Research Article, J Nanomater Mol Nanotechnol Vol: 5 Issue: 4
Crossing the Blood-Brain Barrier with Antibody-Labeled, Gold-Coated Nanoconjugates: A Preliminary Step in Targeting and Eradicating Brain Tumors
| Marshall Cress1, Angela Spurgeon2, Mark F McLaughlin3,4, Tiffany Remsen4, Douglas C Miller5, J David Robertson3,4 and Paul H Pevsner6* |
| 1Department of Neurosurgery, University of Florida, Gainesville, FL, USA |
| 2Department of Neurosurgery, Department of Surgery, University of Missouri School of Medicine, Columbia, MO, USA |
| 3University of Missouri Research Reactor (MURR), Columbia, MO, USA |
| 4Department of Chemistry, University of Missouri, Columbia, MO, USA |
| 5Department of Pathology and Anatomical Sciences, University of Missouri School of Medicine, Columbia, MO, USA |
| 6Nano Imrad Technology, Inc., Irving, TX, USA |
| Corresponding author : Paul H. Pevsner Nano Imrad Technology, Inc., Irving, TX, USA Tel: 917-514-3339 E-mail: paul.pevsner@dpsemail.com |
| Received: June 13, 2016 Accepted: July 26, 2016 Published: July 31, 2016 |
| Citation: Cress M, Spurgeon A, McLaughlin MF, Remsen T, Miller DC, et al. (2016) Crossing the Blood-Brain Barrier with Antibody-Labeled, Gold-Coated Nanoconjugates: A Preliminary Step in Targeting and Eradicating Brain Tumors. J Nanomater Mol Nanotechnol 5:4.doi:10.4172/2324-8777.1000190 |
Abstract
Crossing the Blood-Brain Barrier with Antibody-Labeled, Gold-Coated Nanoconjugates: A Preliminary Step in Targeting and Eradicating Brain Tumors
This paper shows ultrastructural proof of principle that antibodylabeled nanoconjugates can cross the blood-brain barrier and bind to their targeted antigens. Gold-coated nanoconjugates labeled with monoclonal antibodies targeting brain antigens-specifically, the synaptophysin and glial fibrillary acidic proteins-were injected intravascularly into 45 Balb/c mice. Through electron microscopy a portion of the nanoconjugates were shown to have crossed the blood-brain barrier and become localized either on the intermediate filaments in the astrocytic cytoplasm (anti-glial fibrillary acidic proteins) or presynaptic membranes (anti-synaptophysin). Three of the authors have already reported on a similar and successful use of radioactive nanoconjugates to target antigens in a syngeneic murine lung tumor model using CMT-6 breast cancer cells. This proof of principle supported by concrete evidence does not include an analysis of the mechanism by which the nanoconjugates crossed the blood-brain barrier. The success of targeting proteins in the brain and, by implication, antigens in brain tumors, has immense potential for the treatment of a wide variety of metastases and tumors, including brain cancers such as glioblastoma.
Keywords: Blood-brain barrier; Theranostic targeted nanoconjugates; Brain tumor; Glioblastoma; BBB
Keywords |
|
| Blood-brain barrier; Theranostic targeted nanoconjugates; Brain tumor; Glioblastoma; BBB | |
List of Chemicals |
|
| Lanthanum chloride heptahydrate CID: 165791, Gadolinium chloride hexahydrate CID: 197915, Sodium tripolyphosphate CID: 24455, Tribasic sodium citrate CID: 6224, Gold tetrachloride CID: 27127, Tris (2-carboxyethyl) phosphine hydrochloride CID: 2734570, 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC) CID: 2723939, N-hydroxysuccinimide (sulfo-NHS) CID: 3520574, Lipoamide-dpeg12- acid CAS: 1334172-70-2 | |
Introduction |
|
| A long held goal of neurooncology has been the creation of targeted therapies to attack tumor cells while sparing normal tissue. One promising solution is to use antibodies targeting antigens expressed exclusively by the tumor cells. To that end, theranostic (diagnostic and therapeutic) macromolecules may provide an effective treatment for a wide variety of metastases and tumors, including deadly brain tumors such as glioblastoma. | |
| According to the Central Brain Tumor Registry of the United States (CBTRUS), the most common primary brain tumor is glioblastoma. During the 2006-10 period, 50,872 cases of glioblastoma were registered-an average annual incidence rate of 3.19 cases per 100,000 population [1]. The average life expectancy following initial diagnosis without other treatment is 3-4 months. With optimal surgical excision, external beam radiation, and chemotherapeutic intervention, average life expectancy rises to 12-15 months [2,3]. Sadly, in spite of significant advances in imaging, chemotherapy, and radiation therapy technology, these numbers are only slightly improved over those reported 25 years ago [4,5]. | |
| Although radiation therapy and chemotherapy have modestly improved survival rates for patients with glioblastoma and other central nervous system malignancies, they often damage normal tissues and hence the quality of life. Long-term survivors may suffer such problems as radiation-induced necrosis of brain tissue, chemotherapy-induced leukoencephalopathy, or second malignant neoplasms. A targeted treatment-a scalpel that cuts out the cancer, not a broadsword that attacks both the disease and the patient-is needed. | |
| Crossing the BBB | |
| Antibodies have long been recognized as potential tools to target cancer cells since they can be selected to bind exclusively to tumorspecific antigens. A significant obstacle to such antibody-targeted therapy is the blood-brain barrier (BBB), which was first described by Ehrlich as a barrier blocking the entry of aniline dyes from the circulation into the brain [6]. Lewandowsky introduced the term “blood-brain barrier”, and Goldman confirmed its existence [7,8]. Reese and Karnovsky, in a now classic paper, demonstrated with electron microscopy (EM) that the endothelium of murine cerebral capillaries constituted the principal component of the structural barrier preventing entry into the brain of circulating horseradish peroxidase (HRP)-a 40,000 Dalton glycoprotein-macromolecule [9]. The two scientists showed the BBB is formed by the cell membranes of endothelial cells which lack the fenestrations found in non-central nervous system (non-CNS) capillary endothelial cells and the tight junctions between adjacent endothelial cells. The BBB has been demonstrated to mostly exclude circulating antibodies and other macromolecules from entry into the CNS [9]. | |
Materials and Methods |
|
| The authors have developed a hypothetical approach to the eradication of tumors which would cause minimal damage to surrounding cells and tissues by using antibody-labelled gold-coated nanoconjugates (NC) with alpha- or beta-emitters. Minimal in this context means only healthy cells near the site of the cancer would be harmed-far fewer than are damaged by chemotherapy or radiation therapy. This approach begins with proof that NC can cross the BBB to reach membranes containing synaptophysin or GFAP filaments. | |
| The next step is to create animal models of brain tumors and to use tumor-specific antigens. Although targeted organic NC composed of carbon, nitrogen, and oxygen have successfully crossed the BBB following intravenous injection of mice, none have been antigenspecific to one organ or tumor tissue. None have produced singleand double-DNA strand breaks in tumor cells. None have provided tumorocidal targeting [10,11]. | |
| Such targeting is being studied extensively. Delivery systems such as bifunctional chelates and nanoparticles combined with targeting agents such as antibodies and peptides make it possible to specifically direct a therapeutic or diagnostic agent to affected cells. Most nanoparticle research has focused on radioactive goldcoated NC which has shown promising results in early clinical trials using 177Lu DOTATATE to treat somatostatin receptor-expressing neuroendocrine tumors and using 223Radium dichloride (Xofigo) to treat metastatic prostate cancer [12-15]. However, precise targeting remains difficult, even with intra-tumoral injections [16]. Recently strategies to fine tune the pharmacokinetics and biodistribution of gold-coated NC in vivo have been developed. Mukherjee et al. demonstrated that the use of a passive targeting agent, polyethylene glycol (PEG), on the surface of the gold-coated NC greatly increased the circulation time of the NC in the blood in vivo. It has also been shown that by using PEG chains of different lengths and with different functional groups, the biodistribution of NC in vivo can be altered [17-21]. These same tactics can be applied to other NC constructs. | |
| Therefore, the preliminary step-as this paper is subtitled-is to provide ultrastructural proof of principle that antibody-labeled, goldcoated NC can cross the BBB and bind to their targeted antigens. This proof of principle supported by concrete evidence does not include an analysis of the mechanism by which the NC crossed the BBB. The authors (PHP, MFM and JDR) have already reported on a similar and successful use of radioactive NC to target antigens in a syngeneic murine lung tumor model using CMT-6 breast cancer cells [22,23]. | |
| Materials | |
| Reagents-obtained from Sigma, Fisher, and others listed-were used unmodified. | |
| NC preparation | |
| Core@shell {La0.5Gd0.5}PO4@4 GdPO4 shell@Au nanoconjugates described above were prepared through the following 25-step process: | |
| a) 50 μL of 0.1 M LaCl3·7 H2O were mixed with 50 μL of 0.1 M GdCl3·6 H2O in a 1 mL V-bottom glass vial. | |
| b) 200 μL of 0.1 M sodium tripolyphosphate (NaTPP) was added and aspirated until clear. | |
| c) The solution was heated and capped at 90oC for three hours. | |
| d) Additional shells of GdPO4 were added by centrifuging the nanoparticles at 3,000g for three minutes. | |
| e) The supernatant was removed and nanoparticles were redispersed in a mixture containing 200 μL of 0.05 M GdCl3, and 400 μL of 0.05 M NaTPP. | |
| f) Nanoparticles were heated and capped for three hours at 90oC as above. | |
| g) Four shells of GdPO4 were added. | |
| h) After the final shell addition, the solution was dialyzed overnight against 18 MΩ water using a 10 kDa molecular weight cutoff regenerated cellulose membrane. | |
| i) Dialyzed particles were collected and placed in a 5 mL V-bottom vial. | |
| j) 300 μL of 0.1 M tribasic sodium citrate was added to the vial along with enough water to bring the total volume to 2.0 mL. The solution was sonicated for 15 minutes using a bath sonicator. | |
| k) 2.5 mL of 1 mM NaAuCl4- was added drop-by-drop at the rate of 1 mL every ten minutes. | |
| l) The solution was allowed to heat for 30-45 minutes following the final addition. | |
| m) After cooling, the gold-coated nanoparticles in the sample were magnetically separated from the gold-coated LnPO4 core nanoparticles using a high field (>0.3 T) NdFeB magnet. Additional characterization of the nanoparticles obtained was presented in a previous report [24]. | |
| n) Electron microscopy (EM) demonstrated the average diameter of the nanoparticles as 101 nm with a Zeta potential -63 mV, Figure 7. This average diameter was significantly smaller than the 250 nm average diameter of nanoparticles in a prior study, which were used to make NC with non-specific antigens that successfully crossed the BBB [11]. | |
| o) Addition of the PEG linker and antibody to the nanoparticlemaking the nanoparticle a nanoconjugate-increased the average hydrodynamic diameter to 1498 nm and the Zeta potential to -28 mV [25]. | |
| p) Anti-synaptophysin or anti-GFAP (glial fibrillary acidic protein) monoclonal antibodies (Dako, Carpinteria, CA) were added to the surface by addition of a lipoamide-dPEG12-COOH linker (Quanta Biodesign, Plain City, Ohio). | |
| q) 12 mg of polyethylene glycol (PEG) linker was added to 3.0 mg of NC solution in 1 mL of water. | |
| r) 36.0 mg of tris (2-carboxyethyl) phosphine was added to cleave the disulfide bridge in the PEG linker. | |
| s) This solution was stirred for four hours, centrifuged to remove the excess PEG, and redispersed in 1 mL of phosphate buffered saline (PBS) (pH=7.4). | |
| t) Peptide-based targeting agents were added via traditional 1-ethyl-3-(3-dimethylaminopropyl) carbodiimide (EDC)/sulfo N-hydroxysuccinimide (sulfo-NHS) chemistry. | |
| u) 80 μL of 10 mg/mL EDC and 8 μL of 10 mg/mL sulfo-NHS were added to a solution of 0.5 mg of NC in 1 mL of PBS and stirred for 30 minutes. | |
| v) Unreacted EDC/sulfo-NHS was removed by centrifugation, and the NC were redispersed in 1 mL of PBS. | |
| w) Anti-synaptophysin or anti-GFAP (0.5 mg) was added and mechanically stirred overnight at room temperature. | |
| x) The reaction was quenched with 3.0 mg of glycine and purified by centrifugation three times, then redispersed in 1 mL of PBS (pH=7.4). | |
| y) NC were analyzed using EM (JEOL 1400, Tokyo, Japan), and UVVisible spectroscopy (Varian Cary 50, Palo Alto, CA). | |
| NC analysis with plasmon resonance | |
| Antibody addition was verified by shifts in the surface plasmon resonance of the gold-coated NC. UV-Visible absorbance was measured before and after addition of the PEG and after the antibody labeling by UV-Visible spectroscopy (Varian Cary 50, Palo Alto, CA). | |
| Verification of antibody binding and retention of antigenbinding specificity | |
| Both the attachment of the antibodies to the nanoparticles and verification they retained their antigen-binding specificity were confirmed with immunohistochemistry. Anti-synaptophysin antibody gold-coated NC and anti-GFAP antibody gold-coated NC were used instead of primary antibodies on paraffin sections of the formalin-fixed murine brain. Localization of the primary antibodies was identified using conventional immunohistochemical techniques described below: | |
| a) 5 μm thick sections mounted on Superfrost Plus glass slides (Fisher Scientific) were dried overnight at 37ºC and then for one hour at 60ºC, prior to deparaffinization through xylene and hydration through graded ethanols. | |
| b) Following incubation with 3% hydrogen peroxide for ten minutes to block endogenous peroxidase activity, the sections were rinsed for five minutes with a Tris-buffered saline solution containing Tween 20 (wash buffer, S3006, DAKO) and then blocked with 1% BSA for 20 minutes. | |
| c) The sections were incubated with the labeled NC suspension as primary antibodies for 60 minutes at room temperature, rinsed, and then incubated with the appropriate secondary universal biotinylated link anti-murine IgG antibody for 30 minutes at room temperature (LSAB Plus System-HRP, K0690, DAKO, Carpinteria, CA). | |
| d) The sections were rinsed twice with the wash buffer for five minutes each, drained, and then incubated for 30 minutes at room temperature using streptavidin conjugated to horseradish peroxidase. (LSAB Plus System-HRP, K0690, DAKO). | |
| e) The slides were rinsed twice in wash buffer for five minutes each before being developed for five minutes using freshly prepared diaminobenzidine tetrahydrochloride solution (DAB Chromagen Substrate, K3468, DAKO) | |
| f) The sections were counterstained with modified Mayer’s Hematoxylin, dehydrated, cleared, and mounted with Permount as a mounting media (SP 15-500, Fisher Scientific). | |
| Intravenous injection of labeled NC into mice | |
| Three groups of mice were used in this experiment. The 45 mice exceeded the number required by ANOVA analysis. | |
| a) Group 1, 24 mice: Received 50 μL (21 μg) of anti-GFAP immunolabeled gold-coated NC (IV). | |
| b) Group 2, 21 mice: Received 50 μL (21 μg) of anti-synaptophysin immunolabeled gold-coated NC (IV). | |
| c) Group 3, Control, 12 mice: Received 50 μL (21 μg) of PEG-coated nanoparticles without antibodies (IV). | |
| The nanoconjugate and nanoparticle solutions were vigorously vortexed immediately prior to intravenous injection to prevent aggregation. Thirty minutes after injection the brain and other organs were harvested. The animals were sacrificed by fresh 2% paraformaldehyde vascular perfusion under terminal anesthesia. Perfusion was used to both fix the tissue and remove any residual intravascular nanoconjugates or nanoparticles. Brains were sliced into coronal sections using a murine Zivic Brain Slicer (Zivic Instruments, Pittsburgh, PA). | |
| Ultrastructural examination | |
| For the ultrastructural study, fresh coronal sections from the brains of the perfused animals were obtained from all three groups and were further fixed by immersion in 2.5% glutaraldehyde/2% paraformaldehyde, cut into 1 mm cubes, and post fixed with 1% osmium tetroxide. After dehydration in a graded series of ethanols, the specimens were cleared with propylene oxide and embedded in Epon (Wako Corporation, Tokyo, Japan). Ultrathin sections (50 nm) were cut with an ultramicrotome (Leica Ultracut UCT, using a DIATOME 45º diamond knife), stained with uranyl acetate, and imaged with a JEOL1400 EM (Tokyo, Japan). Lead citrate stains might have provided better imaging but were not used to preclude the presence of lead salt precipitates that could have been misidentified as gold-coated NC. | |
| Murine protocol | |
| This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. The protocol was approved by the Animal Care and Use Committee of the University of Missouri, Protocol Number 7055. All surgery on BALB/c mice was performed under isoflurane (1.5%) and oxygen mixture anesthesia, and all efforts were made to minimize suffering. | |
Results and Discussion |
|
| NC analysis | |
| The final {La0.5Gd0.5}PO4@4 GdPO4 shell@Au nanoconjugates had (1) metallic diameters of 26.8 nm ± 4.9 nm and (2) hydrodynamic diameters of approximately 1498 nm ± 77 nm-similar or identical to those synthesized by McLaughlin. Four or five antibody molecules were attached to each nanoparticle (McLaughlin, personal communication). The lack of uniformity was related to the functional sites on the PEG linker. | |
| a) Attachment of the PEG linker was confirmed by UV-Visible spectroscopy absorbance. | |
| b) PEG linker and antibody attachment were determined by the shift in the surface plasmon resonance of the gold-coated NC. That shift demonstrated a change in the NC surface environment indicative of antibody attachment. | |
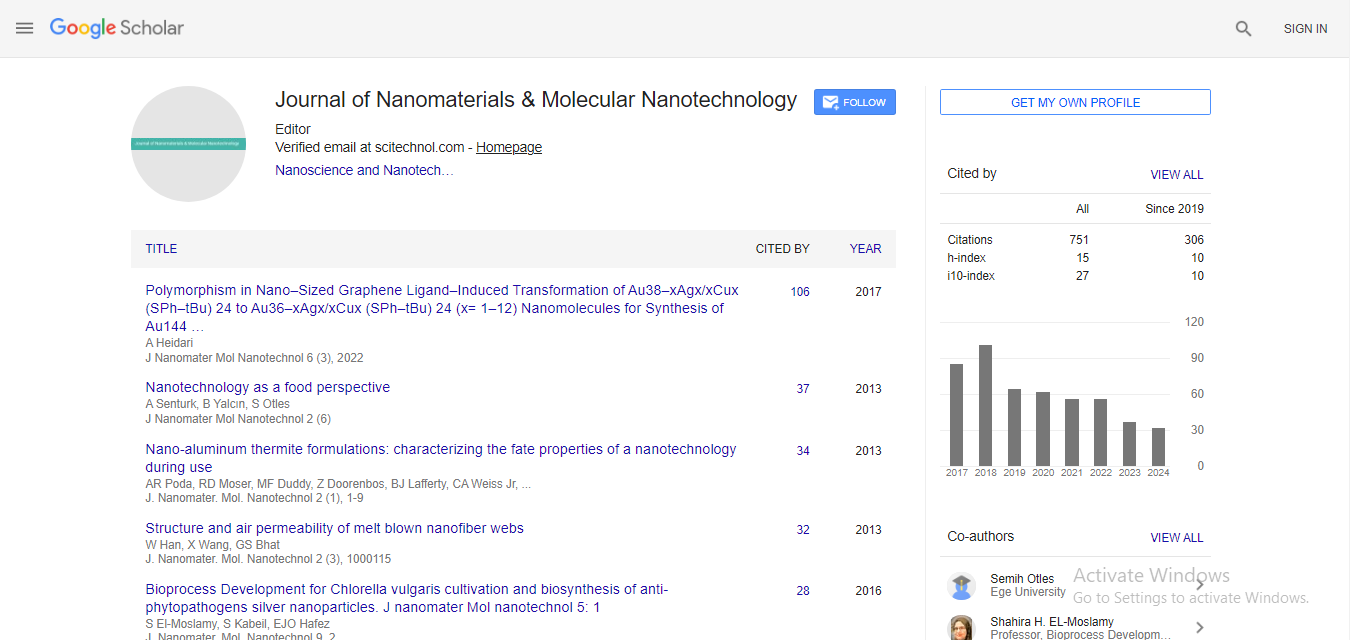
| c) Figures 1 and 2 show the shift in plasmon resonance at key points in the antibody attachment process (before PEG addition and after both PEG and antibody addition). Wavelength shifts identified in the two images prove the aforementioned targeting process was successful. | |
| Figure 1: Plasmon Resonance Shift during Anti-GFAP Addition. | |
| Figure 2: Plasmon Resonance Shift during Anti-synaptophysin Addition. | |
| Use of NC as primary antibodies | |
| As outlined above, gold-coated NC labelled with antisynaptophysin or anti-GFAP antibodies were used as primary antibodies for immunohistochemistry of normal murine brain paraffin sections. The resulting immunostain patterns were identical to those seen in a normal murine brain, thus, confirming the persistent immunogenicity of the targeting antibodies. | |
| a) Figure 3 shows the diffuse finely granular brown staining of the cortical neuropil typical of synaptophysin immunohistochemical staining of gray matter, produced using gold-coated NC with anti-synaptophysin antibodies conjugated to their surfaces. As expected, there was no staining in the white matter [26]. | |
| Figure 3: The diffuse finely granular brown staining of the cortical neuropil typical of synaptophysin immunohistochemical staining of gray matter, produced using gold-coated NC with anti-synaptophysin antibodies conjugated to their surfaces | |
| b) Figure 4 shows positive staining of the astrocytes. As expected, there was no staining of the, neurons, oligodendrocytes, or other non-astrocytic cells [22,26]. | |
| Figure 4: Positive staining of the astrocytes | |
| Ultrastructural localization of injected labeled NC | |
| Although time-consuming and labor-intensive, EM provided the best method to reveal the presence of gold-coated NC in tissue-in this case, brain tissue. As stated above, lead citrate stains might have provided better imaging, but they were not used to preclude the presence of lead salt precipitates that could be misidentified as gold-coated NC. The EM evidence was conclusive, namely, that gold-coated NC were found in all murine brains, except those of the control group. As expected, (1) no ultrastructural evidence of cellular toxicity or apoptosis in any cells in the examined brain sections from any of the three groups was found; (2) mitochondria and other organelles, as well as myelin sheaths, were intact; and (3) no change was seen in the brain capillary endothelial tight junctions. Group-specific results are listed below: | |
| a) Group 1: Anti-GFAP-labeled gold-coated NC were sometimes trapped in spaces between axons and the inner lamellae of myelin sheaths (not illustrated) and were also localized in the cytoplasm of astroglial cells, specifically, those close to some of the intermediate filaments, as shown in Figure 5A-C. It is unclear what mechanism caused this phenomenon, but again the EM evidence is difficult to dispute. | |
| Figure 5: Anti-GFAP-labeled gold-coated NC were sometimes trapped in spaces between axons and the inner lamellae of myelin sheaths (not illustrated) and were also localized in the cytoplasm of astroglial cells, specifically, those close to some of the intermediate filaments. | |
| b) Group 2: Anti-synaptophysin-labeled gold-coated NC were localized exclusively in the synapses, on the synaptic vesicles, or on membranes of the presynaptic processes, as shown in Figure 6A-E. | |
| Figure 6: Anti-synaptophysin-labeled gold-coated NC were localized exclusively in the synapses, on the synaptic vesicles, or on membranes of the presynaptic processes | |
| Figure 7: Electron microscopy (EM) demonstrated the average diameter of the nanoparticles as 101 nm with a Zeta potential -63 mV | |
| c) Group 3, Control: No PEG-coated nanoparticles without antibodies were found in any of the examined brain tissue sections. One control group was deemed sufficient because the chosen antibodies were well characterized and routinely used in clinical and experimental laboratories. | |
Discussion |
|
| The goal of this proof-of-concept study was to show that antibody-labeled, gold-coated NC administered intravenously in a murine model could cross the BBB, retain their antigen-specific binding, and actively target either synaptophysin or GFAP. The ultrastructural evidence constitutes scientifically sound proof that a small proportion of the injected gold-coated NC crossed the BBB and, for the most part, found the appropriate targets. | |
| a) UV-Visible spectroscopy results demonstrate successful labeling of the gold-coated NC with both anti-synaptophysin and anti- GFAP antibodies. | |
| b) Spectral wavelength changes in the plasmon resonance peak of the gold-coated NC indicated both PEG linker and antibody attachment. A small but measurable wavelength change-532- 541nm and 523-537nm-was demonstrated (Figures 1 and 2). | |
| Retention of antigen specificity of the antibody-coated goldcoated NC was confirmed by appropriate immunohistochemical staining of the gray matter neuropil (synaptophysin) or of astrocytes and their processes (GFAP) in brain tissue sections after incubation with the anti-synaptophysin or anti-GFAP labeled gold-coated NC. | |
| Immunohistochemical studies, using the antibody-labeled gold-coated NC used in vivo, confirmed the persistent antigenicity of the targeting antibodies. EM images demonstrated that a portion of the anti-synaptophysin- labeled gold-coated NC crossed the BBB, traversed the interstitial space, and attached to the neuronal synapses-the site of synaptophysin. Similarly, EM images showed that a portion of the anti-GFAP-labeled gold-coated NC crossed the BBB, traversed the interstitial space, passed through the astrocyte plasma membrane, and attached near the intermediate filaments of the glial cells-the site of GFAP. These findings are neither artifactual nor were they present in the control animal samples. Since gold-coated NC were nearly invisible at even a magnification of 1500, the EM imaging performed could not provide an overview of NC tissue distribution. That being said, it bears repeating that the EM imaging found synaptophysin goldcoated NC only on synaptic structures and GFAP gold-coated NC only in astrocytes with filaments and between the axon plasma membranes and myelin membranes. | |
| The targeted anti-synaptophysin and anti-GFAP gold-coated NC reached specific targets in the brain parenchyma without any added chaperones, demonstrating proof of concept that site-specific, receptor-mediated uptake of inorganic gold-coated NC is possible in the CNS and can be applied to specific brain proteins and probably to other (tumor) proteins as well. | |
| Further studies are in process to refine the targeting mechanism and to increase the tumorocidal effect of gold-coated NC. These studies include (1) determination of safe and effective tumorocidal gold-coated NC dosages, (2) pretreatment with intravenous injection of clodronate liposomes to increase gold-coated NC circulation time by temporarily blocking the macrophages in the reticuloendothelial system, (3) improvement of gold-coated NC penetration via electroporation, which enhances the permeability of the cerebral endothelium [25,27-29], and (4) determination of the percentage of tumorocidal gold-coated NC that cross the BBB. Further study is also required to find evidence of antibody-labeled gold-coated NC in the brain capillary endothelium. | |
| Ultrastructural imaging proved that injected anti-synaptophysin and anti-GFAP targeted gold-coated NC successfully crossed the BBB in Balb/c mice and became bound to synaptophysin in the synapses and to GFAP in the intermediate filaments of the astroglial cells. While additional studies are required, the use of antibody-labeled, gold-coated radionuclide NC may become the basis for treatment of a variety of metastases and tumors, including malignant brain tumors such as glioblastoma. | |
Acknowledgments |
|
| Research supported in part under a DOE Nuclear Energy University Program Graduate Fellowship (DE-FOA-0000807). | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi