six percent of the participants receive mental treatment at the Psychiatric Ward during the war, 41% six months following the end of the war, and 33% received treatment 6-12 months after the war ended. Only 3 participants (4%) were not classified as having a comorbid disorder to PTSD, and had their data removed from further analysis; resulting in an unusually high rate of GAD and/or MDD comorbidities with PTSD (96%). The proportion of women participants (66.7%) was significantly higher as compared to men (33.3%) (Binomial test sig= 0.11). The overall PTSD comorbidity exhibited the following distribution: 46% GAD, 33% MDD and 21% GAD+MDD.
Men and women differ significantly only regarding their GAD comorbidity, with women having higher rates of comorbid GAD (χ2(2) =7.759, α<0.01; (Table 2).
Table 2: PTSD Comorbidities by sex.
| PTSD Subclinical Tendencies | Male (n=20) | Female (n=42) | P value |
|---|---|---|---|
| Post Traumatic Anxiety (GAD) | 33.30% | 52.40% | 0.01 |
| Post Traumatic Depression (MDD) | 38.10% | 31.00% | n.s |
| Post Traumatic Anxiety Depression (GAD+MDD) | 28.60% | 16.70% | n.s |
Comorbidities by Religious Affiliation
The GAD comorbidity significantly differs between the Muslim, Christian and Druze groups (60.7%, 25% and 14.3% respectively, χ2(2) =9.929, α<0.01). Such a significant difference also appears for the MDD comorbidity in these groups (66.7%, 4.8% and 28.6% respectively, χ2(2) =12.286, α<0.01; (Table 3). Moreover, a triple comorbidity (GAD, MDD and PTSD) was also found significantly different between Muslims and either Christians or Druze, with Muslims exhibiting a higher rate of triple comorbidity than the other two groups (χ2(2) =4.455, α<0.05). Therefore, it is noticeable that Muslims dominate all three comorbidity categories (GAD, MDD and triple comorbidities).
Table 3: PTSD Comorbidities by Ethnic group.
| PTSD Comorbidity | Muslim (n=40) | Christian (n=10) | Druze | P Value |
|---|---|---|---|---|
| (n=12) | ||||
| Post Traumatic Anxiety (GAD) | 60.70% | 25.00% | 14.30% | 0.007 |
| Post Traumatic Depression (MDD) | 66.70% | 4.80% | 28.60% | 0.002 |
| Post Traumatic Anxiety Depression (GAD+MDD) | 69.20% | 15.40% | 15.40% | 0.035 |
Comorbidities Cross-correlations
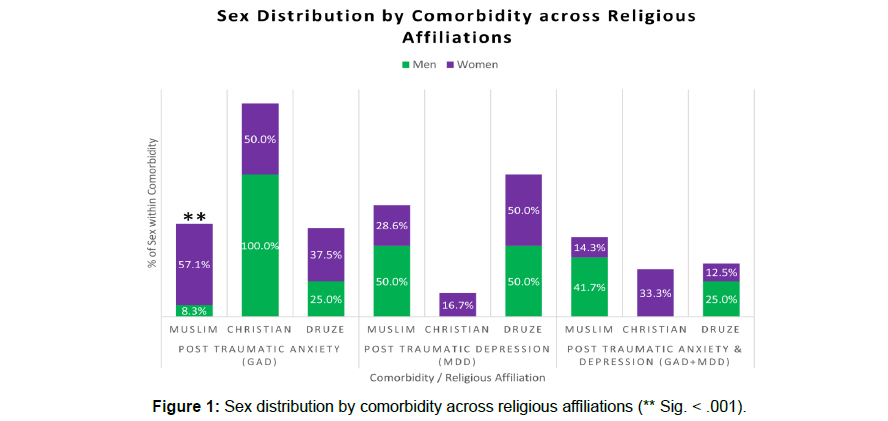
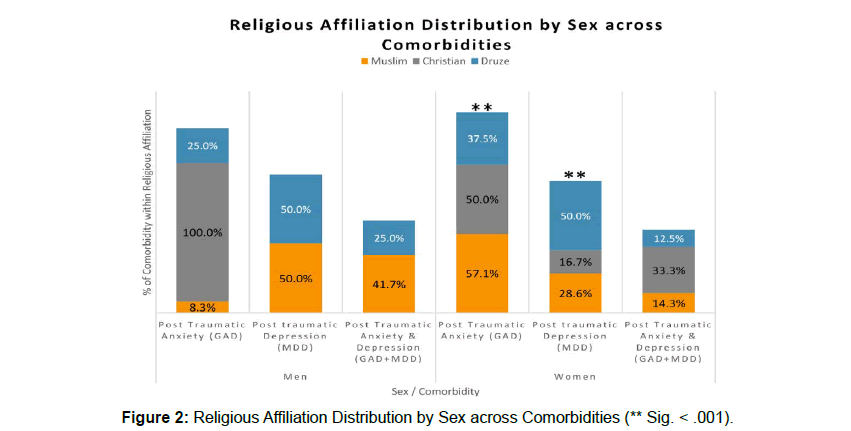
There was a significant difference in the proportion of men and woman across the different religious affiliations (Fisher’s p=7.183, α=0.013, phi=.527; (Figure 1), showing that Muslims’ GAD comorbidity is manifested significantly more in women than in men (χ2 = 13.235; p < 0.001; Figure 1). Correspondingly, in women across different religious affiliations, the GAD comorbidity is manifested significantly more in Muslims than Druze (χ2 = 15.364; p < 0.001; (Figure 2). Druze women were found to manifest significantly higher MDD comorbidity rates than Muslim and Christian women (χ2 = 5.7; p < 0.05). Additionally, Muslim women had significantly higher MDD comorbidity rates than Christian women (χ2 = 5.44; p < 0.02; (Figure 2).
Discussion
This pilot study provides a detailed characterization of the warrelated chronic PTSD in the different Arab ethnic groups in Northern Israel, focusing on comorbidity, and sociodemographic aspects.
Large-scale community surveys, had demonstrated that mental health service usage is significantly associated with several variables including demographic characteristics, attitudes toward treatment, mental health diagnoses, and accessibility [26-30].
Our preliminary findings specifically contribute to the accumulating evidence regarding the ethnic and sex differences in comorbidity distribution. To date, most of the studies reporting PTSD comorbidity rates addressed the Arab population, although comprised of different ethnic and religious groups, as a single homogeneous group. Our results reflect diversities between sexes, where women across ethnicities varied in comorbidity distribution, while no such differences were found among men, who were more homogeneously distributed.
Sociodemographic characteristics by sex
The participant’ record data revealed that twice as many women applied for treatment at the EMMS hospital Psychiatric Ward, as did men. This finding is in line with several population-based surveys that women are significantly more likely to seek care for an emotional problem or a psychiatric disorder than men [31-33]. A possible explanation is that women are more likely than men to develop PTSD following exposure to trauma, and, as a result, their tendency of applying for mental health aid are nearly twice as those of men [18]. Additionally, different studies found that the rates and severity of depression and anxiety were higher in young women than in young men [34,35]. These findings are in line with studies conducted in Arab countries, indicating that university students are more likely to encounter mental health problems, and that women showed favorable attitudes toward seeking professional help [36- 38]. Moreover, most men who applied for mental health aid were married, whereas the percentage of married women was smaller. It is worth mentioning, that men in our study had a much higher rate of employment than the women (Table 1). The current results are also supported by the hospital’s psychiatric staff, who claimed that the majority of men who did apply for treatment, did not come on their own, but rather at the entreaty of their spouses because of the husbands’ high level of disability and distress, which may additionally have a harmful effect on the husbands’ employment status.
This is in line with studies demonstrated that women are more likely to encourage their spouse to obtain mental health care [39]. It was shown that men tend to ignore both their own and their spouse’ health problems in general, and mental health problems in particular [40,41]. One possible explanation for the relatively low rates of men as compared to women applying for mental health services, is the Arab men’s tendency to underreport their mental distress due to stigmatization or due to traditional masculine gender roles [40-42]. This point of view was strengthened by the EMMS psychiatric staff assumption, regarding the reluctance of men to seek mental health services, due to its social unacceptability in their communities. This attitude toward mental treatment is not only found in Arab men, but also widely common among men in other communities [43,44]. Previous studies have demonstrated that Arab participants who develop mental disorders typically wait for a long period of time before seeking healthcare [45]. Data from the Michigan Behavioral Risk Factors Surveillance Survey indicated that Arab Americans experienced poor mental health days, yet they were less likely to report a physician-diagnosed depression disorder [46]. There is a common hypothesis that there is a high level of misconceptions regarding causes and treatment of mental illness among the Arab communities.
Regarding gender differences in receiving treatment [20], found that men in Arab communities tend to underreport their mental distress following traumatic events, due to stigmatization and fear of being perceived as weak and less masculine. Additionally, men were found to associate stigma with mental illness more than women. Thus, negative emotions are perceived as a sign of weakness, discouraging men from reaching out to friends for emotional support [47].
Considering Comorbidities alone and across religions
Earlier studies found that MDD comorbidity rates in PTSD participants ranged from 21% to 94% [10,12,48-50], while GAD ranged from 39% to 97% [9-12]. Additionally, a significant number of participants (11–67%) satisfy the criteria for triple comorbidity at some point in their lives [10,13].
The high comorbidity rate among PTSD participants found in our study (96%) is similar to the high rate of mental comorbidities (97.4%) found in a study conducted [51] on PTSD war veterans in Bosnia-Herzegovina, which concluded that “chronic PTSD in war veterans was almost always accompanied by multiple psychiatric and often somatic comorbidities”. These high comorbidity rates for mental disorders among PTSD populations even exceeds the high comorbidity rates found in the renowned classic study [52], who demonstrated that 82.8% of the PTSD sample met criteria for at least one additional psychiatric disorder. Since the majority of our study’s population is of Muslim ethnicity, the high prevalence of PTSD comorbidity can be attributed to the degree of acculturation (assimilation in society) that is lower than the average in the general population in that region [53]. Within our study’s population 46% exhibited comorbid anxiety, in agreement with previous studies showing the proportion of PTSD comorbid anxiety to range between 39% and 97% [8-10,12,54,55] and 33% of the population which exhibited comorbid depression, in accord with PTSD comorbid depression, reported in studies to range between 21% and 94% [8-10,12,48-50]. Twenty one percent of our study’s population had triple comorbidity, in accordance with studies demonstrating that 11% to 67% of PTSD participants suffer from a triple comorbidity, having depression and anxiety disorders in addition to PTSD [8-10,13]. Muslim population in general dominates all comorbidity categories. Muslims’ comorbid anxiety was found to be significantly higher than Christians and Druze (60.7%, 25.0% and 14.3% respectively). Comorbid depression was significantly higher in Muslims than in either Christian or Druze populations (66.7%, 4.8% and 28.6% respectively), as well as the triple comorbidity rates being significantly higher in Muslims than for either Christians or Druze (69.2%, 15.4% and 15.4% respectively). The Muslims’ triple comorbidity rates, considered to be the more challenging to diagnose and treat [56], exceeds even the high rates reported by [8], at 67% for the general population. A possible explanation for such a high comorbidity rate among Muslims, is that Muslims in Israel are living in constant tension. Muslims comprise the majority of Arabs within the Israeli Arab subpopulation (Jewish 74.7%, Muslim 17.7%, Christian 2%, Druze 1.6%, other 4%) [1]. They are exempt from the compulsory Israeli military service, in terms of the inherent conflict of interests [57]; only a very small percentage of them volunteer to serve in the military. As most Muslims do not serve in the Israel Defense Forces (IDF), they are discriminated by the government’s predominant criterion of military service in receiving benefits, mostly financial in nature, such as loans for housing. As Muslims live in continuous tension, and due to their existential conflict, they are highly prone to develop the most severe form of PTSD, following a traumatic event. The above, is in contrary to the Christians, who live a more western style of living, and are better assimilated into Israeli society (some even serve in the Israeli Defense Forces). Moreover, a study examining mental health help-seeking among Arab university students in Israel, found that Christians perceive less stigma towards mental health systems than their Druze or Islamic counterparts, believe less in traditional healing etiology, and used traditional healing less than Muslim and Druze respondents [58].
Similarly, the Israeli Druze men, most resemble the Jews in terms of their collective identity, most of them serve in the Israeli Defense Forces and vote (81%) for Zionist parties, as opposed to Muslims and Christians, who tend to vote primarily for Arab parties [2,57,59] and as such, are eligible for most of the country’s financial benefits. Thus, Druze men are better assimilated into Israeli society, and in contrast to the Muslims, they do not experience high tension in society, exhibiting lower degrees of anxiety and depression comorbidities.
Comorbidities across the sexes and between and within religions
A number of epidemiological studies have shown that women with PTSD are twice as likely to exhibit depression and anxiety disorders when compared to men with PTSD [60,19]. In contrast to the above study, the current study did not find such significant differences in MDD comorbidity between men and women. Yet, in line with the above, we found that women from the Arab population significantly exhibit more anxiety than men. These results support a study characterizing the Arab population, where anxiety disorders were found to be more prevalent in women than in men [20]. In the current study’s female population, Druze had significantly higher rates of MDD than Muslims and Christians. Similar to Muslim men, Druze women do not serve in the IDF, are less assimilated into the Israeli societal identity, and to an even lesser extent involved (than Druze men) in governmental positions and the military. One possible explanation for such findings may be that Druze women are less extroverted, and exhibit high levels of social inhibition, as they conform to the traditional norms of the Druze secret faith, thus, tending to keep traumatic event to themselves, and therefore exhibit a higher rate of depression patterns. Moreover, they are not encouraged to seek treatment or therapy for themselves [61,62]. A Study that assessed mental health service needs among Israeli Muslim and Druze adolescents and their mothers in the Galilee found that the main obstacle to seeking help for the Druze mothers was ‘reprisal by the authorities’, even though Druze are much more integrated into Israeli society; they may still be wary of jeopardizing their children’s future chances in the IDF by having been diagnosed or labelled with, or treated for, a psychiatric problem. Muslim mothers were more concerned about stigma, and showed higher distrust in professionals [63]. The latter should be taken in the context of mental health services intervention or treatment involving a Jewish consultant with an Arabic patient, specifically Muslim, which necessarily puts the clinical intervention into the crucible of the political dynamic [64].
Muslim women had significantly higher MDD comorbidity rates than Christian women. A possible explanation is that Muslim women are less assimilated into Israeli society and live a more traditional lifestyle, whereas Christian women are better assimilated into the Israeli western lifestyle, and more involved in professional roles [59] in Israeli society, therefore are less subject to conflicts and stress in society. Accordingly, their depression comorbidity rates are lower than those of the Muslim and Druze women. GAD comorbidity in women is manifested significantly more in Muslims than either Druze or Christians.
When comparing the comorbidity distribution between sexes in each of the ethnic groups, a significant difference was found only among the Muslims, where women had significantly higher GAD rates than men (57.1% and 8.3% respectively).
While we found that women had a six-fold higher GAD rate than men, it is most reasonable to assume that the actual portion of GAD in Muslim men is higher than the value reported. The above result is also in accordance with findings indicating that anxiety disorders such as GAD are twice as prevalent among women [19].
Two main phenomena corroborate our findings: stigmatization and assimilation (acculturation).
Stigmatization corroborates with our results of a lower (than average) proportion of men than women in our study sample, as well as the reports by the attending clinical staff. This is supported by studies indicating culturally-related stigmatization of help-seeking behaviors towards mental healthcare [65,66,67].
Assimilation (acculturation) corroborates the proportion of PTSD comorbidity by ethnicity. This is supported by studies that found correlations between: ethnicity and mental health through sense-ofcoherence [68], low degree of acculturation and higher number of symptoms [69], as well as the prevalence of PTSD comorbidities and ethnic minorities [70].
Considering the above results for improving mental health care in diverse ethnicities and sexes, it is of upmost importance to integrate cultural and ethnic aspects into the practitioners’ professional training [64,71]. Such addition may raise the community’s engagement within this practice, to accommodate cultural and specific needs, taking into account ethnic group and gender preferences and beliefs [72]. For instance, a study examining single-session-treatments (OST) and a culturally adaptive OST, among phobic Asian Americans, found the culturally adapted OST to be superior for this specific group [73]. Such practical innovations for reducing PTSD stigmatization were shown to be beneficial among combat veterans, through peer-based support groups, as the veterans believed that only other veterans could truly understand their experience. It was also shown that such intervention enables them to better engage in treatment [74].
A well-tailored, elaborate program for providing optimally personalized mental health interventions, should consider each of the groups’ ethnic characteristics, sociodemographic and gender-related insights for diagnosis and treatment of these unique populations. For example, a meta-analysis of large number of studies indicate the potential of CBT, both in face-to-face settings and via the internet, as an efficacious and acceptable intervention model for the treatment of anxiety, depression and PTSD among Arab populations [75]. It is imperative to establish community intervention programs, to overcome the cultural trend where men tend to underreport their psychological distress, through enhancing awareness and increasing mental health-care utilization and treatment engagement. Moreover, gender norms in each culture should be considered when establishing intervention and treatment programs. In some cultures, females must be accompanied by their husbands in public, which can limit their access to professional help in instances where they do not want their husband to know about their difficulties, or if their husband is unwilling or unable to accompany them to treatment [76,77].
Limitation and Future studies
One of the prominent limitations of this study is its sample size. In our study, the sample included more women than men, as the latter are less likely to seek medical help, due to cultural influences. Additionally, it should be noted that the size of the ethnic groups indeed reflects their distribution in the sampled geographical area, where there is a higher concentration of Muslims in the population compared to Druze and Christians. Consequently, several subdivisions were not sufficiently large enough to obtain statistically significant analysis. To further substantiate the above findings, future studies should approach hospitals serving larger populations (in metropolitan areas), using the specific divisions suggested herein. Future studies are recommended to consider each of the ethnic groups’ distinctive characteristics, and avoid treating them homogeneously, in contrast to the customary approach.
It is also recommended that future studies should examine culture specific factors such as social support, social and cultural assimilation. Moreover, longitudinal studies are essential in the Arab population to monitor mental health progression and recovery in relation to various types of treatments.
Conclusion
Up to date, most of the studies reporting PTSD comorbidity rates, addressed the Arab population, which comprise of different ethnic and religious groups and sexes, as a single homogenous group. Our results reflect diversities between ethnicities & sexes in the Arab population in Israel, where women across ethnicities exhibited distinctive comorbidity distributions of GAD and MDD, while no such differences were found among men, who were more homogenously distributed across the three comorbidities examined.
These findings highlight the need of further studies taking into consideration the sex and the groups’ distinctive cultural and ethnic characteristics and avoid regarding the Arab population homogeneously. Consequently, tailored personalized mental health interventions and treatments are essential to meet the distinct and unique requirements of each ethnic group in sex-depended manner.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Acknowledgments
We would like to thank the EMMS hospital Psychiatric ward physicians, for their outstanding research assistance and for providing their professional insights.
References
- Central Bureau of Statistics, “Population of Israel on the Eve of 2019,” 2019. https://www.cbs.gov.il/he/mediarelease/DocLib/2018/394/11_18_394b.pdf (accessed Nov. 08, 2019).
- Zeedan R (2019) “The Role of Military Service in the Integration/Segregation of Muslims Christians and Druze within Israel.” Societies, 9 (1): 1
- Am ara M, Schnell I (2004) “Identity repertoires among Arabs in Israel,” J Ethn Migr Stud. 30(1): 175–193.
- Yonay Y P, Yaish M, Kraus V (2015) Religious Heterogeneity and Cultural Diffusion The Impact of Christian Neighbors on Muslim and Druze Women’s Participation in the Labor Force in Israel. Sociology, 49 (4): 660–678.
- Lewin A C (2012) Marriage patterns among Palestinians in Israel. Eur. J Popul Eur Démographie, 28(3): 359–380.
- Firro K (2014) The Druzes in the Jewish state. A brief history, 64.
- Halabi R (2014) Invention of a nation The Druze in Israel. J Asian Afr Stud, 49 (3) 267–281.
- Ginzburg K, Ein-Dor T, Solomon Z (2010) Comorbidity of posttraumatic stress disorder, anxiety and depression: A 20-year longitudinal study of war veterans. J Affect Disord, 123 (1–3): 249–257.
- Mayou R, Bryant B, Ehlers A (2001) Prediction of psychological outcomes one year after a motor vehicle accident. Am J Psychiatry, 158 (8): 1231–1238
- Hashemian F, Khoshnood K, Desai M M, Falahati F, Kasl S, et al. (2006) Anxiety, depression, and posttraumatic stress in Iranian survivors of chemical warfare. JAMA, 296 (5): 560–566.
- Mcmillan KA, Sareen J, Asmundson GJG (2014) Social Anxiety Disorder Is Associated With PTSD Symptom Presentation: An Exploratory Study Within A Nationally Representative Sample. J Trauma Stress, 27(5): 602–609
- Sundquist K, Johansson LM, DeMarinis V, Johansson SE, Sundquist J, et al. Posttraumatic stress disorder and psychiatric co-morbidity: Symptoms in a random sample of female Bosnian refugees. Eur Psychiatry,. 20 (2): 158–164.
- Brady K T, Clary CM (2003) Affective and anxiety comorbidity in post-traumatic stress disorder treatment trials of sertraline. Compr Psychiatry, 44(5): 360–369
- Friedman MJ, Resick PA, Bryant R A, Strain J, Horowitz M, et al. (2011) Classification of trauma and stressor-related disorders in DSM-5. Depress Anxiety, 28 (9): 737–749
- Ayazi T, Lien L, Eide AH, Ruom M M, Hauff E, et al. (2012) What are the risk factors for the comorbidity of posttraumatic stress disorder and depression in a war-affected population? a cross-sectional community study in South Sudan. BMC Psychiatry, 12 (1): 175
- Sher L (2005) The concept of post-traumatic mood disorder. Med Hypotheses, 65 (2): 205–210.
- Donnell ML O, Creamer M, Pattison P, (2004) Posttraumatic stress disorder and depression following trauma: understanding comorbidity. Am J Psychiatry, 161(8): 1390–1396.
- Zlotnick C, Zimmerman M, Wolfsdorf BA, Mattia JI (2001) Gender differences in patients with posttraumatic stress disorder in a general psychiatric practice. Am J Psychiatry, 158(11): 1923–1925.
- Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, et al. (2008) Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry, 65 (7): 805–815.
- Tanios C Y, Abou-Saleh M T, Karam A N, Salamoun MM, Mneimneh Z N, et al. (2009) The epidemiology of anxiety disorders in the Arab world A review. J Anxiety Disord, 23 (4): 409–419.
- Shachar-Dadon A, Gueron-Sela N, Weintraub Z, Maayan-Metzger A, Leshem v, “Pre-Conception War Exposure and Mother and Child Adjustment 4 Years Later. J Abnorm Child Psychol, 45 (1): 131–142
- Ron P (2016) The Relationship Between Background Characteristics and Death Anxiety in Times of War: A Comparison Between Three Generations Arab and Jewish Families in Israel. Community Ment Health J, 52 (8): 1123-1132.
- Spitzer R L, Gibbon M E, Skodol A E, Williams J B W, First M B, et al. (2002) DSM-IV-TR casebook A learning companion to the diagnostic and statistical manual of mental disorders (text rev.). American Psychiatric Publishing, Inc.
- Lobbestael J, Leurgans M, Arntz A (2011) Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II). Clin Psychol Psychother, 18(1): 75–79.
- Zanarini M C (2000) The Collaborative Longitudinal Personality Disorders Study: reliability of axis I and II diagnose. J Pers Disord, 14(4): 291–299.
- Elhai J D, Ford J D (2007) Correlates of Mental Health Service Use Intensity in the National Comorbidity Survey and National Comorbidity Survey Replication. Psychiatr Serv, 58(8): 1108–1115.
- Lewis S F (2005) Assault, psychiatric diagnoses, and sociodemographic variables in relation to help-seeking behavior in a national sample of women. JTrauma Stress, 18(2): 97-105.
- Lin E, Parikh S V (1999) Sociodemographic, clinical, and attitudinal characteristics of the untreated depressed in Ontario. J Affect Disord, 53(2): 153-62.
- Parslow R A, Jorm A F (2000) Who uses mental health services in Australia? An analysis of data from the National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry.
- Wang P S, Lane M, Olfson M, Pincus H A, Wells K B, et al. (2005) Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiatry, 62(6): 629–640.
- Bland R C, Newman S C, Orn H (1990) Health care utilization for emotional problems: results from a community survey. Can J Psychiatry, 35(5): 397–400.
- Drapeau A, Boyer R, Lesage A (2009) The influence of social anchorage on the gender difference in the use of mental health services. J Behav Health Serv Res, 36(3): 372–384
- Leaf PJ, Bruce M L (1987) Gender differences in the use of mental health-related services: a re-examination. J Health Soc Behav,28(2): 171–183.
- Ohannessian C M, Lerner R M, von Eye A, Lerner J V (1996) “Direct and indirect relations between perceived parental acceptance, perceptions of the self, and emotional adjustment during early adolescence. Fam Consum. Sci Res J, 25(2): 159–183
- Afifi M (2006) Depression in adolescents: gender differences in Oman and Egypt. EMHJ-Eastern Mediterr Heal Journal, 12(1-2): 61-71
- Al-Samadi A A (1994) Yarmouk University students’ attitudes toward counseling. Derasat, 21(4): 277–297.
- Al-Darmaki FR (2004) Counselor training, anxiety, and counseling self-efficacy: Implications for training psychology students from the united arab emirates university. Soc Behav Pers
- Soliman A M (1993) Choice of helpers, types of problems and sex of helpers of college students. Int J Adv Couns, 16: 67–79.
- Reczek C, Gebhardt-Kram L, Kissling A, Umberson D (2018) Healthcare Work in Marriage: How Gay, Lesbian, and Heterosexual Spouses Encourage and Coerce Medical Care. J Health Soc Behav.
- Wendt D, Shafer K (2014) Gender and Attitudes about Mental Health Help Seeking: Results from National Data. Heal Soc Work, 41(1)
- Addis M E, Mahalik JR (2003) Men, Masculinity, and the Contexts of Help Seeking. American Psychologist,58(1): 5-14.
- Tang M O T, Oliffe J L, Galdas P M, Phinney A, Han CS et al. (2014) College men’s depression-related help-seeking: A gender analysis. J Ment Heal, 23(5): 219-24
- Gulliver A, Griffiths K M, Christensen H (2010) Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10: 113.
- Seidler Z E, Dawes A J, Rice S M, Oliffe J L, Dhillon H M, et al. (2016) The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49: 106-118.
- Charara R (2017)“The burden of mental disorders in the eastern mediterranean region, 1990-2013. PLoS One, 12(1): e0169575.
- Abuelezam N N, El-Sayed A M (2018) Objective and subjective poor mental health indicators among Arab Americans in Michigan: a population-based study. Ethn Heal, 26(2): 225-234
- Pirkis J, Spittal M J, Keogh L, Mousaferiadis T, Currier D, et al. (2017) Masculinity and suicidal thinking. Soc Psychiatry Psychiatr Epidemiol, 52(3): 319-327.
- Ginzburg K (2006) Comorbidity of PTSD and depression following myocardial infarction. J Affect Disord, 94 (1–3): 135–143.
- Salcioglu E, Basoglu M, and M. Livanou (2003) Long-term psychological outcome for non-treatment-seeking earthquake survivors in Turkey. J Nerv Ment Dis, 191(3): 154–160.
- Frayne S M (2004) Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med, 164(12): 1306–1312
- Klaric M, Lovric S, Kresic Coric M, Galic K, Coric S, et al. (2017) Psychiatric comorbidity and PTSD-related health problems in war veterans: Cross-sectional study. Eur J Psychiatry, 31(4): 51–157
- Breslau N, Davis G C, Andreski P, Peterson E (1991) Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry, 48(3): 216–222
- Sharabi (2018) Ethno-religious groups work values and ethics: the case of Jews, Muslims and Christians in Israel. Int Rev Sociol, 28 (1): 171–192.
- McFarlane AC, Papay P (1992) Multiple diagnoses in posttraumatic stress disorder in the victims of a natural disaster. The Journal of nervous and mental disease, 180(8): 498–504.
- Zayfert C (2002) Comorbid anxiety disorders in civilians seeking treatment for posttraumatic stress disorder. J Trauma Stress, 15(1): 31–38.
- Coplan J D, Aaronson C J, Panthangi V, Kim Y (2015) Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches. World J psychiatry 5 (4): 366- 378
- Smooha S (1990)Minority status in an ethnic democracy: The status of the Arab minority in Israel. Ethn Racial Stud, 13(3): 389–413.
- Al-Krenawi A, Graham J R (2011) Mental health help-seeking among Arab university students in Israel, differentiated by religion. Ment Heal Relig Cult, 14(2).
- Landau J M (1969) Royal Institute of International Affairs., The Arabs in Israel: a political study. published under the auspices of the Royal Institute of International Affairs [by] Oxford U.P.
- Breslau N, Davis C G, Patricia A, Peterson E, Schultz L, et al. (1997) Sex differences in posttraumatic stress disorder. Arch Gen Psychiatry, 54 (11): 1044–1048.
- Janet D, Carter D, Roger T, Mulder (2014) Parental stress in the NICU: The infl uence of personality, psychological, pregnancy and family factors. Personal Ment Health. 95: 86–95.
- van Krugten F C W (2017) Indicators of patients with major depressive disorder in need of highly specialized care: A systematic review. PLoS One, 12 (2): e0171659.
- Daeem R (2019) Barriers to help-seeking in Israeli Arab minority adolescents with mental health problems: Results from the Galilee study. Isr J Health Policy Res
- Al-Krenawi A, Graham J R (2005) Mental health practice for the Muslim Arab population in Israel. Underst Gend Cult Help Process, 68–83.
- Al Ali N M, Alqurneh M K, Dalky H, Al-Omari H (2017) Factors affecting help-seeking attitudes regarding mental health services among attendance of primary health care centers in Jordan. Int J Ment Health, 46(1): 38–51.
- Kayrouz R (2015) Intergenerational and cross-cultural differences in emotional wellbeing, mental health service utilisation, treatment-seeking preferences and acceptability of psychological treatments for Arab Australians. Int J Soc Psychiatry, 61(5): 484–491.
- Clement S (2015) What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med, 45(1): 11–27.
- Baron-Epel O, Berardi V, Bellettiere J, Shalata W (2017) The Relation Between Discrimination, Sense of Coherence and Health Varies According to Ethnicity: A Study Among Three Distinct Populations in Israel. J Immigr Minor Heal, 19 (6): 1386–1396
- Asnaani A, Hall-Clark B (2017) Recent developments in understanding ethnocultural and race differences in trauma exposure and PTSD. Curr Opin Psychol, 14: 96–101.
- Watkins D C, Assari S, Johnson-Lawrence V (2015) Race and Ethnic Group Differences in Comorbid Major Depressive Disorder, Generalized Anxiety Disorder, and Chronic Medical Conditions. J racial Ethn Heal disparities, 2(3): 385–394.
- Roberts A L, Gilman S E, Breslau J, Breslau N, Koenen K C, et al. (2011) Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med, 41(1): 71–83.
- Van Loon A, Van Schaik A, Dekker J, Beekman A (2013) Bridging the gap for ethnic minority adult outpatients with depression and anxiety disorders by culturally adapted treatments. J Affect Disord, 147 (1–3): 9–16.
- Pan D, Huey S J, Hernandez D (2011) Culturally adapted versus standard exposure treatment for phobic Asian Americans: Treatment efficacy, moderators, and predictors. Cult Divers Ethn Minor Psychol, vol. 17(1): 11–22.
- Mittal D, Drummond K L, Blevins D, Curran G, Corrigan P, et al. (2013) Stigma Associated With PTSD: Perceptions of Treatment Seeking Combat Veterans. Psychiatr Rehabil J, 36(2): 86–92.
- Kayrouz R, Dear B F, Kayrouz B, Karin E, Gandy M, et al. (2018) Meta-analysis of the efficacy and acceptability of cognitive-behavioural therapy for Arab adult populations experiencing anxiety, depression or post-traumatic stress disorder. Cognitive Behaviour Therapy.47(5): 412-430.
- Gearing R E (2013) Adaptation and translation of mental health interventions in Middle Eastern Arab countries: A systematic review of barriers to and strategies for effective treatment implementation. Inter J Social Psychiatry, 59(7): 671-81.
- Al-Krenawi A, Graham J R (1999) Gender and biomedical/traditional mental health utilization among the Bedouin-Arabs of the Negev. Cult Med Psychiatry, 23(2): 219-43.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi