Editorial, Analg Resusc Curr Res Vol: 5 Issue: 1
CYP2D6 Polymorphisms and Response to Codeine and Tramadol
| Mark I Johnson1,2* and Helen Radford1,3 | |
| 1Faculty of Health and Social Sciences, Leeds Beckett University, United Kingdom | |
| 2Leeds Pallium Research Group, Leeds, United Kingdom | |
| 3Leeds Centre for Neurosciences, Leeds Teaching Hospitals NHS Trust, United Kingdom | |
| Corresponding author : Mark I Johnson Faculty of Health and Social Sciences, Leeds Beckett University, City Campus, Leeds LS1 3HE, United Kingdom Tel: +44 113 2063375 Fax: 0113 2063314 E-mail: M.Johnson@leedsbeckett.ac.uk |
|
| Received: March 09, 2015 Accepted: March 11, 2016 Published: March 15, 2016 | |
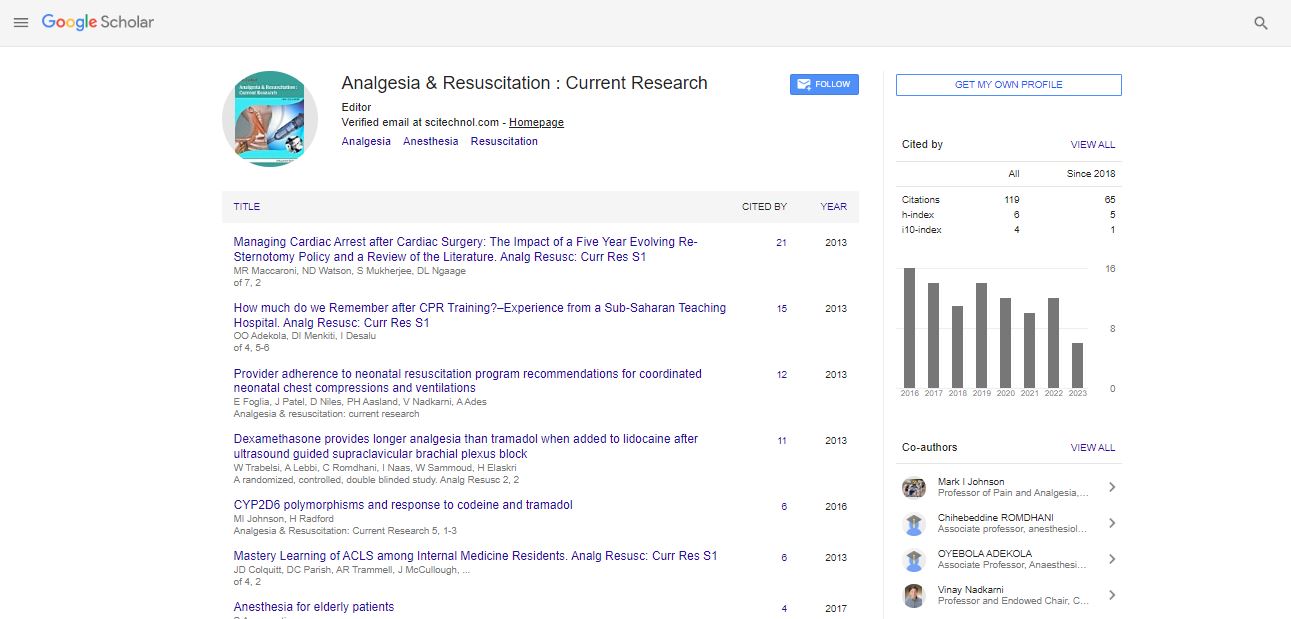
| Citation: Johnson MI, Radford H (2016) CYP2D6 Polymorphisms and Response to Codeine and Tramadol. Analg Resusc: Curr Res 5:1. doi:10.4172/2324-903X.1000e106 |
Abstract
CYP2D6 Polymorphisms and Response to Codeine and Tramadol
The science of how an individual’s genotype affects the body’s response to drugs, termed pharmacogenomics, began in the late 1950’s. Since then the promise that medicines could be tailored to the individual instead of the one-size-fits-all approach has been heralded as the future of medicine [1-3]. However, pharmacogenomics has made very little impact on the practice of pain management at the point of care and clinicians still rely on a ‘trial and error’ approach to prescribing and dosing. This carries the risk of adverse events due to toxicity and sub-optimal analgesic response [4-6]. The largest epidemiological study of adults with chronic pain in Europe to date found that 40% of participants reported inadequate pain management by medication and 44% of participants reported that their medications were regularly changed due to lack of efficacy [7]. In 23% of individuals pain was managed by codeine or tramadol. Codeine and tramadol are prodrugs and require biotransformation primarily in the liver to active metabolites for analgesic efficacy [8]. The purpose of this Editorial is to discuss CYP2D6 polymorphisms and codeine non-response in pain populations.
Keywords: Polymorphisms; Codeine; Tramadol
Introduction |
| The science of how an individual’s genotype affects the body’s response to drugs, termed pharmacogenomics, began in the late 1950’s. Since then the promise that medicines could be tailored to the individual instead of the one-size-fits-all approach has been heralded as the future of medicine [1-3]. However, pharmacogenomics has made very little impact on the practice of pain management at the point of care and clinicians still rely on a ‘trial and error’ approach to prescribing and dosing. This carries the risk of adverse events due to toxicity and sub-optimal analgesic response [4-6]. The largest epidemiological study of adults with chronic pain in Europe to date found that 40% of participants reported inadequate pain management by medication and 44% of participants reported that their medications were regularly changed due to lack of efficacy [7]. In 23% of individuals pain was managed by codeine or tramadol. Codeine and tramadol are prodrugs and require biotransformation primarily in the liver to active metabolites for analgesic efficacy [8]. The purpose of this Editorial is to discuss CYP2D6 polymorphisms and codeine non-response in pain populations. |
Pharmacogenomics of CYP2D6 |
| It has been estimated that 25-30% of prescribed drugs involve CYP2D6 [9]. CYP2D6 has the largest polymorphic variability of all the CYP genes with over 100 known allelic variants identified. The rate of metabolism of CYP2D6 substrates increases significantly with each functional copy of the allele present in an individual, so individuals with multiple copies of the CYP2D6 gene have greaterthan- normal CYP2D6 enzyme function [2]. |
| Codeine (3-methylmorphine) is an opiate that is typically administered orally and indicated for mild to moderate pain, cough and diarrhea. Codeine is available as a single-ingredient drug and in combination with paracetamol (co-codamol), ibuprofen, and aspirin (co-codaprin). Up to 15% of codeine is converted into morphine, the active metabolite, by the enzyme cytochrome P450 2D6 (CYP2D6). Tramadol is metabolized by CYP2D6 and cytochrome P450 3A4 (CYP3A4) to the active metabolite O-desmethyltramadol which is an opioid with analgesic properties. An individual’s capacity to metabolize codeine and tramadol into active metabolites is known to vary considerably because of genetic polymorphism resulting in phenotypical variability of the CYP2D6 enzyme. The CYP2D6 enzyme is encoded by the CYP2D6 gene and part of the Cytochrome P450 superfamily of haem-containing mono-oxygenases. There are 17 cytochrome P450 families in man, encoded by 57 functional genes. Six cytochrome P450 enzymes having an important role in drug metabolism are CYP1A2, CYP2C19, CYP2C9, CYP2D6, CYP2E1, and CYP3A4. Genetic polymorphisms of cytochrome P450 (CYP) causes variability in drug pharmacokinetics and response. |
| Published prescribing guidelines give little attention to the impact of pharmacogenomics on response to analgesics [6,10], although the British National Formulary emphasizes that inter-patient variability in codeine metabolism may result in reduced efficacy or toxicity [11,12]. In the U.K. codeine and tramadol are the second and third most commonly prescribed analgesics for persistent pain respectively. Prescriptions for codeine based drugs has risen by 10.5 percent in primary care settings in the U.K. with a net rise in drug ingredient costs of £10.3 million, from £82.4 in 2011 to £92.7 million in 2012 [13]. Prescriptions of tramadol had been increased by 6.1% although net drug ingredient costs remained stable at £47 million. |
| There is substantial evidence that CYP2D6 polymorphisms are clinically important to many therapeutic areas, and especially pain management [14-23]. Recently, we conducted a service improvement project that analyzed referral letters to a secondary care specialist pain management clinic from primary care physicians (general practitioners) for the potential impact of polypharmacy on CYP2D6 inhibition and phenocopying [24]. We found that 58.7% of referrals were prescribed at least one analgesic prodrug reliant on the function of CYP2D6 for analgesic efficacy. In addition, 29.5% of referrals were co-prescribed at least one CYP2D6 inhibitor with a risk of clinically meaningful drug interactions in 19.9% of patients and a risk of suboptimal analgesic response in 18.75% of patients. We concluded that current prescribing trends posed a risk to the safety of some patients and recommended that prescribers need education about the potential for CYP2D6 inhibition from polypharmacy when prescribing analgesic prodrugs such as codeine and tramadol. Moreover, challenges in translating knowledge about CYP2D6 polymorphisms in chronic pain settings are also relevant for pain associated with trauma, surgery, immobilization, and the use of medical equipment such as endotracheal tubes and catheters in urgent and emergency care and critically ill patients. |
Historical Context of CYP2D6 |
| The CYP2D6 gene was identified in the mid 1970’s through observations of bimodal response in clinical trials of the antiarrhythmic drug sparteine and the anti-hypertensive drug debrisoquine. The majority of participants of clinical studies conducted in the 1970s and 1980s exhibited no side effects as the drugs were metabolized quickly into inactive metabolites and excreted in urine. Nevertheless, a minority of participants experienced side effects such as blurred vision, hypotension and headaches [25-27]. At the time investigators concluded that an unidentified gene that influenced metabolism of the drug was responsible for the inter-individual differences observed. The term debrisoquine/sparteine polymorphism was used to describe the mechanism [28]. In the mid-1980s Distlerath et al. [29] successfully purified and characterized two forms of the CYP2D6 gene and identified poor and extensive (normal) CYP2D6 phenotypes. Since then developments in pharmacogenomics have resulted in extensive research into the polymorphic variability of the CYP2D6 gene, leading to the classification of a further two CYP2D6 phenotypes of intermediate and ultra-rapid [2,23,30]. Ultra-rapid, intermediate and poor metabolizer phenotypes affect clinical response for analgesic prodrugs reliant on CYP2D6. |
The Role of CYP2D6 on the Action of Codeine |
| Four CYP2D6 phenotypic groups of enzyme function have been identified [31-33]: |
| • Ultra-rapid Metabolisers (UM): have greater than expected CYP2D6 enzyme function, so individuals rapidly biotransform codeine and produce excessive levels of morphine resulting in toxicity and a risk of adverse drug reactions |
| • Extensive Metabolisers (EM): have normal CYP2D6 enzyme function, so individuals biotransform codeine normally and produce expected levels of morphine that lie within the therapeutic window within an optimal time frame |
| • Intermediate Metabolisers (IM): have reduced CYP2D6 enzyme function, so individuals are unable to fully biotransform codeine, and produce reduced levels of morphine resulting in suboptimal analgesic response |
| • Poor Metabolisers (PM): have little or no CYP2D6 enzyme function, so individuals are unable to biotransform codeine and produce minimal levels of morphine resulting in little or no analgesic response. |
| The prevalence of CYP2D6 phenotypes due to genetic polymorphism varies according to ethnicity. The UM phenotype is present in approximately 40% of North Africans compared with 5.5% in Caucasians [2,30]. IM phenotypes are present in approximately 25-30% of Asian populations compared with 10-15% in Caucasians [2,30]. Caucasians have the highest prevalence of the PM phenotype at 5-11% compared with 3-5% in Black populations and 1% in Japanese, Chinese, Koreans and Asian populations [34,35]. Therefore, up to 26% of Caucasians lack optimal CYP2D6 function and are categorized as IM or PMs. In the UK the Caucasian population is 48.2 million [36] so up to 12 million individuals may be at risk of sub-optimal response to codeine (7.23 million IMs, 4.82 million PMs) and 2.41 million individuals at risk of morphine toxicity because they are UMs. However, the unavailability of pharmacogenetic screening at the point of care makes it challenging for clinicians to consider the role of pharmacogenomics in response to analgesic prodrugs. The situation is confounded in polypharmacy because some drugs inhibit CYP2D6 function and others induce CYP2D6 function further complicating response to analgesics. |
Polypharmacy and CYP2D6 Polymorphism on Response to Analgesics |
| The function of the CYP2D6 enzyme can be inhibited, and in some instances induced by drugs [37]. The risk of drug interactions from CYP2D6 induction is low with dexamethasone and rifampin being the only drugs with potential for induction [38,39]. The of drug interactions from CYP2D6 inhibition is much higher. Inhibition of CYP2D6 enzyme function during polypharmacy of multiple CYP2D6 substrates or inhibitors results in failure to bioactivate analgesic prodrugs for therapeutic efficacy [38,40-42]. In our service improvement project we found that 29.5% of referrals were coprescribed at least one CYP2D6 inhibitor, with a risk of clinically meaningful drug interactions in 19.9% of patients and suboptimal analgesic response in 18.75% of patients [24]. CYP2D6 inhibition by co-prescription with selective serotonin re-uptake inhibitors (SSRIs) was particularly problematic during polypharmacy. The magnitude of inhibition has been estimated for numerous drugs by the FDA and other organizations [38,40-42]. Fluoxetine or paroxetine are strong CYP2D6 inhibitors producing ~100% reduction in CYP2D6 function, and sertraline and citalopram are moderate CYP2D6 inhibitors producing ~50% reduction in CYP2D6 function. The risk of serotonin syndrome increases with co-prescription of SSRIs with tramadol and fentanyl. |
Clinical Implications |
| Adequate and immediate pain control through carefully considered prescribing reduces patient suffering, medication wastage and healthcare utilization costs. CYP2D6 phenotype is not assessed routinely so clinicians adopt a ‘trial and error’ approach to prescribing that includes increasing doses of analgesic prodrugs and adding pain adjuvants when analgesic response is suboptimal. Some adjuvants are prescribed as primary analgesic agents for neuropathic pain (e.g. anti-depressants (amitriptyline) and anti-convulsants (gabapentin, pregabalin)) but they are also prescribed as a secondary agent in combination with other analgesic drugs for neuropathic and nociceptive pain. The British National Formulary acknowledges risks associated with PM and UM phenotypes being at risk of sub-optimal response and/or adverse drug reactions [12,41]. However no further prescribing guidance or information on CYP2D6 polymorphisms is provided. |
| Clearly, more information is needed, especially with respect to alternative prescribing information and CYP2D6 inhibitors to be avoided. Healthcare professionals need to be proactive in protecting patients from potentially serious adverse events associated with CYP2D6 inhibition. Medication reviews should check for risks of CYP2D6 inhibition, especially when there is medication change. Patients need to be made aware of risks of drug interactions from over the counter medication that could alter CYP2D6 function and affect the efficacy of any prodrugs. There should be continuous professional education for CYP2D6 in pain management prescribers. The International Society of Pharmacogenomics recommends that pharmacogenomics should be integral to the pharmacology curriculum for medical, nursing and pharmacist students [43]. |
Conclusion |
| There is a needs indent for greater awareness of pharmacogenomics especially on CYP2D6 in the field of pain management through education and a need for algorithms to aid prescribing. The development of CYP2D6 screening at the point of care by genotyping and/or phenotyping from, for example, urinary codeine metabolites is necessary to personalize medication to CYP2D6 genetic profile to reduce the risk of sub-optimal analgesia and adverse events due to drug interactions. |
References |
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi