Research Article, J Spine Neurosurg Vol: 12 Issue: 6
Clinico-Radiological Profile of Spine Injury at Dayanand Medical College and Hospital
Swarjith Nimmakayala*, Ashwani Kumar Chaudhary, Hanish Bansal, Shivender Sobti, Jagminder Singh and Saurabh Sharma
Department of Neurosurgery, Dayanand Medical College, Punjab, India
*Corresponding Author:
Swarjith Nimmakayala
Department of Neurosurgery,
Dayanand Medical College,
Punjab,
India;
E-mail: swarjithn@gmail.com
Received date: 18 May, 2023, Manuscript No. JSNS-23-99145;
Editor assigned date: 22 May, 2023, PreQC No. JSNS-23-99145 (PQ);
Reviewed date: 05 June, 2023, QC No. JSNS-23-99145;
Revised date: 18 July, 2023, Manuscript No. JSNS-23-99145 (R);
Published date: 25 July, 2023, DOI: 10.4172/2325-9701.1000183
Citation: Nimmakayala S, Chaudhary AK, Bansal H, Sobti S, Singh J, et al. (2023) Clinico-Radiological Profile of Spine Injury at Dayanand Medical College and Hospital. J Spine Neurosurg 12:6.
Abstract
Traumatic spinal injuries comprise of either column fractures or spinal cord injuries or both. Spinal injury is one of the most devastating injuries having a great impact on patients, their families, and society. The major cause of injury in the developed world is due to motor vehicle accidents. Men are mostly affected during their early and late adulthood (3rd decade and 8th decade of life). The age distribution is bimodal. The highest prevalence of traumatic spine injury was seen in age group 15-45 years old, vertebral fractures occur due to force applied to spinal structures. It takes a relatively stronger force to cause a vertebral fracture in healthy bone tissue, but when a bone is weakened due to various causes, vertebral fractures can result from trivial trauma.
This study was conducted in the department of neurosurgery DMCH Ludhiana over a period of one year. About 43 patients of all age groups with spinal injuries were included in the study. Majority of patients in our study were male compared to female (79.1% versus 20.9% of patients) with male to female ratio of 2.7:1, the range of age of patients suffering spine trauma was 18 years to 87 years with mean age being 44.5 years. Majority of spine injuries were seen in students (32.5% of cases), aged less than 30 years. Most of the spine injuries occurred during winter season which accounted for 44.1% of cases, due to low visibility leading to high risk of road traffic accidents. Most common level of spine injury in our study was seen in cervical region (79% of cases) followed by thoracic region (9.3% of cases). The most common type of fracture was burst fracture (39.5% of cases) followed by subluxation fractures (32.5% of cases). In our study about 41.9% of patients underwent surgery and 58.9% of them were managed conservatively. In patients who were managed conservatively 61% of injuries were seen in cervical region. The mean duration of hospital stay was 17.62 days and standard deviation of 10.72. The most common associated injury was head injury in 9.3% of cases followed by chest and long bones injuries with 6.9% of cases each. Mortality rate in our study was 9.3% of cases and the patients who died had cervical spine injury and its complications.
Keywords: Spine injury; Quadriplegia; Neurological deficit; Fixation; Mortality and morbidity
Introduction
Spinal Cord Injury (SCI) is a debilitating neurological condition with socioeconomic impact on affected individuals as well as the health care system. Spinal Cord Injury (SCI) remains one of the most devastating incidents to happen to an individual. This not only has multispectral negative impacts on the affected individual, but also on their family members, society, and the nation as a whole. Etiologically, more than 90% of SCI cases are traumatic and caused by incidents such as traffic accidents, assault, sports, or fall from height [1]. According to the national spinal cord injury statistical center, there are about 12,500 new cases of SCI each year in North America [2]. SCI commonly results from a sudden, traumatic impact on the spine that causes fractures or vertebral dislocation. The male-to-female ratio of 2:1 for SCI, happens more frequently in adults compared to children. Men are mostly affected during their early and late adulthood (3rd decade and 8th decade of life). The age distribution is bimodal, with a first peak involving young adults and a second peak involving those over the age of 60 years [3]. The highest prevalence of traumatic spine injury was seen in age group 15-45 years old, which can be justified by the fact that younger men, as an active group of the community, tend to spend more time outdoors and are therefore at higher risk for trauma, whereas women spend more time at home and face lower trauma risks, especially in rural areas but are more prone for osteoporosis. In India as per estimates, incidence of spinal injury is around 15 to 20 per million populations per year. According to a report by the world health organisation, 82% of the victims of SCI are male, with the majority of them (56%) in the age group of 16-30 years. To make the matter worse 50% to 60% of them remain unemployed following the injury [4]. Such injuries have tremendous consequences on the overall resource allocations in many developing and underdeveloped nations. Traumatic spinal injuries comprise of either column fractures or spinal cord injuries or both. Vertebral fractures occur due to force applied to spinal structures. It takes a relatively stronger force to cause a vertebral fracture in healthy bone tissue, but when a bone is weakened due to various causes, vertebral fractures can result from trivial trauma [5]. Spine injuries have a great impact on patients, their families, and society. It may lead to serious disability when involving the spinal cord with long-term medical complications, including pressure ulcers, autonomic dysreflexia, deep venous thrombosis and pneumonia. People with spinal injury have a high level of mental distress, depression, anxiety, and suicide thoughts because of their low levels of life satisfaction. The cost of treatment of spine injuries and its impact on the health care system is high. Every year, around the world, between 2,50,000-5,00,000 people suffer a Spinal Cord Injury (SCI) due to various reasons. The majority of spinal cords injuries are due to preventable causes such as road traffic crashes fall from height, or violence. Fall from height is the most common cause in Southern Asia. People with a spinal cord injury are two to five times more prone to die prematurely than people without a spinal cord injury, with worse survival rates in low-income and middle-income countries. Re-admission rates within a year of injury for such patients are as high as 27.5%. One cross-sectional study from the US healthcare system found that 95.6% of SCI patients had at least one medical complication at the time of their routine annual check-up. Spinal cord injury is associated with low rates of school enrolment and economic participation, and it carries substantial high individual and societal costs. High-quality radiological investigations are essential for the diagnosis and management of patients with spinal trauma. The clinical outcomes of SCI depend on the severity and location of the lesion and may include partial or complete loss of sensory and/or motor function below the level of injury. Lower thoracic lesions can cause paraplegia while a lesion at the cervical spine level is associated with quadriplegia [6].
Patients who present with complete spinal cord injuries, without any discernible motor or sensory preservation on the neurological examination have a very poor prognosis. On the other hand patients with incomplete spine injury regain a significant amount of neurological function; they may be spared progression into a complete injury with rapid diagnosis, and treatment of fracture elements, hematoma, and other compressive lesions [7]. Kang, et al., review reported that the cervical level of the spine was the most common part of spine to be injured in both developed countries and underdeveloped countries [8]. In the thoracolumbar region, L1 was the commonest site of fracture followed by T12, L4, L2-L3, T11, and T5. As per Indian estimates, an incidence is of around 15-20 per million population per year [9]. The uunited nations has recently implemented the “decade of action for road safety” to reduce this problem globally [10]. SCI typically affects the cervical spine of the spinal cord (50%) with the single most common level affected being C5 (1). Other injuries include the dorsal spine level (35%) and lumbar region (11%). SCI patients often survive these traumatic injuries and live for decades after the initial injury [11]. Motor Vehicle Accidents (MVA) are the principal cause of spine trauma which account for approximately 40% of reported cases. Other injuries are typically the result of a fall from height or sporting activities [12]. The 40-year survival rate of these individuals was 47 and 62% for persons with quadriplegia and paraplegia, respectively. The life expectancy of SCI patients highly depends on the level of injury and preserved functions. For instance, patients with ASIA Impairment Scale (AIS) grade D who require a wheelchair for daily activities have an estimated 75% of normal life expectancy, while patients who do not require a wheelchair and catheterization can have a higher life expectancy of up to 90% of that of a normal individual [13]. The traumatic Spinal Cord Injury (SCI) encompasses a great deal of pain and mental trauma due to disability for patients and their caregivers. To fight this dreaded situation, a deep understanding of various aspects like management issues, complications, new developments, etc. is essential. It is also very important to make proper guidelines for such patients and training of the medical individual. Identification of local problems in transportation and caregiving is also to be taken into consideration.
Pathophysiology of the spinal cord injury
Spinal cord injury can be due to primary or secondary mechanisms as described below.
Primary injury to the spinal cord: The primary mechanism consists of the direct damage to the spinal cord tissue perpetrated by a direct trauma on the spinal cord parenchyma. Among various possible factors are direct impacts with persistent or transient compression, vertebral fracture and displacement, and cord laceration or transection, missile damage (such as in gunshot-related SCI), laceration, shear damage, and distraction.
Secondary injury to the spinal cord: The aforementioned list of possible mechanisms of damage causes a focal neuronal and oligodendrocytes injury resulting in a Blood-Spinal-Barrier (BSB) interruption with increased spinal cord parenchyma permeability and subsequent changes in the concentration of the electrolyte beyond the BSB, with altered sodium and calcium channel function. Direct neurons and oligodendrocytes damage along with damage to the microvasculature, result in focal ischemia and a cellular swelling evolving in cellular death with the release of pro-inflammatory factors, vasoactive peptides, and cytokines, in response to which, there is increased permeability including the inflammation of cells promoting further tissue damage. Among the possible pathogenesis of such focal ischemia, mechanical damage-related vasospasm, micro-hemorrhages, and focal thrombosis caused by platelet aggregation, oxygen free radicals have been advocated. Cellular excess of oxygen free radicals species is formed in response to focal ischemia, because of an incomplete transformation process operated by the dismutase/catalase enzyme system during the electron transport in the mitochondrial oxygen metabolism chain. This results in progressive peroxidation of the cellular inner membrane causing a dysfunction of the phospholipids-dependent enzymes, among which cGMP and Na+/K+ ATPase, with subsequent alteration of further damage [14].
The cord swelling tends to peak after 3 to 6 days and subsides slowly over weeks. This acute phase appears to be followed by a progressive neuron degeneration mediated by persistent inflammation and characterized by extensive microglial and astroglial activation.
Evaluation of spine injury
Both clinical and radiological assessment.
Clinical assessment: Early recognition of traumatic spinal cord injury in the field is crucial to avoid additional cord damage during transportation. However, the early evaluation of any patient with traumatic spinal cord injury includes.
• Sensory, motor examination of reflexes.
• Careful exclusion of other serious injuries such as to the head, chest,
abdomen and pelvis.
• Respiratory failure because of loss of diaphragmatic function.
• Refractory hypotension and bradycardia due to neurogenic shock
(loss of sympathetic outflow along with unopposed vagal activity).
• Spinal shock typically presenting with reflex flaccid paralysis with
anaesthesia below the level of lesion.
Radiological assessment: The main objective of the radiological examination in the clinical setting is to depict the spinal axis and detect spinal trauma rapidly and accurately and to guide potential surgical decompression. Several imaging modalities can be used, but nowadays Multi-Detector Computed Tomography (MDCT) and Magnetic Resonance (MR) imaging are the most important imaging modalities.
Plain X-ray films: Plain X-ray films are a quick‟ way to assess the spine. They are readily available in most hospitals and trauma centers. Plain radiographs may be helpful in fracture screening, and are mainly used to detect a spinal deformity. Indications for obtaining “screening” radiographs of the thoracic and lumbar spine in patients with blunt injuries include: Back pain, fall from a height of 10 feet or more, ejection from a motorcycle/motor vehicle crash at 50 mph or more, Glasgow Coma Scale (GCS) score at admission <8, and neurological deficit.
The “National Emergency X-Radiography Utilization Study (NEXUS) low-risk criteria (NLC)” was first described in 1992. More recently, the “Canadian C-Spine Rule (CCR)” was developed for use with alert (GCS=15) in stable cervical spinal trauma patients. For alert trauma patients who are in stable condition, the CCR was found to be superior to the NLC with respect to sensitivity and specificity for cervical spine injury [15]. Plain X-ray films even with the best possible technique, underestimate the amount of traumatic spine injury, and lesion (s) may be missed.
Computed Tomography (CT): Computed Tomography (CT) and in particular MDCT, plays a critical role in the rapid assessment of the poly-trauma patient. Early on, many trauma centers adopted the technique of thin-section CT with reformation in sagittal or coronal planes to evaluate the spine. CT screening has a higher sensitivity and specificity for evaluating cervical spine injury compared with plain film radiographs. In the cervical spine, CT detects 97% to 100% of fractures. Many major trauma centers nowadays have replaced plain film radiographs with spiral CT or MDCT as the standard of care in the initial evaluation of the cervical spine in moderate to severe trauma patients.
The most important limitation of CT is the inability to provide screening for ligamentous injury and spinal cord lesions. Traditionally, CT of the thoracic and lumbar spine is commonly performed to evaluate suspicious levels on plain film studies, or to evaluate the patient with a known level of injury. Recent literature data indicate that MDCT diagnoses thoracolumbar spine fractures more accurately than plain X-ray films.
Magnetic Resonance Imaging (MRI): MR imaging is the preferred technique for the detection of soft tissue injuries. It is mainly used to exclude occult injuries and to identify spinal cord lesions. MR imaging is the investigation of choice for assessing traumatic lesions involving the intervertebral discs and spinal ligaments. It has been recommended that cervical spine trauma patients with negative standard radiographs and suspected occult cervical injury should be investigated by MR imaging to detect ligamentous injuries that were not seen on plain X-ray studies. A more recent study showed that, in cervical spine trauma, MR imaging was highly sensitive for injury to the intervertebral disc (93%), posterior longitudinal ligament and inter-spinous soft tissues (100%), but was less sensitive in assessing injury to the anterior longitudinal and flavum ligaments. MR imaging is able to reveal the location and severity of the lesion and, at the same time able to indicate the cause of spinal cord compression. This is especially useful in the management of patients with incomplete spinal cord injury, for whom surgical intervention may prevent further deterioration. Several types of traumatic spinal cord lesions can be found: Intramedullary hemorrhage, spinal cord contusion/edema, extrinsic compression by a bone fragment or a traumatic disc herniation, and complete transection of the cord. MR imaging helps in predicting neurological recovery. Neurological recovery is usually insignificant in patients with intramedullary hemorrhage or cord transection, whereas patients with cord edema or contusion may significantly recover from neurological dysfunction.
Neurological assessment of spine injury: A detailed neurological examination is necessary to determine the level of the injury and the severity of the neurological impairment.
• Frankel scale.
• ASIA (American Spinal Cord Injury Association) scale.
• Modified Rankin Scale (MRS).
Although Traumatic Spinal Cord Injury (TSCI) is potentially preventable condition, it is essential to understand the epidemiology and the clinico-radiological profile of SCI to target high risk groups and take preventive measures effectively. In addition, updated knowledge of local prevalence as well as the epidemiological profile of SCI is important for the strategic planning of clinical and supportive measures. At the individual level, information about the prognosis, morbidity and mortality is necessary to answer patient’s questions about their functional capabilities and to provide effective and efficient neurorehabilitation for spine injury patients with neurological deficit.
In the clinical management of patient with spinal cord injury, neurological outcomes are generally determined after 72 hrs after injury using the ASIA scale. This time point has been shown to provide a more precise assessment of neurological impairments after SCI. One important predictor of neurological recovery is to determine whether the spinal cord injury is incomplete or complete [16]. As time passes, SCI patients experience spontaneous improvement of motor and sensory functions. Much of the neurological recovery occurs during the first 3 months and in most patients reaches a maximum by 9 months after injury. However, additional recovery can occur up to 12-18 months post spinal cord injury. Long-term outcomes of SCI are assessed by the level of the injury, the severity of the primary injury, and the progression of the secondary injury. Depending on the level of SCI, patients experience paraplegia or quadriplegia. Paraplegia is defined as the impairment of sensory or motor function in the lower extremities/limbs. Patients with incomplete paraplegia generally have a good prognosis of regaining neurological ability (∼76% of patients) within a year of injury. Patients with complete paraplegia experience complete recovery of lower limb function if their neurological level of injury is above D9 level. An NLI below D9 is associated with a 38% chance of regaining some lower limb neurological function. The Neurological Level of Injury (NLI) is defined as “the most caudal neurological level at which all sensory and motor functions are normal”. In patients with complete paraplegia, the chance of recovery to an incomplete status is only 4% with only half of these patients regaining lost bladder and bowel control. Quadriplegia is defined as partial or total loss of sensory or motor function in all four limbs. Patients with incomplete quadriplegia will have better recovery than complete quadriplegia and paraplegia. Unlike in complete SCI, recovery from incomplete tetraplegia usually happens at multiple levels below the NLI. Patients generally reach a plateau of recovery within 9-12 months after injury. Regaining some motor power within the first month after the spinal injury is associated with a better neurological outcome. Moreover, the appearance of muscle flicker (local involuntary muscle contractions) in the lower extremities is highly associated with recovery of neurological function. Patients with complete quadriplegia, often (66% to 90%) regain function at one level below the injury [17]. Importantly, initial muscle strength is an important predictor of functional recovery in these patients. Complete quadriplegic patients with cervical SCI can regain antigravity muscle function in 27% of the cases when their initial muscle strength is 0 on a 5-point scale. However, the rate of regaining antigravity muscle strength at one caudal level below the injury increases to 97% when the patients have initial muscle strength of 1-2 on a 5-point scale. An association between sensory and motor recovery is demonstrated in SCI where spontaneous sensory recovery usually follows the pattern of motor recovery. Maintenance of pinprick sensation at the zone of partial preservation or in sacral segments has been shown as a reliable predictor of motor recovery. One proposed reason for this association is that pinprick fibers in the lateral spinothalamic tract travel in the proximity of motor fibers in the lateral corticospinal tract, and thus, the preservation of sensory fibers can be an indicator of the preserved motor fibers. Diagnosis of an incomplete spinal injury is of great importance. Failure to detect sensory preservation at sacral segments results in an inaccurate assessment of the prognosis.
Aims and objectives
To determine clinico-radiological profile of spinal injuries in our institute and to identify prognostic factors and determine outcome.
Materials and Methods
The patients presented to Dayanand medical college and hospital emergency, Ludhiana, Emergency with traumatic spine injury were taken into study group. The study period extended from 1st September 2021 to 31st August 2022. Detailed clinical and neurological examinations were performed in all patients. MRI screening of whole spine was performed for all patients who had any of the factors such as-severe mode of injury, spinal pain or tenderness, age older than 60 years, patients with neurological deficit. Data extracted includes-age, socioeconomic status, gender, etiology, severity, management, complications and outcome. For classifying injury severity, American Spinal Injury Association (ASIA) scale was used. Outcome was defined by the state of the patient during and after discharge and based on Modified Rankin Scale (MRS). Statistical analysis was done using SPSS (Statistical Package for Social Science). All the patients with spinal injury with or without neuro deficit.
Pathological fractures and fractures due to systemic prolonged illness are excluded from the study. Data was described in terms of range; mean ± Standard Deviation (± SD), median, frequencies (number of cases) and relative frequencies (percentages) as appropriate. All statistical calculations were done using (Statistical Package for the Social Science) SPSS 21 version (SPSS Inc., Chicago, IL, USA) statistical program for Microsoft windows. Patients were managed according to the neurological examination and radiological findings and appropriate management plan was decided whether surgical or non-surgical. ICU care and ventilator and inotropic support were given as and when required.
Outcome was assessed at the end of hospital-discharge and on regular follow up at 1 month and 6 months. Outcome was graded as: No recovery (no evidence of clinical improvement in the nerve function), partial recovery (some objective clinical recovery), or complete recovery (at the end of the follow-up period, the patient was asymptomatic). Outcome was measured by modified Rankin Score (MRS) and classified into slight disability, moderate disability, moderately severe disability, and severe disability [18].
Results
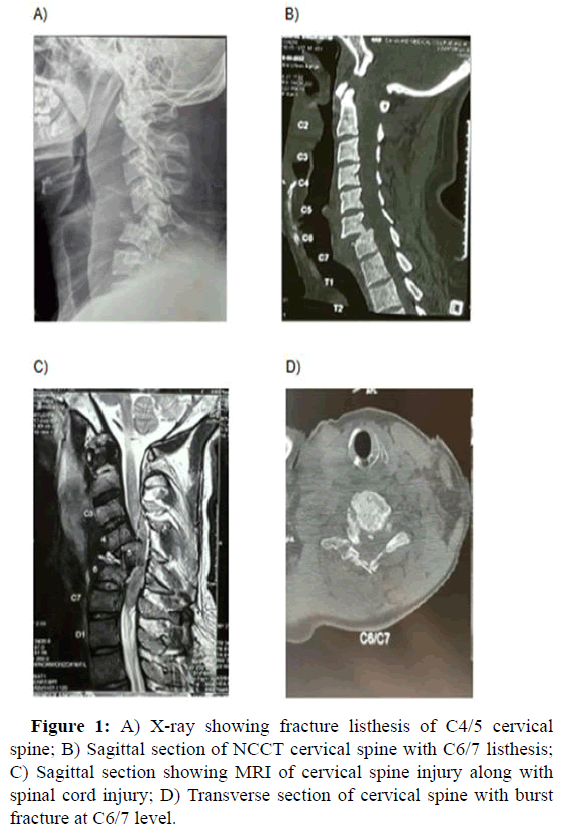
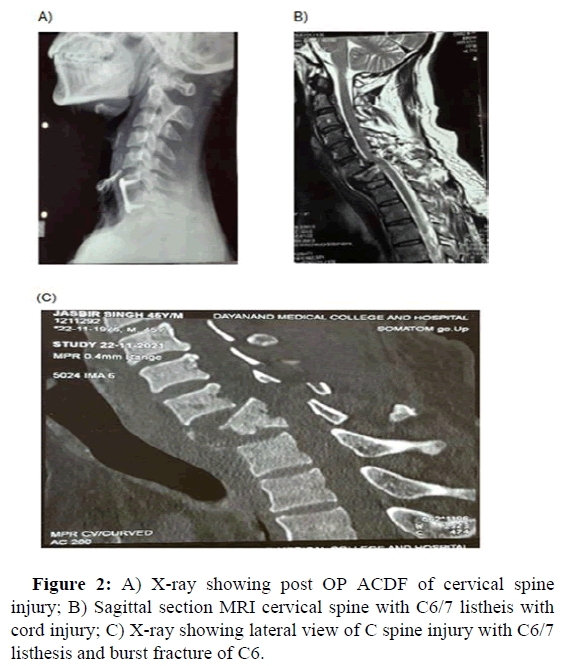
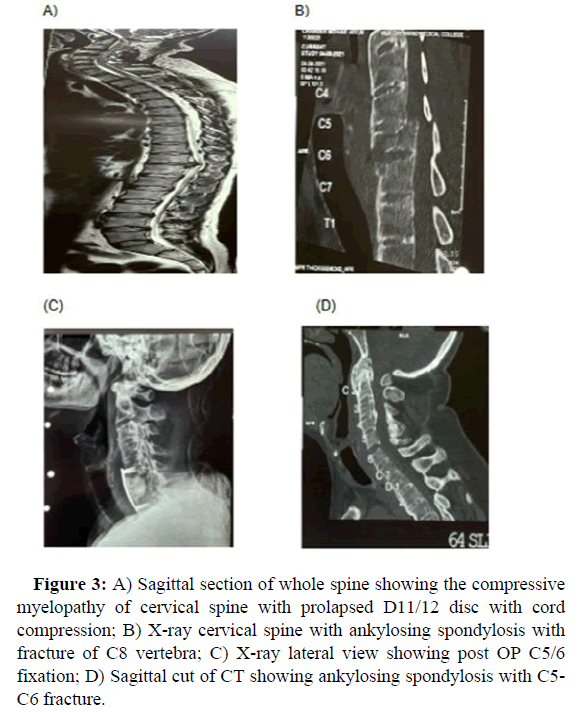
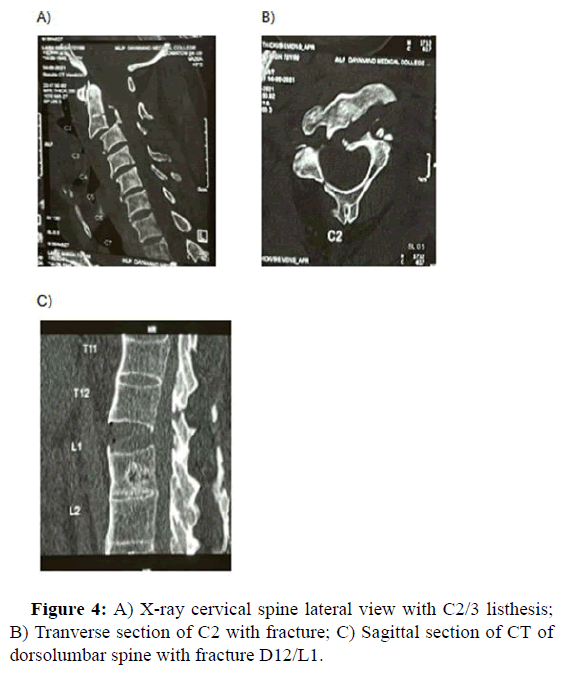
We had a total of 43 patients with spinal injuries who presented to department of neurosurgery over a period of one year from 1st September 2021 to 31st August 2022. Male patients outnumbered female patients with a male to female ratio of 3.78:1. This reflects that spine trauma is more common in males as compared to females (Figure 1A-D). The patients were aged between 18-87 years with mean age being 44.55 years. Of the total 43 patients with spine trauma, majority of patients i.e., 15 (34.9 %) were seen in age group less than 30 years, followed by 41-50 age group (23.3%). Majority of spinal injuries were seen in students (32.5% of cases), followed by farmers (27.9%), businessmen and homemaker (13.9% of cases each), dependent/elderly (11.6% of cases) (Figure 2A-C). In our study, road side accident was the most common cause of spinal injury which accounted for 65.1% of cases followed by history of domestic fall (34.6%). Most of the injuries were observed to have happened during 6 pm to 12 am which accounted for 48.3% of cases followed by 12 pm to 6 pm (34.8%), 6 am to 12 pm (9.3%) and 12 am to 6 am (6.9%). Most of the patients suffered injuries driving post alcohol consumption/drug intoxication. In our study, most of the spinal injuries happened in winter season which accounted for 44.1% (N=19), about 23.2% (N=10) occurred in summer, 20.9% (N=9) in autumn and 13.9% (N=6) in spring season. Most of the injuries occurred in winter due to low visibility and high incidence of RSA in winters (Figure 3A-D). Most of spine injuries presented due to road side accidents to our institute involved light motor vehicles which accounted for 17 (60.8%) followed by two wheeler which happened to be the mode of transport in 11 patients (39.2%). Spine injury with history of fall accounted for (15 patients) 34.8%, of which 5 patients (33.3%) each accounted for fall from stairs and in bathroom, one patient (6.66%) fell from electric pole and 4 (26.6%) accounted for fall from balcony. Glasgow coma scale at the time of admission was analysed, most of the patients (76.7% of them) were admitted with GCS 13-15 and about 14% of them were admitted with GCS 9-12 and 9.3% were admitted with GCS <8 respectively. About 58.1 % (n=25) of patients who presented with spine injury in our institute had ASIA grade A at the time of admission followed by 14% (N=6), 9.3%(N=4), 4.7% (N=2) of cases with ASIA grade D, E, B and C respectively. In about 9.3 % (N=4) of patients ASIA grade couldn’t be determined at the time of admission because patient had low GCS at the time of admission. About 79.0% (N=34) of spine injuries occurred in cervical region followed by 9.3% (N=4), 7% (N=3), 4.7% (N=2) of cases in dorsal region, lumbar region and cervico thoracic region respectively (Figure 4A-C). About 93% of patients had single level fracture followed by two level fractures in 4.6% and 2.3% of them had fractures in more than 3 levels. The most common type of fractures were burst type which accounted for about 39.5% (N=17), followed by 32.5%, 16.25%, 4.65%, 2.32% of cases were subluxation, wedge fractures, odontoid fractures and spinous process, hangman fracture respectively. About 32.4% of spine injury patients have shown associated listhesis along with fractures, and no listhesis was seen in 67.4% of patients. 6 (60.5%) patients had quadriplegia, 7 (16.3%) patients had quadriparesis, 4 (9.3%) had paraplegia, and 2 (4.7%) had paraparesis and 4 (9.3%) patients did not have any neurological deficit [19].
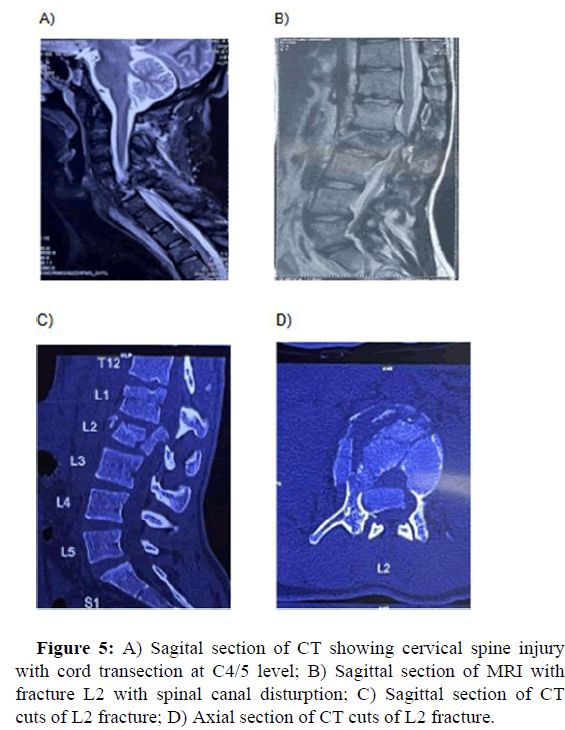
In our study, about 69.7% (N=30) of patients had isolated spine trauma. Head injury was most common 9.3% (N=4) of cases associated injury seen in our study, followed by chest and long bones (6.9% of cases each), abdomen injury in 4.6% and electric burn in 2.3% of patients. About 13.9% of the spine injury patients had normal spinal cord finding in MRI, however about 46.5% (N=20) of them had cord contusion, 20.9% (N=9) had cord compression, 4.6% (N=2) of cases had cord transection, 13.9% (N=6) had cord compression along with contusion. In our study of 43 patients, about 67.4% had no associated co morbid conditions, while 11.6% of them had hypertension, 9.3% of them had diabetes, 7.0% of them had septic shock and 2.3% of them had spinal shock and 2.3 % of them had ankylosing spondylosis (Figure 5A-D). Of all the patients, about 41.9 % (N=18) of patients underwent surgical intervention while 58.1% (N=25) of them were managed conservatively. About 41.9% (N=18) of cases were managed surgically. Out of which, about 61.1% of them were performed in cervical region followed by 16.6 % each in thoracic and lumbar regions and 5.5% of each in cervico-thoracic and thoracolumbar regions. Those patients who underwent surgical intervention for cervical spine injury underwent anterior cervical discectomy and fusion and those with dorsal and lumbar spine injury underwent decompression and transpedicle screw fixation.
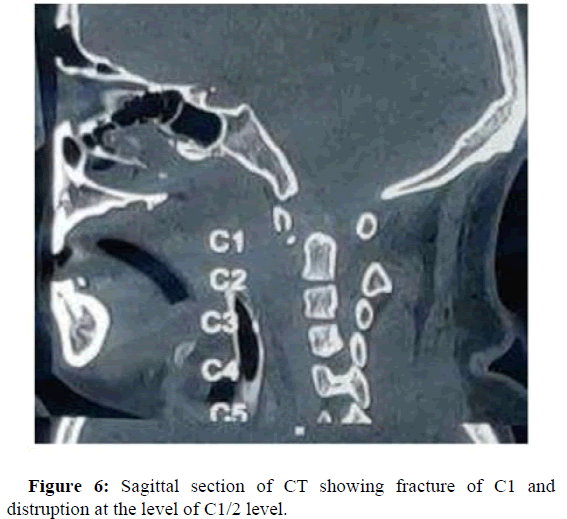
In our study, 34.8% (N=15) of patients had hospital stay between 10-19 days followed by 27.9% (N=12) stayed for less than 10 days, 23.2% (N=10) stayed for more than 30 days and 13.9% (N=6) of patients had hospital stay of 20-29 days with a mean stay of 17.62 and standard deviation of 10.72. About 34.8% of patients had MRS score of 4, followed by 18.6% of patients with score of 5, 13.9% of patients with score 3.11.6% of patients with score of 2, 9.3% with score of 6 and 0 each, 2.32% of them with score of 1 (Figure 6).
Figure 3: A) Sagittal section of whole spine showing the compressive myelopathy of cervical spine with prolapsed D11/12 disc with cord compression; B) X-ray cervical spine with ankylosing spondylosis with fracture of C8 vertebra; C) X-ray lateral view showing post OP C5/6 fixation; D) Sagittal cut of CT showing ankylosing spondylosis with C5- C6 fracture.
Discussion
Majority of patients in our study were male compared to female (79.1% versus 20.9% of patients) with male to female ratio of 2.7:1, this coordinates with other studies in the literature. In Karammehmetoglu, et al., study the male to female ratio was 3:1. Pickett, et al., in their study reported the male to female ratio in the age groups from 10 to 69 years range 2.2 to 3.5:1. Calancie, et al., reported about 76.4% of spine injuries in males which is similar to our study in which 79.1% of spine injuries were seen in males. Lofvenmark, et al., reported about 71% of spine injuries in male [20]. Thus male to female ratio in our study is similar to previous studies in the literature. In our study, age groups ranged from 18 to 87 years with the mean age of 44.5 years. About 34.9% of spine injuries were seen in the age group less than 30 years followed by 23.3% of cases in 41 to 50 years group. This is similar to previous studies in literature. Calancie, et al., reported the average age of spine injury as 39.8 ± 16.8 years. Chhabra, et al., Thomson, et al., and Anadalib, et al., in their study reported that the mean age of spine injury as 34 years, 39.1 ± 15.9 years and 42.7 ± 16.8 years respectively. The age group in our study is similar to previous studies in the literature. In our study majority of the spine injuries were seen in people who were students (32.5% of patients), followed by farmers (27.9% of patients), businessman and homemakers which accounted for 13.9% of patients each and then dependents (5% of patients). Chhabra, et al. reported that most of the spinal injuries were seen in non-professional job (18.02% of cases) followed by professional private jobs (17.26%), students (12.26%), labourers (8.04% of cases). Mathur, et al., reported that about 23.3% and 22.9% of spinal injuries were seen in farmers and labourers respectively. Liu, et al., found that most common occupation of patients with spinal cord injury as workers (28.6%) followed by office clerk (16.8% of cases). In our study most of the injuries were observed to have happened during 6:00 PM to 12:00 PM (48.3% of cases) followed by 12:00 PM to 6:00 PM (34.8%), then during morning hours 6:00 AM to 12:00 PM (9.3%) and 12:00 AM to 6:00 AM (6.9% of cases). No literature is available to compare our study with previous literature. In our study, most of the spine injuries happened during winter season which accounted for 44.1% (N=19). About 23.2%, 20.9%, 13.9% of spine injuries were seen in seasons of summer, autumn and spring respectively. In our study, most of the injuries happened in winter season because of low visibility leading to high incidence of road traffic accidents. Chhabra, et al., reported that most injuries were seen in the month of May and June. Johnson, et al. found that incidents of spine injury were higher during summer and autumn months. Other previous literature reported that most of the injuries occurred during summer season due to increased travelling activities during summer time. In our study road traffic accident was the most common cause of spine trauma which accounted for 65.1% of cases, followed by fall history which accounted for 34.8% of them. Among patients with history of fall, fall from Stairs and in bathroom accounted for 33% of them, and fall from balcony was the second most common cause in patients with history of fall which accounted for 26.6% and fall from electric pole accounted for 6.6% of them. when compared with previous literature, some literature reported that road traffic accident was the most common cause followed by fall history whereas in some other literature it was contradictory with history of fall as most common cause followed by road traffic accident. Mathur, et al., reported that fall from heights (53% of them) was most common cause followed by road traffic accidents (28%). Joseph, et al., reported that most common cause of spinal injury was fall (58%) followed by transport related events (40%) respectively. Liu, et al. reported that RTA the most common cause and history of fall the second most common mode of injury. This observation is similar to that of most other studies from developed countries but in contrast Indian studies show that fall is the most common mode of injury. Most of the spine injuries caused due to a RSA, presented to our institute were most commonly caused by accidents involving light vehicles which accounted for 60.8% of cases followed by accidents involving 2 wheelers which accounted for 39.2% of cases. Most of the accidents happened in secondary type of roads i.e., state highways rather than the national highways. Lofvenmark, et al., reported that the main cause of traumatic spine injury was RSA followed by assault and fall. Chhabra, et al., reported that RTA was the most common cause and fall the second most common mode of injury. This observation is similar to that of most other studies from developed countries but in contrast to other Indian studies in which fall is the most common mode of injury. Few studies also revealed that major cause of traumatic spine injury in North America, Western Europe and Australian regions involved 4 wheeled motor vehicle accidents. Chhabra, et al., series reported RTA on highway roads in 39.5% of the cases. In our study spine injuries due to RSA occurred mostly due to reckless driving accompanied by poor condition of the road, alcohol consumption and drug intoxication. About 58.1% of patients who presented with spine injury in our institute had ASIA grade A at the time of admission, followed by 14%, 9.3%, 4.7% of cases with ASIA grade D, E, B and C respectively. In 4 patients (9.3%) ASIA grading could not be determined at the time of admission due to poor GCS. Derakhshanrad, et al., reported that most common neurological type of injury was ASIA grade A (53.5%) followed by 18.7%, 17.6%, 9.6% and 0.6% as ASIA grade B, C, D, E respectively. Halovorsen, et al., also reported that most common injury at the time of admission was complete injury ASIA grade at which was seen in 77% of cases. Rahimi Movaghar, et al., reported the complete injury was more common than incomplete injury complete SCI 56.5%, incomplete SCI 43% of cases.
In our study about 79% of spine injuries occurred in cervical region followed by 9.3% (N=4), 7% (N=3), 4.7% (N=2) of them in dorsal region, lumbar region, cervico-thoracic region respectively in previous literature. Roche, et al., reported that 42.6%, 14.29%, 7.14%, 28.57%of spinal injuries were cervical, thoracic, lumbar and sacral spine injuries. Hagen, et al., also reported that most of the spine injuries were seen in cervical and thoracic region which accounted for 52.4% and 29.5% respectively. Liu, et al., also reported that 54% of their patients had cervical injuries. In our study most of the spine injuries were seen in cervical region. Calenoff, et al., reported that, of the 43 patients studied, 2 patients sustained injuries at 2 level (4.6% of cases) and 1 patient showed fracture at more than 3 levels (2.3% of cases). Mortazavi, et al., reported that the incidence of multi levels final involvement reported in literature ranges from 6% to 50% in children. In their study 48 (26.2%) patients had injuries involving more than one segment of the spine. In our study about 93% (N=40) of patients presented with single level fracture followed by 4.6% and 2.3% of patients had 2 level and more than 3 level fractures respectively. In our study, the most common type of fractures were burst fractures which accounted for 39.5% of cases followed by 32.5% (N=17), 16.25% (N=14), 4.6%, 2.3% of cases with subluxation, wedge fracture, spinous process and hangman fracture respectively. Roche, et al. reported that in 285 patients there were a total of 380 injuries to the vertebral column consisting of 366 fractures, 8 subluxation, 2 fracturesubluxations and 1 dislocation. Andalib, et al., reported that most common fractures seen in cervical spine were translational injury (19.4% of cases), compression fracture (10.4%), whereas in thoracic regions most common fractures seen were burst fractures (62.7% of cases), wedge fractures (21.3% of cases) and in lumbar regions most common fractures seen were burst fractures (75.4% of cases), locked facet was seen in 4.4%. In our study about 86.1% of patients had cord abnormalities, 13.9% of them had normal MRI, 46% patients with spine injury had cord contusion. 29.5% of patients had cord compression, 13.9% had cord compression along with contusion and 4.6% of patients had cord transections. Parashar, et al., MRI examination revealed that cord abnormalities were present in 47 out of 62 patients i.e. 75.8% of the patients, in 26.32% no abnormality was noted in cord. Kulkarni, et al., revealed presence of cord abnormalities in 70% patients and skeletal abnormalities in 78% of patients. In our study about 41.9% of patients underwent surgery while 58.1% were managed conservatively. In patients who were managed surgically, about 61.1% of them had spinal injury in cervical region followed by 16.6% in thoracic and lumbar region each, 5.5% of cases in cervicothoracic and thoracolumbar regions each. In patients who were managed conservatively about 72% of them had no indication for surgery, 8% died before surgery and 20% of them did not give consent for surgery. Wang, et al., in their study reported that 2763 (79.24%) received surgical treatment and 724 (20.76%) received conservative treatment. Michelle, et al., index study over the last 10 years reported surgical rate was seen in 77% of the patient switch spine injury. Pandey, et al., index study showed that 17 patients were given injection Solumedrol, et al., with conservative treatment, 35 (60%) patients were given only conservative treatment and 7 (11.66%) patients were operated. In our study, the surgical rate was similar to the previous study in literature. In our study 34.8% (N=15) of patients had hospital stay between 10-19 days followed by 27.9% (N=12) stayed for less than 10 days, 23.2% (N=10) stayed for more than 30 days and 13.9% (N=6) patients had hospital stay of 20-29 days with a mean stay of 17.62 days and standard deviation of 10.72. Wang, et al. reported that mean hospital stay in patients with traumatic spinal cord injury was 17 days (range 1 to 80 days). Wank, et al., also reported that duration of hospitalization in patients with spinal cord injury ranged from 1 to 375 days with an average of 17.5 days. Singh, et al., reported that average hospital stay in their study was 39.5 days (range 7 to 93 days) thus the duration of our study is similar to previous study in the literature. In our study about 69.7% (N=30) of patients had isolated spine trauma. Head injury was most common 9.3% (N=4) of patients associated injury seen in our study, followed by chest and long bone (6.9% of cases) each, abdomen injury in 4.6% and electric burn in 2.3% of patients. Chhabra, et al., showed that out of other injuries associated spinal injuries, orthopedic injuries were commonest (23.18%) injuries, followed by chest injuries (11.07%), head injuries (5.548%) and other spine fractures (2.94% of cases). Wang, et al., reported that injuries associated with spine trauma included craniocerebral injury (11.09%), front-facial injury (22.79%), chest/ abdominal injuries (20.1%), pelvic injuries (14.4%) and limb fractures (31.8% of cases). Mathur, et al., reported in their studies that extremity and rib fractures (10.6%) and head injuries (7.2% of cases) were common associated injuries. In our study the complications that occurred during hospital stay included requirement of tracheostomy, sepsis. Santos, et al., reported that medical complications were observed in 45% of the patients, pneumonia being the most frequent one. Other complications included pressure ulcers in 3.7% of cases, urinary tract infections in 2.3% of cases, deep venous thrombosis in 3.2%, wound infections and others 34% of cases. Wang, et al. reported that during hospitalization, a total of 1341 patients experienced complications with the percentage of 38.4%. Among all complications pulmonary infection was the most common 32.5% of cases, followed by hyponatremia 24.3% of cases, bedsore 16.3% of cases, urinary tract infection 12.5% of cases, deep venous thrombosis 11.7% of cases and others 2.53% of cases. Mu, et al., reported that out of total 294 of patients with cervical spine injury 52% of them received tracheostomy. In our study also most of the patients who underwent tracheostomy suffered from cervical spine injuries. In our study, on follow up about 34% of patients had MRS score of 4, followed by 18.6% of patients with score of 5, 13.9% of patients with score 3. 11.6% of patients with score of 2, 9.3% with score of 6 and 0 each, 2.32% of patients with score of 1. No studies were available in the literature to compare where MRS is used to compare in spinal injuries. In our study, among the patients who died, all 4 had cervical spine injury. No death was seen in patients with dorsal or lumbosacral fractures. Among the causes of death, respiratory failure and sepsis were major causes. In our study, mortality rate was seen in 9.3% of cases and among who died all of them had cervical spine injuries. No death was seen in dorsal, lumbar, sacral fractures. Shock, sepsis and respiratory failure were observed as causes of death. The patients who died were managed conservatively. Calancie, et al., reported that 17 of their patients died during the 3 years follow up. Many of them were dependent on ventilator from the time of injury and later developed pulmonary insufficiency. 3 subjects died of pulmonary embolism and GI bleeding. Feng, et al., eight patients died after operation, 7 had cervical spine injury and 1 patient with lower dorsal fracture, in the end 4 patients died because of respiratory failure, 2 died from acute pulmonary embolism and 2 died due to multi-organ failure. Kang, et al., estimations of spinal cord injury among developed nations varied from 3.1 to 22.2% while mortality in underdeveloped nations ranged from 1.4 to 20%. In our study the mortality rate was similar to previous literature.
Conclusions
• Spine trauma was more common in males than females with male to
female ratio 3.7:1.
• The range of age of patients suffering spine trauma was 18 years to
87 years with mean age being 44.5 years.
• Majority of spine injuries were seen in students (32.5% of cases),
aged less than 30 years.
• Most of the spine trauma cases were seen during 6 PM TO 12 AM
which accounted to 48.3% of cases.
• Most of the spine injuries occurred during winter season which
accounted for 44.1% of cases, due to low visibility leading to high
risk of road traffic accidents.
• The most common cause of spine injury was road traffic accidents
and accounted for 65.1% of cases.
• Most of the spine injuries due to RSA were caused by 4 wheeler
light motor vehicle accounting to 60.8% of cases.
• Most of spine injuries due to fall were domestic fall from stairs/in
bathroom which accounted for 33% each.
• Most of the patients with spine injury presented to our institute were
within GCS 13-15 which accounted for 76.7% of cases.
• Most common ASIA scale at the time of admission was GRADE A
which accounted for 58.1% of cases.
• Most common level of spine injury in our study was seen in cervical
region (79% of cases) followed by thoracic region (9.3% of cases)
• In our study about 93% of patients had single level of fracture
followed by 2 level fractures in 4.6% and 2.3% of cases had more
than 3 levels of fracture.
• The most common type of fracture was burst fracture (39.5% of
cases) followed by subluxation fractures (32.5% of cases).
• Most common MRI finding in our study was cord contusion (46.5%
of cases) followed by cord compression (20.5% of cases).
• In our study about 41.9% of patients underwent surgery and 58.9%
of them were managed conservatively.
• In patients who were managed conservatively 61% of injuries were
seen in cervical region.
• In conservatively managed patients, 72% did not have indication for
surgery, 8% died before surgery and 20% of them did not give
consent for surgery.
• In patients who were surgically managed about 61.1% of them had
injury in cervical region and they underwent anterior cervical
discectomy and fusion (ACDF/ACCF) and those with dorsal and
lumbar spine injury underwent decompression and transpedicle
screw fixation.
• The mean duration of hospital stay was 17.62 days and standard
deviation of 10.72.
• The most common associated injury was head injury in 9.3% of
cases followed by chest and long bones injuries with 6.9% of cases
each.
• In our study, about 34% of patients had an MRS score of 4, followed
by 18.6% of patients with score of 5, 13.9% of patients with score
3,11.6% of patients with score of 2, 9.3% each with score of 6 and
0 , 2.32 % of them with score of 1.
• Mortality rate in our study was 9.3% of cases and the patients who
died had cervical spine injury and its complications
• Most common cause of death in our study was sepsis (4.6% of
cases) followed by respiratory failure and shock (2.3% of cases
each).
International Spinal cord Society (ISCoS) has decided to observe spinal cord injury day on 6th September every year with the intention of increasing awareness among the general public. According to the observation and results from our study the most common cause of spine injury was road traffic accidents. Wearing protective headgear, seat belts while driving is highly recommended, improving road conditions, increasing de-addiction clinics and avoiding the low visibility conditions or foggy conditions while driving is recommended to prevent head and spine injuries. Fall from height was another important cause of spinal injury. In our region and country as a whole, the emergency services in primary healthcare centres provided to patients with spine trauma is not up to the mark. A Teaching and awareness program to healthcare workers regarding primary care of patient who sustains spine trauma is very important step that is much needed. Knowledge of how to transport patient who sustained spine injury is very important regarding airway management in cervical trauma, immobilization of neck, use of spine board while transporting suspected spine trauma patient, dose of methylprednisolone are some of the very crucial steps initially and determines the final outcome of patients. On reaching well equipped medical center decision regarding surgical or non-surgical medical assistance needs to be taken. For those patients who require surgery, early decision is always recommended even though its role in determining the outcome of patient is controversial once the spinal shock or associated acute conditions are resolved. Post-surgery or in those patients who are quadriplegic or paraplegic aggressive nursing care and physiotherapy is recommended to prevent complications like bedsores, pneumonia and DVT. Lastly, as most of the patients are quadriplegic or paraplegic and usually they become dependent on the family members for rest of their life, so aggressive rehabilitation, encouragement and family support is crucial and play significant role in their life.
References
- Hachem LD, Ahuja CS, Fehlings MG (2017) Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J Spinal Cord Med 40:665-675.
[Crossref] [Google Scholar] [PubMed]
- Stein DM, Pineda JA, Roddy V, Knight WA (2015) Emergency neurological life support: Traumatic spine injury. Neurocrit Care 23:S155-S164.
[Crossref] [Google Scholar] [PubMed]
- Grivna M, Eid HO, Abu-Zidan FM (2015) Epidemiology of spinal injuries in the United Arab Emirates. World J Emerg Surg 10:20.
[Crossref] [Google Scholar] [PubMed]
- Myers ER, Wilson SE (1997) Biomechanics of osteoporosis and vertebral fracture. Spine 22:25S-31S.
[Crossref] [Google Scholar] [PubMed]
- Wilson JR, Cadotte DW, Fehlings MG (2012) Clinical predictors of neurological outcome, functional status, and survival after traumatic spinal cord injury: A systematic review. J Neurosurg Spine 17:11-26.
[Crossref] [Google Scholar] [PubMed]
- Suman NV, Chincholi S (2017) Profile of patients with thoracolumbarspine injury: A descriptive study. Int J Orthop Sci 3:882-884.
- Kang Y, Ding H, Zhou H, Wei Z, Liu L, et al. (2018) Epidemiology of worldwide spinal cord injury: A literature review. J Neurorestoratology 6:1-9.
- Srivastava RN, Singh A, Garg RK, Agarwal A, Raj S (2015) Epidemiologyof traumatic spinal cord injury: A SAARC perspective. Int J Mol Biol Biochem 3:9-22.
- Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, et al. (2012) Life expectancy after spinal cord injury: A 50-year study. Spinal Cord 50:803-811.
[Crossref] [Google Scholar] [PubMed]
- Parizel PM, van der Zijden T, Gaudino S, Spaepen M, VoormolenMH, et al. (2010) Trauma of the spine and spinal cord: Imaging strategies. Eur Spine J 19:S8-S17.
[Crossref] [Google Scholar] [PubMed]
- Shavelle RM, Paculdo DR, Tran LM, Strauss DJ, Brooks JC, et al. (2015) Mobility, continence, and life expectancy in persons with Asia impairment scale grade D spinal cord injuries. Am J Phys Med Rehabil 94:180-191.
[Crossref] [Google Scholar] [PubMed]
- Denis F (1983) The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine 8:817-831.
[Crossref] [Google Scholar] [PubMed]
- Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, et al. (1969) The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia I. Paraplegia 7:179-192.
[Crossref] [Google Scholar] [PubMed]
- Tsou PM, Wang J, Khoo L, Shamie AN, Holly L (2006) A thoracic andlumbar spine injury severity classification based on neurologicfunction grade, spinal canal deformity, and spinal biomechanical stability. Spine J 6:636-647.
[Crossref] [Google Scholar] [PubMed]
- Ferguson RL, Allen BL (1984) A mechanistic classification of thoracolumbar spine fractures. Clin Orthop Relat Res 159:177-188.
[Google Scholar] [PubMed]
- Singh K, Vaccaro AR, Eichenbaum MD, Fitzhenry LN (2004) The surgical management of thoracolumbar injuries. J Spinal Cord Med 27:95-101.
[Crossref] [Google Scholar] [PubMed]
- Bensch FV, Koivikko MP, Kiuru MJ, Koskinen SK (2006) The incidenceand distribution of burst fractures. Emerg Radiol 12:124-129.
[Crossref] [Google Scholar] [PubMed]
- McAfee PC, Yuan HA, Fredrickson BE, Lubicky JP (1983) The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am 65:461-473.
[Google Scholar] [PubMed]
- Bernstein MP, Mirvis SE, Shanmuganathan K (2006) Chance type fractures of the thoracolumbar spine: Imaging analysis in 53 patients. AJR AmJ Roentgenol 187:859-868.
[Crossref] [Google Scholar] [PubMed]
- Tator CH (1995) Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 5:407-413.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi