Research Article, J Spine Neurosurg Vol: 12 Issue: 4
Comparison of 2-Year Postoperative Clinical Outcomes between Transforaminal and Lateral Transpsoas Lumbar Interbody Fusion in the Treatment of Degenerative Spondylolisthesis at L4-5
Frank M Phillips1*, Bryce A Basques1, Grant D Shifflett1, Kaveh Khajavi2, Adam S Kanter3and Mark D Peterson4
1Department of Orthopaedic Surgery, Rush University Medical Center, Chicago, United States
2Department of Orthopaedic Surgery, Georgia Spine and Neurosurgery Center, Atlanta, United States
3Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, United States
4Department of Neurological Surgery, Asante Spine Care, Oregon, United States
- *Corresponding Author:
- Frank M Phillips
Department of Orthopaedic Surgery,
Rush University Medical Center,
Chicago,
United States;
E-mail: Frank.Phillips@rushortho.com
Received date: 08 January, 2020, Manuscript No. JSNS-23-6224;
Editor assigned date: 13 January, 2020, PreQC No. JSNS-23-6224 (PQ);
Reviewed date: 27 January, 2020, QC No. JSNS-23-6224;
Revised date: 14 June, 2023, Manuscript No. JSNS-23-6224 (R);
Published date: 12 July, 2023, DOI: 10.4172/2325-9701.1000160
Citation: Phillips FM, Basques BA, Shifflett GD, Khajavi K, Kanter AS, et al. (2023) Comparison of 2-Year Postoperative Clinical Outcomes between Transforaminal and Lateral Transpsoas Lumbar Interbody Fusion in the Treatment of Degenerative Spondylolisthesis at L4-5. J Spine Neurosurg 12:3.
Abstract
Background: Lumbar interbody fusion has been shown to be effective in the treatment of degenerative spondylolisthesis, though a variety of surgical techniques exist and there are few direct comparisons between homogenous patient samples in the literature to guide evidence-based decision making. This is a retrospective review of prospectively collected data from a multi-center, patient outcomes registry. The purpose of this study is to compare perioperative and two-year postoperative clinical outcomes between patients treated with either lateral Lumbar Interbody Fusion (LLIF) using real-time, directional neuromonitoring or Transforaminal Lumbar Interbody Fusion (TLIF) for isolated degenerative spondylolisthesis at L4-5. Methods: A total of 72 patients (47 LLIF, 25 TLIF) who underwent single-level interbody fusion at L4-5 for degenerative spondylolisthesis with a minimum of two year postoperative clinical outcomes were included in the analysis. Results: The baseline characteristics were similar across the groups (all, p>0.05). Postoperative length of hospital stay was similar between groups (p>0.05), however, operative time was lower in the LLIF group compared to the TLIF group (119.2 minutes vs. 149.7 minutes, respectively; p=0.053). Complications were more frequent in the TLIF group compared to the LLIF group (p=0.057), with a notable absence of neurological injuries in both groups. MCID thresholds were met in 74%, 84% and 72% of LLIF patients and 72%, 63% and 75% of TLIF patients for Oswestry Disability Index (ODI), lower back pain and worst-leg pain, respectively. Similarly, Substantial Clinical Benefit (SCB) was met in 76% to 84% of LLIF patients and 67% to 81% of TLIF patients (all p>0.05). Conclusion: In the treatment of degenerative spondylolisthesis at L4-5, both LLIF, with real-time neural monitoring and TLIF resulted in substantial clinical improvements that were maintained through two years postoperative, though with more complications and generally depressed clinical outcomes in the TLIF group compared to the LLIF group
Keywords: Spondylolisthesis, Outcome differences, Registry, Patients
Introduction
Degenerative spondylolisthesis of the lumbar spine most commonly occurs at L4-5 and there are a variety of open and minimally invasive surgical techniques for the treatment of this condition at this level. The goals of surgery in these patients typically include neural decompression, restoration of sagittal alignment (correction of the spondylolisthesis and restoration of spinopelvic harmony), stabilization and fusion. Numerous studies have confirmed the clinical and cost effectiveness of spinal fusion in treating spondylolisthesis as well as the incremental benefits of instrumented surgery over nonoperative therapies in these patients at both early and long-term time points [1].
A variety of surgical approaches for spinal fusion can be used to treat spondylolisthesis, including Anterior Lumbar Interbody Fusion (ALIF), Posterior Lumbar Interbody Fusion (PLIF), Transforaminal Lumbar Interbody Fusion (TLIF), Lateral Lumbar Interbody Fusion (LLIF) and Posterolateral Fusion (PLF). Two approaches that have been more recently developed and adopted for this indication over the past 15 years are LLIF and TLIF. LLIF was introduced in the literature in 2006 as eXtreme Lateral Interbody Fusion (XLIF) and has been increasingly used as the approach avoids much of the morbidity associated with traditional anterior and posterior approaches with many of the benefits of Anterior Lumbar Interbody Fusion (ALIF). LLIF may also avoid the requirement for direct neural manipulation by achieving indirect decompression via disc space distraction with wide-footprint implant placement and realignment of the segment through ligamentotaxis [2].
Transforaminal Lumbar Interbody Fusion (TLIF) is one of the most common approaches for interbody fusion, utilizing an off-midline posterior approach for facet removal and access to the disc through the intervertebral foramen. The TLIF procedure offers a direct decompression of neural structures and placement of posterior instrumentation for spinal realignment without repositioning the patient. The approach can also be performed using minimally invasive or traditional open surgical exposures.
Recently, reports have shown that LLIF and TLIF may both be effective at treating lumbar degenerative spondylolisthesis despite different mechanisms of action (indirect versus direct decompression). However, studies on comparative differences between LLIF and TLIF remain few. The aim of this investigation, therefore, was to compare the safety and efficacy of LLIF and TLIF in patients treated at L4-5 for degenerative spondylolisthesis.
Materials and Methods
Study design
A retrospective review was performed from the SpineTRACK registry, a comprehensive, prospective, long-term, multi-center patient outcomes registry. The SpineTRACK registry is built on a web based and electronic Data Capture (eDC) system and consists of both cervical and thoracolumbar study groups as well as degenerative, traumatic and deformity. Patients treated conservatively or surgically via any procedure are eligible for inclusion in the registry, though only patients treated surgically and who met inclusion criteria, listed below, were considered for this study [3].
Data collection
Variables in the SpineTRACK registry used in this analysis included baseline demographic, pathology, treatment, complication, reoperation, clinical outcome and satisfaction information. Baseline patient information included age, gender, Body Mass Index (BMI), tobacco use and comorbidities. Treatment characteristics included Estimated Blood Loss (EBL), Operative Time (ORT) and postoperative Length of hospital Stay (LOS). Complications were recorded at all time points and were classified according to a fivepoint severity scale (Table 1) [4].
| Complication level | Complication description |
|---|---|
| Level 1 | Required minor invasive (e.g., Foley catheter, NG tube) or simple treatment but with no long-term effect |
| Level 2 | Required invasive (e.g., surgery) or complex treatment (e.g., monitored bed) and is most likely to have a temporary (<6 months) adverse effect on outcome |
| Level 3 | Required invasive (e.g., surgery) or complex treatment (e.g., monitored bed) and is most likely to have a prolonged (>6 months) adverse effect on outcome |
| Level 4 | Significant neural injury (i.e., one or more grade deterioration in ASIA grade) or serious life or limb‑threatening event (i.e., sentinel event) |
| Level 5 | Resulting in death |
Note: NG=Nasogastric; ASIA=American Spinal Injury Association; Sentinel event=A sentinel event is an unexpected serious life or limb-threatening event that necessitates investigation and review to determine the root cause
Table 1: Five-point complication scale used in the SpineTRACK registry.
Patient Reported Outcomes (PROs) were collected preoperatively and at six week, three-month, six-month, 12-month and 24-month postoperative intervals. PROs included disability (Oswestry Disability Index (ODI)) and lower back and worst-leg pain (10 point Numeric Rating Scale (NRS)). Thresholds for Minimum Clinically Important Difference (MCID) and Substantial Clinical Benefit (SCB) were calculated for each patient across ODI, lower back pain and worst-leg pain thresholds [5].
Patient samples
Patients were selected for the study based on the following inclusion criteria: Patients were at least 18 years of age, had degenerative spondylolisthesis with resultant stenosis and neurogenic symptoms consistent with the pathology at L4-5, were treated with either eXtreme Lateral Interbody Fusion (XLIF® (LLIF), NuVasive, Inc.) or Transforaminal Lumbar Interbody Fusion (TLIF) at L4-5 only and had evaluable data at baseline and at least one two-year postoperative follow up measure [6].
Surgical technique-LLIF
The surgical technique for LLIF (XLIF) has been previously described. In summary, the procedure utilizes blunt dissection through a 90° off-midline (lateral), retroperitoneal, transpsoas approach to the lateral disc space. Development of and passage through the retroperitoneal space and psoas muscle requires understanding of relevant neural and visceral structures and use of neuromonitoring integrated into approach and procedural instrumentation. Once the disc space has been accessed, standard surgical techniques for discectomy and interbody fusion are used with placement of a large intervertebral spacer with the goal of indirectly decompressing the neural elements and realignment of the segment through ligamentotaxis, as the Anterior and Posterior Longitudinal Ligaments (A/PLL) remain intact. Supplemental fixation is applied at the surgeon’s discretion [7].
Surgical technique-TLIF
The technique for TLIF has been previously described.
Statistical analysis
Statistical analysis was performed using SAS v9.4. Patient demographics (age, gender, body mass index and tobacco use) and operative characteristics (EBL, ORT and LOS) were compared between treatment groups (LLIF and TLIF) using general linear modeling and chi-square/Fisher’s exact tests. General linear modeling was used to compare outcomes at the 24-month postoperative time point to the preoperative time point across groups. Significant p-values were examined with Scheffe’s post hoc test for significance at the p<0.05 level. The rates of postoperative complications and satisfaction were compared among groups using chi-square/Fisher’s exact tests. Statistical significance was defined at p<0.05 [8].
Results
Patient demographics and operative data
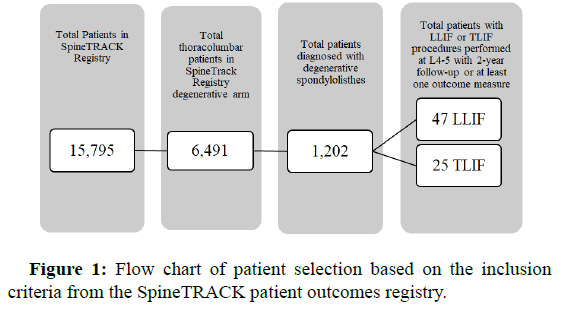
Out of 15,795 patients in the SpineTRACK registry, 72 patients (47 LLIF, 25 TLIF) met all inclusion criteria (Figure 1). Of the 72 patients enrolled in the study, 46 (63.89%) patients were female, the mean age was 67 years (range: 44 to 85 years) and the mean Body Mass Index (BMI) was 30.83 kg/m2 (range: 19.20 to 46.20 kg/m2). Patients had a mean Charlson comorbidity index score of 2.61 (range: 0 to 5). The most common baseline comorbidities included hypertension (50% of patients), osteoarthritis (26.39% of patients) and diabetes mellitus (20.83% of patients). Seventeen (23.61%) patients had prior spine surgery. All patients were diagnosed with grade I or grade II degenerative spondylolisthesis at L4-5. The mean baseline characteristics were similar between LLIF and TLIF groups (all, p>0.05). Patient baseline characteristics are included in Table 2 [9].
| Characteristic | LLIF N=47 | TLIF N=25 | p-value |
|---|---|---|---|
| Demographics | |||
| Mean age in years (stdev) | 67.16 (8.36) | 66.84 (9.49) | 0.886 |
| Female (%) | 31 (65.96) | 15 (60.00) | 0.618 |
| BMI (kg/m2) (stdev) | 31.58 (6.83) | 29.69 (7.49) | 0.305 |
| Tobacco use (%) | 7 (14.89) | 3 (12.00) | 1 |
| Mean Charlson comorbidity score (stdev) | 2.68 (1.20) | 2.45 (0.96) | 0.442 |
| Comorbidities | |||
| Hypertension (%) | 22 (46.81) | 14 (56.00) | 0.458 |
| Osteoarthritis (%) | 15 (31.91) | 4 (16.00) | 0.171 |
| Diabetes mellitus (%) | 13 (27.66) | 2 (8.00) | 0.069 |
| Asthma (%) | 8 (17.02) | 3 (12.00) | 0.737 |
| Depression (%) | 4 (8.51) | 5 (20.00) | 0.26 |
| Chronic pulmonary disease (%) | 4 (8.51) | 2 (8.00) | 1 |
| Osteoporosis (%) | 4 (8.51) | 0 (0.00) | 0.291 |
| Nervous system disorder (%) | 2 (4.26) | 0 (0.00) | 0.54 |
| Anemia (%) | 1 (2.13) | 0 (0.00) | 1 |
| Cerebrovascular disease (%) | 1 (2.13) | 0 (0.00) | 1 |
| Renal disease (%) | 1 (2.13) | 0 (0.00) | 1 |
| Malignant solid tumor (%) | 1 (2.13) | 0 (0.00) | 1 |
| Myocardial infarction (%) | 1 (2.13) | 0 (0.00) | 1 |
| Any prior lumbar spine surgery? | |||
| Yes (%) | 12 (25.53) | 5 (20.00) | 0.851 |
| No (%) | 34 (72.34) | 20 (80.00) | |
| Unknown (%) | 1 (2.13) | 0 (0.00) | |
| Diagnoses | |||
| Grade I degenerative (%) | 26 (55.32) | 13 (52.00) | 0.788 |
| Grade II degenerative (%) | 5 (10.64) | 2 (8.00) | 1 |
| Unspecified (%) | 16 (34.04) | 10 (40.00) | - |
| Presentation | |||
| Lower back pain (%) | 45 (95.74) | 25 (100.00) | 0.54 |
| Leg pain (%) | 43 (91.49) | 19 (76.00) | 0.086 |
Note: N=Number of patients; LLIF=Lateral Lumbar Interbody Fusion; TLIF=Transforaminal Lumbar Interbody Fusion; stdev=Standard deviation; BMI=Body Mass Index
Table 2: Demographics.
Bilateral pedicle screw was performed in 70% of LLIF and 72% of TLIF patients, with unilateral pedicle screws used in 6% of LLIF patients and 4% of TLIF patients. In the remaining patients laterality of pedicle screws were not specified [10].
Perioperative results
The mean blood loss for the TLIF group was significantly higher than the LLIF group (180.0 mL versus 56.6 mL, respectively; p<0.005). Postoperative length of hospital stay was similar between groups (p>0.05), however, operative time was lower in the LLIF group compared to the TLIF group (119.2 minutes versus 149.7 minutes, respectively; p=0.053). No patient was reported to receive any supplemental blood products. Discharge location was available for most patients and a majority of those patients were discharged home. Detailed perioperative characteristics are included in Table 3 [11].
| Characteristic | LLIF N=47 | TLIF N=25 | p-value |
|---|---|---|---|
| Perioperative characteristics | |||
| n | 39 | 19 | 0.053 |
| Mean ORT (mins) (stdev) | 119.21 (56.21) | 149.68 (52.39) | |
| n | 40 | 25 | 0.002 |
| Mean EBL (mL) (stdev) | 56.63 (60.83) | 180.00 (174.09) | |
| n | 27 | 18 | 0.07 |
| Mean LOS (days) (stdev) | 1.22 (1.49) | 1.36 (0.90) | |
| Discharge location | |||
| n | 41 | 24 | 0.302 |
| Home (%) | 34 (82.93) | 23 (95.83) | |
| Skilled nursing (%) | 1 (2.44) | 0 (0.00) | |
| Unknown (%) | 6 (14.63) | 1 (4.17) | |
Note: N=Number of patients; n=Number of patients in each group; LLIF=Lateral Lumbar Interbody Fusion; TLIF=Transforaminal Lumbar Interbody Fusion; ORT=Operating Room Time; mins=Minutes, stdev=Standard Deviation; EBL=Estimated Blood Loss; LOS=Length of Stay
Table 3: Treatment information.
Clinical results
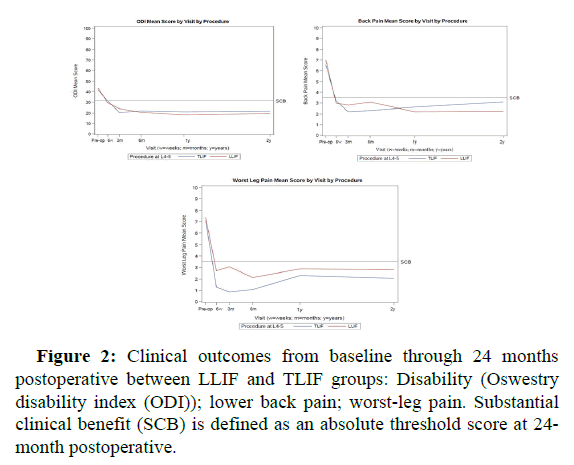
Preoperative clinical measures were similar among all groups (all p>0.05). At 24 months postoperative, improvements from preoperative were also similar among groups, though slightly greater improvements were seen in the LLIF group compared to the TLIF group across disability and lower back pain measures. Complete clinical outcomes are shown in Figure 2 and Table 4 [12].
| Characteristic | LLIF N=47 | TLIF N=25 | p-value |
|---|---|---|---|
| Disability (ODI)-mean | |||
| Pre-op (n) | 43.36 (47) | 41.52 (25) | 0.633 |
| 2-year post-op (n) | 19.53 (47) | 21.68 (25) | 0.673 |
| 2-year post-op change (%) (n) | 59.23 (47) | 51.69 (25) | 0.432 |
| Lower back pain (NRS)-mean | |||
| Pre-op (n) | 7.02 (45) | 6.56 (25) | 0.378 |
| 2-year post-op (n) | 2.24 (46) | 3.08 (24) | 0.273 |
| 2-year post-op change (%) (n) | 68.54 (44) | 58.38 (24) | 0.309 |
| Worst-leg pain (NRS)-mean | |||
| Pre-op (n) | 7.40 (25) | 7.13 (16) | 0.723 |
| 2-year post-op (n) | 2.80 (25) | 2.06 (16) | 0.505 |
| 2-year post-op change (%) (n) | 67.04 (25) | 67.53 (16) | 0.972 |
Note: N=Number of patients; n=Number of patients in each group; LLIF=Lateral Lumbar Interbody Fusion; TLIF=Transforaminal Lumbar Interbody Fusion; ODI=Oswestry Disability Index; NRS=Numeric Rating Scale
Table 4: Preoperative to 2-year postoperative clinical outcomes.
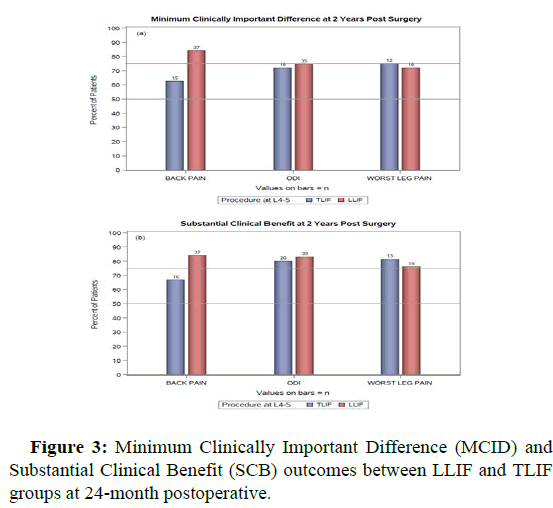
MCID thresholds were met in 74%, 84% and 72% of LLIF patients and 72%, 63% and 75% of TLIF patients for ODI, lower back pain and worst-leg pain, respectively. The proportion of patients reaching MCID was significantly higher in the LLIF group for back pain (p<0.05). Similarly, SCB was met in 76% to 84% of LLIF patients and 67% to 81% of TLIF patients (all p>0.05). MCID and SCB details are included in Figure 3 and Table 5 [13].
| Characteristic | LLIF N=47 | TLIF N=25 | p-value |
|---|---|---|---|
| MCID (%) | |||
| Disability-ODI (n) | 74.47 (47) | 72.00 (25) | 0.821 |
| Back pain-NRS (n) | 84.09 (44) | 62.50 (24) | 0.045 |
| Worst-leg pain-NRS (n) | 72.00 (25) | 75.00 (16) | 1 |
| SCB (%) | |||
| Disability-ODI (n) | 82.98 (47) | 80.00 (25) | 0.757 |
| Back pain-NRS (n) | 84.09 (44) | 66.67 (24) | 0.098 |
| Worst-leg pain-NRS (n) | 76.00 (25) | 81.25 (16) | 1 |
Note: N=Number of patients; n=Number of patients in each group; LLIF=Lateral Lumbar Interbody Fusion; TLIF=Transforaminal Lumbar Interbody Fusion; MCID=Minimum Clinically Important Difference; ODI=Oswestry Disability Index; NRS=Numeric Rating Scale; SCB=Substantial Clinical Benefit
Table 5: Minimum Clinically Important Difference (MCID) and Substantial Clinical Benefit (SCB) results at 2-year postoperative.
Complications
Complications were more frequent in the TLIF group compared to the LLIF group (p=0.057). Out of nine reported complications, six complications were graded as level 3 or lower (Table 1). Of the spine specific complications, there was one dural tear and one wound infection in the TLIF group. Specifically, there were no cases of motor deficit in either group. A list of complications and classification level are included in Table 6.
| Complications | LLIF N=47 | TLIF N=25 |
|---|---|---|
| Surgical complications (%) | 0 (0.00) | 1 (4.00) |
| Dural tear (level 1) | 0 | 1 |
| Postoperative complications (%) | 3 (6.38) | 5 (20.00) |
| Bowel obstruction (level 2) | 0 | 1 |
| Hardware failure (level 1) | 0 | 1 |
| Meniscus tear right knee (level not reported) | 1 | 0 |
| Left total knee arthroplasty (level 3) | 0 | 1 |
| Scoliosis above fusion (level not reported) | 1 | 0 |
| Superficial wound infection (level 1) | 0 | 1 |
| Urinary incontinence (level not reported) | 1 | 0 |
| Urinary tract infection (level 2) | 0 | 1 |
Note: N=Number of patients; LLIF=Lateral Lumbar Interbody Fusion; TLIF=Transforaminal Lumbar Interbody Fusion
Table 6: Perioperative and postoperative complications and classification level.
Discussion
Spinal decompression and fusion in the treatment of degenerative spondylolisthesis has been consistently shown to have significant clinical- and cost-effectiveness over non-operative therapies. One challenge in the surgical decision making around this common pathology is the choice of approach and procedure, as spondylolisthesis can be treated by ALIF, LLIF, TLIF, PLIF, PLF, nonfusion devices or simple decompressions in certain instances [14].
The lateral interbody approach allows for placement of a large intervertebral spacer and maintenance of the Anterior Longitudinal Ligament (ALL) and Posterior Longitudinal Ligament (PLL), which allows for segmental realignment through ligamentotaxis. However, the main risk during the lateral transpsoas approach is injury to the lumbar plexus. In patients with spondylolisthesis at L4-5, targeting of the lateral disc space is further challenged, as the plexus tends to migrate anteriorly along with the translational deformity. Thus, advanced neuromonitoring integrated into approach and procedural instrumentation is considered to be a key part of the surgical technique in order to identify and avoid motor neural structures.
Posterior approaches rely on instrumentation for spinal realignment and fusion as well as direct decompression of neural structures. Many of the major complications of anterior approaches are avoided in posterior approaches, though with the introduction of, in particular, paraspinal muscle and ligamentous disruption, nerve root injury, dural complications and elevated risk of postoperative infection [15].
While there are some studies that have evaluated the outcomes of LLIF in the treatment of degenerative spondylolisthesis, comparative studies of LLIF versus other common techniques remain few and therefore provide limited guidance for evidence-based medical decision making. Khajavi et al., reported on 60 patients treated with XLIF at varied lumbar levels with supplemental fixation (in 95% of patients) for low-grade degenerative spondylolisthesis. ORT, EBL and LOS were 206 minutes, 83 mL and 1.3 days, respectively. Complications were observed in 5% of patients, with one mild ankle dorsiflexion weakness as the only motor neural complication. Hip flexion weakness occurred in 3% of cases and new postoperative anterior thigh sensory changes were seen in 5% of cases, all of which resolved without intervention. At an average of 20 months postoperative, ODI, lower back pain, worst-leg pain, PCS and MCS improved 51%, 71%, 65%, 40% and 19% respectively, with 95% of patients reporting satisfaction with their outcome and 90% willingness to redo their operation.
TLIF in the treatment of degenerative spondylolisthesis has been similarly studied with good clinical outcomes reported. A large-scale, systematic literature review of MIS and open TLIF by Goldstein et al., of which spondylolisthesis was a common indication, showed broad clinical improvements in both cohorts.
Sembrano et al., performed a prospective, multi-center study to test the ability of LLIF and TLIF to treat degenerative spondylolisthesis. The authors reviewed two-year outcomes for 29 LLIF and 26 MIS TLIF patients and found comparable perioperative outcomes. Hip flexion weakness was common in the LLIF patients (31%), a known side effect of surgery and was absent in the MIS TLIF cohort. New lower extremity weakness was evident in one LLIF patient and no MIS TLIF patients. New postoperative sensory changes were seen in three LLIF and two MIS TLIF patients, all of which resolved by 12 months postoperative. Greater back pain improvement was seen in the LLIF group compared to TLIF group (73% and 64%, respectively), with similar improvements in leg pain and ODI between two groups. In contraindication to the current study, Sembrano study was not limited to spondylolisthesis at the L4-5 level.
In the current study, complications were greater in the TLIF groups compared to LLIF group with a notable absence of neurological injuries in both groups. This finding is consistent with other studies of LLIF and are in contrast to alternative techniques for LLIF that do not use systematic neuromonitoring and which have consistently higher reported neural injury rates. The theoretical risk to the lumbar plexus, even in these higher-risk pathologies with grade I and grade II spondylolisthesis (where the deformity decreases the working window of the approach), has been repeatedly shown to continue to be low and largely avoided when these advanced neuromonitoring techniques are employed.
The clinical outcomes for both procedures showed significant improvements in all clinical parameters from baseline to 24 months postoperative. Lower back pain was improved 68% in LLIF and 58%in TLIF groups (p=0.309) with a similar improvement seen in worst-leg pain for both groups (67%). Disability improved 59% in LLIF and 52% in TLIF patients (p=0.432). The study may have been underpowered to detect subtle differences in outcomes between the procedures.
Limitations of the current study include relatively small sample sizes, which limit statistical power to detect more nuanced differences between treatment cohorts. Also, while the use of the registry data allow for a broader sample of patients from the real-life practices of surgeons in different geographies, the lack of a formal protocol can have a negative impact on data collection.
Conclusion
These data support that both LLIF and TLIF in the treatment of degenerative spondylolisthesis at L4-5 resulted in clinical improvements that were maintained through two years postoperative with similar clinical benefits and maintenance of outcome. While perioperative and long-term complications were higher in the TLIF compared to LLIF group, both groups experienced few major complications. These data also did not show elevated neural complication rates in LLIF patients treated at L4-5 for degenerative spondylolisthesis.
Acknowledgement
The authors would like to acknowledge Kyle Malone, MS, Linda Sullivan, PhD, Fatemeh Nooshabadi, PhD and Sarika Reed, MS, at NuVasive for their statistical and editorial assistance.
Disclosure
No funds were received in support of this work. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
References
- Jacobsen S, Sonne-Holm S, Rovsing H, Monrad H, Gebuhr P (2007) Degenerative lumbar spondylolisthesis: An epidemiological perspective: The copenhagen osteoarthritis study. Spine 32: 120-125.
[Crossref] [Google Scholar] [PubMed]
- Ahmadian A, Verma S, Mundis GM, Oskouian RJ, Smith DA, et al. (2013) Minimally invasive lateral retroperitoneal transpsoas interbody fusion for L4-5 spondylolisthesis: Clinical outcomes presented at the 2013 spine section meeting. J Neurosurg Spine 19: 314-320.
[Crossref] [Google Scholar] [PubMed]
- Khajavi K, Shen A, Hutchison A (2015) Substantial clinical benefit of minimally invasive lateral interbody fusion for degenerative spondylolisthesis. Eur Spine J 24: 314-321.
[Crossref] [Google Scholar] [PubMed]
- Lombardi JS, Wiltse LL, Reynolds J, Widell EH, Spencer CU (1985) Treatment of degenerative spondylolisthesis. Spine 10: 821-827.
[Crossref] [Google Scholar] [PubMed]
- Mardjetko SM, Connolly PJ, Shott S (1994) Degenerative lumbar spondylolisthesis: A meta-analysis of literature 1970-1993. Spine 19: 2256S-2265S.
[Google Scholar] [PubMed]
- Rothenfluh DA, Mueller DA, Rothenfluh E, Min K (2015) Pelvic incidence-lumbar lordosis mismatch predisposes to adjacent segment disease after lumbar spinal fusion. Eur Spine J 24: 1251-1258.
[Crossref] [Google Scholar] [PubMed]
- Adogwa O, Parker SL, Davis BJ, Aaronson O, Devin C, et al. (2015) Cost-effectiveness of transforaminal lumbar interbody fusion for grade I degenerative spondylolisthesis. J Neurosurg Spine 15: 138-143.
[Crossref] [Google Scholar] [PubMed]
- Rihn JA, Hilibrand AS, Zhao W, Lurie JD, Vaccaro AR, et al. (2015) Effectiveness of surgery for lumbar stenosis and degenerative spondylolisthesis in the octogenarian population: Analysis of the Spine Patient Outcomes Research Trial (SPORT) data. J Bone Joint Surg 97: 177.
[Crossref] [Google Scholar] [PubMed]
- Goldstein CL, Phillips FM, Rampersaud YR (2016) Comparative effectiveness and economic evaluations of open versus minimally invasive posterior or transforaminal lumbar interbody fusion. Spine 41: S74-S89.
[Crossref] [Google Scholar] [PubMed]
- Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, et al. (2007) Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. New Eng J Med 356: 2257-2270.
[Crossref] [Google Scholar] [PubMed]
- Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, et al. (2009) Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: Four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg 91: 1295.
[Crossref] [Google Scholar] [PubMed]
- Tosteson AN, Tosteson TD, Lurie JD, Abdu W, Herkowitz H, et al. (2011) Comparative effectiveness evidence from the spine patient outcomes research trial: Surgical vs. non-operative care for spinal stenosis, degenerative spondylolisthesis and intervertebral disc herniation. Spine 36: 2061.
[Crossref] [Google Scholar] [PubMed]
- Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme Lateral Interbody Fusion (XLIF): A novel surgical technique for anterior lumbar interbody fusion. Spine J 6: 435-443.
[Crossref] [Google Scholar] [PubMed]
- Elowitz EH, Yanni DS, Chwajol M, Starke RM, Perin NI (2011) Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: Radiographic and outcome analysis. Min Invas Neurosurg 54: 201-206.
[Crossref] [Google Scholar] [PubMed]
- Kepler CK, Sharma AK, Huang RC, Meredith DS, Girardi FP, et al. (2012) Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine 16: 329-333.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi