Review Article, J Nanomater Mol Nanotechnol Vol: 9 Issue: 1
Cholesterol Metabolism: As a Promising Target Candidate for Tuberculosis Treatment by Nanomedicine
Parv Tanwar, Shivangi and Laxman S Meena*
CSIR-Institute of Genomics and Integrative Biology, Mall Road, Delhi, 110007, India
*Corresponding Author : Laxman S Meena, Ph.D.
CSIR-Institute of Genomics and Integrative Biology, Mall Road, Delhi, 110007, India
Tel: 0091-11-27002200
E-mail: meena@igib.res.in; laxmansm72@yahoo.com
Received: October 30, 2019 Accepted: November 15, 2019 Published: November 26, 2019
Citation: Tanwar P, Shivangi, Meena LS (2019) Cholesterol Metabolism: As a Promising Target Candidate for Tuberculosis Treatment by Nanomedicine. J Nanomater Mol Nanotechnol 8:4.
Abstract
We are facing a tremendous need to develop anti-tuberculosis (TB) drugs due to extreme rise in incidence and mortal cases of this disease. Mycobacterium tuberculosis (M. tuberculosis), the causative agent behind this malady have attained the drug-resistant characteristic by adding mutation at its genetic level and modifying their metabolic pathways. An important metabolic pathway employed in the bacterium is cholesterol metabolic pathway. Cholesterol is needed by the bacterium for attachment, entry, as a major nutrient source, persistence, and infection in the host. Manifold roles of cholesterol in M. tuberculosis making it an important mark to target the survival and virulence of the bacterium. Genetic regulation of cholesterol metabolism is a complex phenomenon. This review emphasizes the close and quick view towards cholesterol metabolism in M. tuberculosis and nanotechnology strategies to target this pathway. Targeting this pathway with specific biomarker designed nanoparticles loaded with anti-cholesterol drugs (Azasteroid, steroid, econazole, etc.) might be a better way of treatment. Antituberculosis drugs that could target their specific enzymes could lead to hindrance in uptake and degradation of this lipid and thus lead to nutrient depletion and accumulation of toxic metabolites which may ultimately lead to bacterial death.
Keywords: M. tuberculosis; Cholesterol; Mannose; Nano particle; Econazole; Dosage
Introduction
Mycobacterium tuberculosis H37Rv (M. tuberculosis) which causes disease Tuberculosis (TB) in humans is one of the major reasons for death due to an infectious disease. In 2017, 10 million people were diseased with TB, and 1.6 million died from the disease. It is now known that M. tuberculosis survival mechanism depends upon many factors such as the layer of mycolic acid, dormancy and persistence, protection against oxidative radicals, Vitamin D3, cholesterol, and retinoic acid, etc. Vitamin D3 and cholesterol play crucial role in growth of the bacterium [1]. TB is currently decreasing with rate of 2% worldwide but the rate is needed to be increased up to 4%-5% to end this disease in the coming years. Major countries contributing to the widespread disease are developing countries or southern Asian such as India, Pakistan, China, Philippines, Indonesia, Bangladesh, South Africa, and Nigeria. TB mostly affects adults in their productive years but the disease can be found in every age group in developing countries, approximately 1 million children are living with TB and 230,000 deceased in year 2017 itself. The global prevalence of this disease is comprised of the current epidemic of co-infection of HIV and diabetes with TB. The condition is becoming much worse with an alarming increase in drug-resistant M. tuberculosis strains. Currently BCG vaccine is the only vaccine being used to cure the disease but is now becoming invalidated due to genetic drifts in nature of the bacterium. Despite availability of BCG vaccines, Isoniazid and rifampicin are other two primary first-line anti-TB first-line drugs that are widely used in treatment of this disease. M. tuberculosis employed an efficient phenomenon to rescue from host environment and additive mutation effect in their genome. These characteristics of this bacterium make treatment of the disease complex and give rise to generation of Multiple Drug-Resistant Tuberculosis (MDR-TB), XDRTB and TDR-TB. Second and third-line drug regimens as shown in Table 1 are the extensive therapy to cure this disease by applying more antibacterial effect [2-15]. Although TB is caused by spreading of the bacteria through air channels while coughing and sneezing etc. But, it is seen that smoking is also attributing a significant percentage of 7.9% to the deadly disease. Along with it TB with HIV is common and confounded now and forms a deadly combination. People infected with HIV are 20 to 30 percent prone to TB rather than people without HIV [16]. In year 1882 the deadly disease was discovered and till now the disease is making its way to proliferate and even spreading on a large scale. Even after whole-genome sequencing been completed for this bacterium and more than 140 passed years, we are still unable to completely eliminate this disease. The notorious bacterium has very complex and rigid structure and employs several mechanisms to survive inside host cell. On the primary basis, it forms and resides inside a granulomatous lesion in the alveolar sacs for a longer period of time without any interference from host immune system. Granuloma is a cluster of immune cells that encircle or trap any foreign strain, which is not phagocytosed by macrophage cells. The immune cells that participate in formation of this granuloma are mainly highly differentiated cells such as epithelioid cells, multinucleated giant cells, B-cells, T-cells, macrophages cells that give granuloma a foamy appearance. Granuloma accomplishes a mutual relationship between host and bacterium, M. tuberculosis can stay inside the granuloma for years in dormant state and in time of immune-compromised state it can escape from the granuloma to proliferate which results into the symptoms of active disease. Despite residing inside the granulomatous lesion of the host cells, this bacterium applies several other mechanisms also to escape from host stress environment and defense mechanism (Figure 1). These responses include up-regulation of genes involved in stress response conditions, mutation in genome, modifying its metabolic pathway, etc [17].
| Drug | Mode of action | Invention | Reference | |
|---|---|---|---|---|
| First Line Drugs | Isoniazid | Inhibit cell wall, nucleic acid synthesis, causes metabolic depression by activation through katG that generates NAD(+) and NADP(+) | 1952 | 2 |
| Rifampicin | Inhibit bacterial RNA polymerase | 1966 | 3 | |
| Ethambutol | Inhibit synthesis of cell wall component arabinogalactan and Lipoarabinomannan (LAM) by inhibiting arabinosyltransferases: EmbA, EmbB, and EmbC | 1961 | 4 | |
| Pyrazinamide | Inhibit membrane transport and disrupt membrane potential | 1952 | 5 | |
| Second Line Drugs | Ethionamide | Disrupts mycolic acid biosynthesis and responsible for inhibiting acid fastness | 1956 | 6 |
| Prothionamide | Disrupts mycolic acid biosynthesis and responsible for inhibiting acid fastness | 1956 | 6 | |
| Capreomycin | Inhibit mycobacterial protein synthesis by interruption in binding with inhibit 30S and 50S ribosomal subunits | 1960 | 6 | |
| Bedaquiline | Inhibit ATP production by binding to mycobacterial ATP synthase | 2012 | 7 | |
| Kanamycin | Inhibit protein synthesis by binding with 30S subunit of ribosome | 1957 | 6 | |
| Levofloxacin | Inhibit DNA gyrase and DNA topoisomerase IV | 1990 | 8 | |
| Moxifloxacin | Inhibit DNA gyrase and DNA topoisomerase IV | 1990 | 8 | |
| Para-aminosolicylic acid | Inhibit the action of dihydrofolate reductase | 1943 | 9 | |
| Third Line Drugs | Bedaquiline | Inhibit ATP production by binding to mycobacterial ATP synthase | 2012 | 7 |
| Delamanid | Inhibit synthesis of methoxy mycolic acid and ketomycolic acid component of cell wall | 2014 | 10 | |
| Clofazimine | Competitive inhibitor of menaquinone, a cofactor of mycobacterial ETC and release reactive oxygen species | 1986 | 9 | |
| New Drug, B Candidate | SQ-109 | Inhibit activity of MmpL3 | 10 | |
| Linezolid | Bind with 50s subunit and inhibt formation of initiation complex of protein synthesis | 1980s | 11 | |
| Rifapentine | Inhibit mycobacterial DNA polymerase | 12-13 | ||
| Meropenem | Inhibit cell wall synthesis | 14 | ||
| Imidazopyridine Amide | Inhibitor of mycobacterial Electron Transport Chain | 14 | ||
| Macrolide | Inhibit protein synthesis by binding to the 50s subunit | 15 |
Table 1: List of all drugs that had been used to cure Tuberculosis (TB).
Figure 1: Establishment of granuloma: Infection of M. tuberculosis begins with inhalation of bacilli during contact with an infectious person. Bacterium resides into alveolar macrophage where it establishes a mutual relationship with host in form of granuloma. In granuloma, M. tuberculosis can reside in persistent manner without interference of host and on the other side host immune cells (B cell, T cell, NK cell, macrophage, dendritic cell, neutrophils etc.) invade bacterium and defend host from its diffusion.
The main focus which we try to elaborate and the major aim of this article is to exaggerate cholesterol metabolism in M. tuberculosis and how much it is important for its survival? If it is necessary to a great extent, then how can we target this metabolic pathway so that growth of this bacterium could be halted which ultimately leads to lesser epidemic of this disease? In order to focus on the mentioned research arm, we are aiming towards developing various strategies employed in the development of novel drug targeting catabolism of cholesterol of M. tuberculosis [18]. This would be done with the help of nanobiotechnology where nanoparticle would be loaded with various types of anti-cholesterol drugs. Poly(lactic-co-glycolic acid) (PLGA) nanoparticles are best-known class of nanoparticles which are biodegradable and biocompatible polymers that are hydrolytically degraded into nontoxic monomers, oligomers, lactic acid, and glycolic acid. Nanoparticle would be loaded with first-line drugs such as isoniazid, rifampicin, pyrazinamide, ethambutol, econazole, and steroid fibrates. The drugs and steroids might play very important role in cholesterol metabolism and reducing the disease [19].
As mentioned in various reports and also in the above lines of this article, Cholesterol metabolism is one of the main and major arms that work for bacterial survival, growth, and virulence. Targeting this arm with the help of nanoparticle loaded with effective drug turn out to be an efficient technology towards eradicating or minimizing the threat of this disease.
The fundamental role of cholesterol in M. tuberculosis
Mycobacterium resides inside alveolar macrophages in a very nutritionally constrained environment and has capability to persist in this environment for many years. It had been said that most of the bacteria utilize the catabolite repression phenomenon in which they prefer to use one substrate for growth over the other [20]. But as most of the bacterial species, Mycobacterium does not obey the same rule of catabolite repression. This bacterium evolved with the ability to co-catabolite different carbon sources including acetate, dextrose, glycerol, etc. with different metabolic fate which ultimately leads to maximization of its monophasic growth [21].
There are various reports which proved that intracellular pathogens obtain their nutrient from surrounded lipids of the host and they utilize these lipids as their primary carbon source rather than using carbohydrates. Host cells comprise different types of lipids and one of the major lipids that present is cholesterol. Cholesterol accompanies a major part of lipid in eukaryote cell and thus this is also a major lipid from which M. tuberculosis obtains its nutrients [22]. This was also proved by a study that shows impair growth of M. tuberculosis in the absence of cholesterol. Cholesterol is majorly required for persistence of the bacterium in addition to establishing and propagating infection inside host cells [23]. The impaired growth of the bacterium in the absence of cholesterol is due to non-functioning of mce4 operon. mce4 operon consists of various genes that form a part of ABC transporter family and are majorly responsible for cholesterol uptake. This statement was confirmed by the study of Sanaratne et al. which showed that mce4 mutants were unable to grow on medium where cholesterol is the sole carbon source. In addition, cholesterol is not just taken up by M. tuberculosis but also catabolized.
Ramon Garcia et al. confirmed the role of Rv1410c which codes for P55 efflux pump in M. tuberculosis growth in the presence of cholesterol. Another study also proved the interaction of mce4 and mce1 with P55 gene in in-vivo conditions. P55 gene is a part of membrane transporter of major facilitator superfamily (MFS) [24]. This gene mainly benefited the bacterium by maintaining cellular growth of M. tuberculosis, maintaining its intracellular redox balance, etc. This gene was found to be a major culprit with regard to exportation of antibiotics, primarily first-line antibiotics against TB which leads to development of drug-resistant TB. P55 gene is also an important part of P55-lprG operon in which LprG gene encoded by Rv1411c. Rv1410c-lprG deletion mutant had shown attenuated characteristics of M. tuberculosis growth in mice [25].
Despite the advantages of cholesterol, it is required for retention of TACO on M. tuberculosis containing phagosome and due to this retention, only the fusion of phagosome lysosome is blocked [1]. As lipid plays major role in M. tuberculosis infection in different ways thus targeting cholesterol uptake of the bacterium provides us with much greater extent of the treatment. Hence, the above-mentioned information indeed shows that cholesterol is one of the factors which affect the growth of M. tuberculosis and very important role in persistence and virulence of this bacterium.
Genetic regulation of M. tuberculosis cholesterol metabolism
Although it had been said from many decades that cholesterol is essential for mycobacterial survival, infection as well as for persistence, the acquisition, and its utilization mechanism remains poorly described. The majority of studies covers M. tuberculosis and cholesterol as their main topics evidence about the utilization of host cholesterol by bacterium as a source of carbon and energy. First of all uptake of cholesterol require mce4 operon which spans from Rv3492c to Rv3501c in the mycobacterial genome [26]. The bioinformatic analysis employed in several previous studies proved that there are 51 genes out of 82 genes cluster are consistently expressed during growth on cholesterol. One of them is kstR (Rv3574) encodes a tetR like transcriptional repressor and regulate cholesterol metabolism, another gene in the operon is kstR2 (Rv3557c) which is responsible for differential expression of 15 genes (Rv3548-Rv3565) [27]. One of the famous regulatory processes for cholesterol metabolism is betaoxidation and the main enzyme responsible for this is fadA5 which catalyzes thiolysis of acetoacetyl CoA and activity of this enzyme leads to generation of androsterone metabolites required for virulence [28]. One of the recent studies found the essentiality of fad operon (fadD17, fadD19, fadE26, fadE27, and rv04690) in R. rhodococcus cholesterol side-chain degradation [29]. There are other genes also that take part in sterol ring degradation in cholesterol regulation such as Rv1106c and Rv3409c code for a 3β-hydroxysteroid dehydrogenase (3β-HSD) and cholesterol oxidase (ChoD) respectively. These enzymes help in cholesterol metabolism by degrading cholesterol to cholest-4- en-3-one. The other catabolic gene is hsaD is a part of operon that consists of hsaA, hsaC and hsaD which is required for survival of the bacterium inside macrophages is member of α/β Hydrolase family responsible for aromatic compounds degradation [30].
Apart from this genetic regulation, there is a cytochrome p450 system is present in M. tuberculosis that is responsible for major steps for β-oxidation. Saturation of side chains of cholesterol is the necessary step for β-oxidation. Multiple steps have been required to complete the side chain of cholesterol and these steps are as oxidation of cholesterol to alcohol, aldehyde, and acid and all these conversions requires action of cytochrome p450 [31]. Three genes of cytochrome p450 system (CYP125; Rv3545c, CYP142; Rv3518c and CYP124; Rv2266) have been required to complete this function as mentioned in Table 2.
| Functional category | Gene | Mycobacterial homolog | Molecular function |
|---|---|---|---|
| Cholesterol Import | mce4A (Rv3499)* mce4B(Rv3498)# mce4C (Rv3497)# mce4D (Rv3496)# mce4E (Rv3495)# mce4F (Rv3494)# |
M. bovis*# M. leprae* M. smegmatis*# M. marinum*# |
Transport cholesterol across mycolic acid and pseudoperiplasmic space |
| YrbE4 (Rv3501)* YrbE4B (Rv3502)* |
M. bovis* M. leprae* M. smegmatis* M. marinum* |
Transport cholesterol through cytoplasmic membrane | |
| Mam 4A(Rv3493)* Mam4B (Rv3492)* |
M. bovis* M. smegmatis* M. marinum* |
Regulator of mce4 assembly | |
| Degradation by β Oxidation | Cyp 125 (Rv3545)* Cyp142 (Rv3518)* |
M. bovis* M. smegmatis* M. marinum* |
Hydroxylation of terminal C of cholesterol |
| FadD19 (Rv3515)* FadA5 (Rv3546)# |
M. bovis*# M. leprae* M. smegmatis*# M. marinum*# |
Add CoA to the side chain | |
| ChsE4(Rv3504)* ChsE3 (Rv3572)* ChsE1 (Rv3543)# ChsE2 (Rv3544)& |
M. bovis*#& M. leprae* M. smegmatis*#& M. marinum*# |
component of multimeric acyl-CoA dehydrogenase complex | |
| Ltp2 (Rv3505)* | M. bovis* M. leprae* M. smegmatis* M. marinum* |
Work as an aldolase enzyme and cleave C-C bond | |
| Degradation of A and B ring | KstD (Rv3537)& KshA (Rv3526)# KshB (Rv3571)* hsaB (Rv3567)# |
M. bovis*#& M. leprae* M. smegmatis&#* M. marinum#* |
Degrades side chains A and B ring |
| Degradation of C and D ring | FadD3 (Rv3561)$ IpdA (Rv3551)# IpdB (Rv3552)# FadA6 (Rv3556)# |
M. bovis$# M. smegmatis# M. marinum$# |
Degrades side chains C and D ring |
Table 2: Genes involved in regulation of cholesterol metabolism in M. tuberculosis.
Designing of nano bio-particle to target M. tuberculosis H37Rv
The concept of using nanoparticle is adequate and much benefited as it makes a drug to target at the site of infection, with least or minimal side effects and a quicker way to act upon the bacteria. It acts as a selfdriving vehicle to release or unload the drugs to specifically target site. Delivery of drugs with nanoparticles could be advantageous in form of giving temporal and target-dependent transportation of drugs. These nanoparticles comprises of relatively large surface area to volume ratio which makes it feasible to make contact with intracellular parts either through the surface or internally. Nanoparticles in the field of medicine could be used in form of nanocarriers, polymer therapeutics and Solid Drug Nanoparticle (SDN). Nanocarrier could be used as transporters for drug candidates that are either encapsulated inside or attached to surface by strong covalent interactions. The most famous nanocarriers are lipid nanoparticle that provides colloidal stability to the encapsulated hydrophilic drug. Polymer therapeutics is conjugate compound of polymer and drug which releases the drug upon interaction with the target site. This type of nanoparticle could provide physiological distribution as it could be made specified to specific cells. This specific transport could be possible by designing nanoparticle with specific type of biomarkers that only recognizes paratope present on antigen surface or it can also make pHresponsive element that only activates and release drug at low pH. Solid drug nanoparticle on the other side is the drug itself with modified surface adsorbed material. This is the simplest form of nanoparticles that comprises large surface area to volume ratio thus provides greater extent to expose drugs in comparison to non-formulated native drugs [32].
There is a different class of biodegradable nanoparticles that have been discovered till date such as Poly-d,l-lactide-co-glycolide (PLGA), poly-lactic acid (PLA), Poly-ɛ-caprolactone (PCL), Chitosan, gelatin, etc. The nanoparticle surface should be designed in such a way so that it functionalized only on the confluence of infected alveolar macrophage cells infected with M. tuberculosis and treat only infected cells without any harm to its neighboring parts. This could be possible by designing nanoparticles with D-mannose at optimum concentrations and put the whole mixture for agitation. This procedure thus helps in the targeted delivery of drugs only to the M. tuberculosis cell as bacterium express mannose receptors on their surface [1].
Loading of the nanoparticle with first-line drugs would be a better way to treat the infection at primary level. There are several medications had been developed to cure this malady such as isoniazid (INH), rifampicin (RIF), pyrazinamide (PZA), ethambutol (ETM), bedaquiline, capreomycin, delamanid, kanamycin etc. There are other drugs that are used to treat drug-resistant tuberculosis as well, Table 1 enlists all drugs that have used to treat TB at different stages [33-40].
Advancement to target cholesterol metabolism by nanoparticle
After completion of organization of the desired vehicle, it is loaded with the required arms and weapons to attack the pathogenic strain but still modifications and advancement will be required as we know M. tuberculosis is a notorious bacteria it mutates itself according to the stresses. We need to introduce the concept of dosage, time-dependent manner of drug delivery and path of administration are three aspects that are very much important. We know that drugs or steroids work best at some optimal level beyond that or below it, their efficiency decreases significantly. Time-dependent manner of drug delivery is very important and different from dosage because we intend to maintain/exhibit the constant stress created by previous doses of drugs and another important factor would be that how much time then would be taken by our nanoparticle to degrade. Temporal dependent regulation also helps other uninfected cells to get sudden and frequent harm from large amounts of drugs. After setting all above parameters, the nanoparticle loaded with drug might target M. tuberculosis cell and inhibit cholesterol uptake as well as its metabolism which ultimately leads to intoxication due to cholesterol metabolites (Figure 2).
Figure 2: Treatment by anti-cholesterol drug encapsulated nanoparticle: After infection into the host cell, M. tuberculosis reside into alveolar macrophage. (a): M. tuberculosis utilizes host cholesterol for attachment and entry into the macrophages; (b): A bacillus has the advantage to replicate inside macrophage without any interference of the host immune system; (c): Mannosylated or specific biomarker coated nanoparticle target infected macrophage and can hinder with the metabolism of cholesterol by inhibiting various enzymes of cholesterol metabolic pathway; (d): Non degradation of cholesterol metabolism could lead to accumulation of toxic metabolic intermediate which can lead to bacterial death and apoptosis.
Fibrates are the other alternatives that can be used because M. tuberculosis body structure contains a layer of lipids and fatty acids below mycolic acid where fibrates could provide vulnerable stress to the pathogenic bacteria and might degrade the primary level defense mechanism of M. tuberculosis. With the help of first-line defense drugs and fibrates, M. tuberculosis is exposed to sudden stresses and it thus reduces the cholesterol uptake by M. tuberculosis by the help of econazole which acts as the carbon source and helps in growth and proliferation of bacteria. The dosage of aimed medicine should fall short of the multiplication time of M. tuberculosis so that it doesn’t give time to bacteria to multiply and develop any kind of resistance to the medicine. The path of administration or drug delivery should be nasal (which can be inhaled from mouth or nose) as we aim to target the alveolar sac where the macrophage cells hold up the pathogenic strain. In this section the selection of nanoparticle matters the structure and designing plays a very important role as we aim our drug to be inhaled through nasal cavity according to which chitosan, PLGA proves to be the best nanoparticles [41]. Cyclic adenosine monophosphate (cAMP) on the other side, also inhibits mycobacterial cholesterol metabolism by inhibiting initiation steps of its degradation pathway and therefore prohibits bacterial replication inside macrophages [42]. But the main focus is to target cholesterol uptake and its metabolism in the M. tuberculosis cell. Econazole, LP10 azasteroids, etc. are some of the dugs that act upon cholesterol metabolism by interfering with cytochrome P450, cyp125 and sterol biosynthesis respectively enlisted in Table 3 [43]. After selection of drugs to be loaded in the nanoparticle, the next step would be to regulate dosage and temporal modification which is possible by maintaining the thickness of outer layer of nanoparticle so that it releases small amount of drugs at regular interval of time and thus leads to less cytotoxicity and harm to the other cells [32].
| S.No. | Anti-Cholesterol Drug | Target | Reference |
|---|---|---|---|
| 1. | Azasteroids | Inhibit 3β HSD enzyme that catalyzes conversion of cholesterol to 4-en-3-one | 34 |
| 2. | Clotrimazole and econazole | Bind with CYP450s and inhibit its function | 35 |
| 3. | 3β-hydroxysterol-(25R)- cholest-5-en-3β,16β,26-triol |
Inhibit alkylation of cholesterol side chain | 36 |
| 4. | V-13-011503 and V-13-012725 | Inhibit the function of HsaAB that converts 3-HAS to 3,4-DHSA (3,4-dihydroxy-9,10-seconandrost-1,3,5(10)-triene-9,17-dione) in the catabolism of the A/B rings of cholesterol | 37 |
| 5. | 3-chlorocatechol | Inhibitor of extradiol dioxygenase | 38 |
| 6. | Phenylmethylsulfonyl fluoride and 3,4-dichloroisocoumarin | Modify the function of HsaD which catalyzes the hydrolysis of C-C bond | 39 |
| 7. | 20,60-dichloro-DHB and 4-chloro-3-dihydroxy-6- methyl-7,8-dihydro-10-Cl-stilbene |
Inactivates HsaC Which is type I iron-dependent extradiol dioxygenase that cleaves 2,3-dihydroxybiphenyl(2,3-DHB) | 40 |
Table 3: Anti-cholesterol drugs.
What else could be considered on the multidrug-resistant strain of M. tuberculosis?
Although we have tried to limit our approach till inhibiting cholesterol uptake and metabolism but there are other factors also that add in the virulence of this bacterium. Those factors are lipid content of the cell wall, vitamin D3, retinoic acid, retention of Tryptophan aspartate containing coat protein (TACO) protein, dormancy, and persistence within host macrophage, the protection against oxidative radicals, etc.
Optimum translocation of Lipoarabinomannan (LAM) into the cell wall is an essential feature in comprising mycobacterial stability. In addition to increasing stability, LAM also participates in the arresting of phagosome maturation by immature rab5 marker that also marks intracellular survival of the bacterium. It also triggers response of cytokines upon infection. Lipomannan is another constituent lipid of mycobacterial cell wall that is responsible for innate immune response against pathogens also important for virulence.
Trehlose-6, 6’-dimycolate (TDM) is another important part of virulence that is known as cord factor is the most abundant and toxic lipid in the mycobacterial cell wall envelope. It is comprised of two trehalose head groups and esterified mycolic acid molecule. This lipidomic content variation is the major determinant of inflammatory response. In spite of being functional to generate inflammatory responses, this molecule also responsible for inhibiting acidification of phagolysosomes, inhibit calcium-dependent fusion of phagosomelysosome that is the main feature for killing of pathogen within the initial phase of infection. Phthiocerol dimycocerosate (PDIM) and phenolic glycolipid (PGL) are lipids that are responsible for duplication of bacterial cells. PDIM is also involved in mycobacterial resistance to detergent and also protect bacterium against reactive nitrogen and oxygen species.
Although the lipid profile of M. tuberculosis is the main focus for drug development there are other branches also which are important for maintaining the intactness of the bacilli. One of them is the secretory transportation system employed by M. tuberculosis. Studies prove that twin-arginine transporter system (TAT) is an important translocator responsible for transportation of folded proteins to its destined location. M. smegmatis that is deficient in tatA and tatC are unable to grow on agar medium, defective against beta-lactamases and show a hypersensitive pattern for Sodium Dodecyl Sulfate (SDS). Excretory system (ESX) is the major secretory system composed of several proteins that reside in the mycobacterial cytoplasmic membrane and carrying the exportation of cytoplasmic molecules to the extracellular surroundings. These proteins are the major culprit in causing drug-resistant TB [44,45].
M. tuberculosis is the reason behind approx 1.5 million lives for each subsequent year, making it the main source of mortality from prominent bacterial infections. M. tuberculosis is almost constrained in among 33% of the total population, 90% of whom show symptom less inactive diseases that speak to a subclinical or latent pool of pathogenic M. tuberculosis strain and convoluted tuberculosis (TB) control methodologies [46]. The prevalence of TB is expected to a limited extent to this capacity to set up unending disease, alongside the deficiency of present treatments [47]. The WHO has proclaimed TB a worldwide threat and declared emergency against it. The basic fundamental aspect behind its residence in host cellular environment is dependent on inability of the host immune system to rescue themselves and inhibition of the biogenesis of phagosome lysosome complex known as phagolysosomes.
Cholesterol has a significant perspective on the infectivity and pathogenicity of M. tuberculosis. Host cholesterol has been appeared to encourage the survival of mycobacteria into macrophages [48]. Moreover, M. tuberculosis is able to utilize cholesterol as a carbon source. The cholesterol metabolism pathway in mycobacteria has been proposed in view of the assurance of the qualities associated with cholesterol catabolism in the Rhodococcus species. The majority of these qualities in M. tuberculosis have been observed to be under the influence of kstR regulons, which encode a TetR-like transcriptional repressor [49,50]. A few qualities in the kstR cholesterol regulons are incited in macrophages or are basic for disease, accentuating the job of cholesterol catabolism in intracellular survival.
This implausible width of multiplicity among different nanoparticle purposes has been established successfully for an extensive range of treatments, including multiple cancer chemotherapies, ARVs, and even suntan lotion. For the perspective of TB, it already grants considerable improvement; amongst which the many advantages are as increased carrier capacity, reduced degradation in the bowels, improved stability, lesser cytotoxicity and the ability to cater to both a hydrophobic and hydrophilic environment [51,52].
It can provide both sustained and targeted drug delivery and could deliver drugs either to plasma of blood or to the particular organ tissue. In this way, this mechanism gains success to establish direct contact between the pathogen and drug and no other part will be affected. Therefore it is of great advantage over commercial drug and normal drug delivery medication. Although we only emphasize to target cholesterol metabolism of M. tuberculosis by several anticholesterol medications, there are many other aspects that could be and should be targeted by this nanoparticle approach to obtain a successful and better way achievement in the way of eradication of TB [53-55].
One of the important targets to achieve this treatment is to target the vitamin D system of M. tuberculosis as it had been proved that it is one of the major pathways running in this pathogenic bacterium. Retinoic acid and vitamin D3 are also important in downregulating the growth and survival of M. tuberculosis. Vitamin A and vitamin D are major vitamins that have involved in protection of host against infection. Earlier studies show that retinoic acid and vitamin D3 together suppress the expression of TACO protein in a dosedependent manner which therefore also can halt mycobacterial entry to the host cell [45]. Transportation of accessory retinoic acid and vitamin D3 along with nanoparticles could be beneficial to suppress the survival of M. tuberculosis. By now we know that M. tuberculosis is highly aerobic bacteria so we can develop a drug or by the help of nanoparticle we can take away the free oxygen molecules which are needed by M. tuberculosis in order to survive. We intend to make our drugs more specific to target the pathogenic strain which is least harmful to the body and is more effective against the pathogen and treat the disease in as much less time as possible. This methodology of targeting the cholesterol utilizing arm of the bacterium which is the major carbon source will definitely raise an effective anti TB drug. This is because inhibition or hindrance in this pathway would lead to accumulation of toxic metabolites that ultimately lead to bacterial death. So studying in this direction would absolutely a beneficial side for social benefit in terms of getting rid of this disease.
Discussion
Drug delivery is a major concern in case of tuberculosis due to the persistent nature of the bacterium inside granuloma without even any information to host immune system. TB is a global disease caused by the bacteria M. tuberculosis. The genome of M. tuberculosis is studied up to a great extent but still there are some complexities which are needed to be understood as it shows number of variations from normal pathways on exposure to different drugs and steroids and the resistant nature of the bacterium [56-58]. Mycobacterium when residing in the granuloma in host utilizes host cholesterol as their nutrient and main lipid content. Cholesterol, therefore, is one of the major reasons behind this malady because it maintains its growth inside the granuloma.
Conclusion
This review emphasizes the importance of cholesterol in mycobacterial survival and growth and nanoparticle-mediated delivery of anti-cholesterol drugs to cease the uptake and utilization of host cholesterol by M. tuberculosis. Anti-cholesterol drugs would be loaded onto a nanoparticle which would be designed with specific mannose biomarkers that specifically traverses through host inhalatory system to reach alveolar macrophage containing bacilli. Target specific delivery is beneficial in several manners as in lower dosage, lesser cytotoxicity, and effective treatment.
Acknowledgement
The authors acknowledge financial support from the Department of Science and Technology-SERB, Council of Scientific and Industrial Research-Institute of Genomics and Integrative Biology under the research project GAP0145.
References
- Meena LS, Rajni (2010) Survival mechanisms of pathogenic M. tuberculosis H37Rv. FEBS J 277: 2416-2427.
- Timmins GS, Deretic V (2006) Mechanisms of action of isoniazid. Mol Microbiol 62: 1220-1227.
- Wehrli W (1983) Rifampin: mechanisms of action and resistance. Rev Infect Dis 3: 407-411.
- Forbes M, Kuck NA, Peets EA (1962) Mode of action of ethambutol. J Bacteriol 84: 1099-1103.
- Zhang Y, Wade MM (2003) Mode of action of pyrazinamide: disruption of Mycobacterium tuberculosis membrane transport and energetics by pyrazinoic acid. J Antimicrob Chemother 52: 790-795.
- Antwi S, Yang H, Enimil (2017) A Pharmacokinetics of the first-line antituberculosis drugs in Ghanaian children with tuberculosis with or without HIV coinfection. Antimicrob Agents Chemother 61: 1701-1716.
- Deoghare S (2013) Bedaquiline: a new drug approved for treatment of multidrug-resistant tuberculosis. Ind J Pharma 45: 536-537.
- Bastian I, Rigouts L, Palomino JC (2001) Kanamycin susceptibility testing of Mycobacterium tuberculosis using Mycobacterium growth indicator tube and a colorimetric method. Antimicrob Agents Chemother 45: 1934-1936.
- Noel GJ (2009) A review of levofloxacin for the treatment of bacterial infections. Clin Med Therapeut 1: 433-458.
- Zheng J, Rubin EJ, Bifani P (2013) Para-aminosalicylic acid is a prodrug targeting dihydrofolate reductase in Mycobacterium tuberculosis. J Biol Chem288: 23447-23456.
- Xavier AS, Lakshmanan M (2014) Delamanid: A new armor in combating drug-resistant tuberculosis. J Pharmacol Pharmacotherapeut 5: 222-224.
- Lechartier B, Cole ST (2015) Mode of action of clofazimine and combination therapy with benzothiazinones against Mycobacterium tuberculosis. Antimicrob Agents Chemother 59: 4457-4463.
- Hoagland DT (2016) New agents for the treatment of drug-resistant Mycobacterium tuberculosis. Adv Drug Del Rev 102: 55-72.
- Sonal S, Munsiff C (2006) Rifapentine for the treatment of pulmonary tuberculosis. Cli Infect Dis 43: 1468-1475.
- Wiseman LR, Wagstaff AJ (1995) Meropenem. A review of its antibacterial activity, pharmacokinetic properties and clinical efficacy. Drugs 50: 73-101.
- World Health Organization (2018) Global tuberculosis report
- Madhukar P, Behr MA, Dowdy D(2016) Tuberculosis. Nat Rev 2: 16076.
- Fieweger RA, Wilburn KM, Vander VBC (2019) Comparing the metabolic capabilities of bacteria in the Mycobacterium tuberculosis complex. Microorg 18: 7.
- Pedro TG (2018) Potential effect of statins on Mycobacterium tuberculosis infection
- De CP, Fischer SM, Marrero J (2010) Metabolomics of Mycobacterium tuberculosis reveals compartmentalized co-catabolism of carbon substrates. Chem Biol 17: 1122-1131.
- Russell DG, Vander VC, Lee W (2010) Mycobacterium tuberculosis wears what it eats. Cell Host Microbe 8: 68-76.
- Senaratne RH, Sidders B, Sequeira P (2008) Mycobacterium tuberculosis strains disrupted in MCE3 and MCE4 operons is attenuated in mice. J Med Microbiol 57: 164-170.
- Mali PC, Meena LS (2018) Triacylglycerol: nourishing molecule in endurance of Mycobacterium tuberculosis. J Biosci 43: 149.
- Ramon GS (2015) The mycobacterial P55 efflux pump is required for optimal growth on cholesterol. Virulence 6: 444-448.
- Joshi SM, Pandey AK, Capite N (2006) Characterization of mycobacterial virulence genes through genetic interaction mapping. Proc Natl Acad Sci 103: 11760-11765.
- Pandey AK, Sassetti CM (2008) Mycobacterial persistence requires the utilization of host cholesterol. Proc Natl Acad Sci USA 105: 4376-4380.
- Kendall SL (2007) A highly conserved transcriptional repressor controls a large regulon involved in lipid degradation in Mycobacterium smegmatis and Mycobacterium tuberculosis. Mol Microbiol 65: 684-699.
- Kendall SL (2010) Cholesterol utilization in Mycobacteria is controlled by two TetR-type transcriptional regulators: kstR and kstR2. Microbiol 156: 1362-1371.
- Brzostek A (2009) Mycobacterium tuberculosis is able to accumulate and utilize cholesterol. J Bacteriol 191: 6584-6591.
- Wilbrink MH (2011) FadD19 of Rhodococcus rhodochrous DSM43269, a steroid-coenzyme a ligase essential for degradation of C-24 branched sterol side chains. Appl Environ Microbiol 77: 4455-4464.
- Yang X (2007) Rv1106c from Mycobacterium tuberculosis is a 3beta-hydroxysteroid dehydrogenase. Biochem 46: 9058-9067.
- Samantha D, Marco G (2019) Nanomedicines towards targeting intracellular MTb for the treatment of tuberculosis. J Interdiscipli Nanomed 4: 76-85.
- Ouellet H, Johnston JB, Montellano PR (2011) Cholesterol catabolism as a therapeutic target in Mycobacterium tuberculosis. Trends Microbiol 19: 530-539.
- Thomas ST, Yang X, Sampson NS (2011) Inhibition of the M. tuberculosis 3β-hydroxysteroid dehydrogenase by azasteroids. Bioorg Med Chem Lett 21: 2216-2219.
- McLean KJ, Munro AW (2008) Structural biology and biochemistry of cytochrome P450 systems in Mycobacterium tuberculosis. Drug Metab Rev 40: 427-446.
- Schmidt AW, Choi TA, Theumer G (2013) Inhibitory effect of oxygenated cholestan-3β-ol derivatives on the growth of Mycobacterium tuberculosis. Bioorg Med Chem Lett 23: 6111-6113.
- Vanderven BC, Fahey RJ, Lee W (2015) Novel inhibitors of cholesterol degradation in Mycobacterium tuberculosis reveal how the bacterium’s metabolism is constrained by the intracellular environment. PLoS Pathog 11: 2.
- Garnier T, Eiglmeier K, Camus JC (2003) The complete genome sequence of Mycobacterium bovis. Proc Natl Acad Sci 100: 7877-7882.
- Ryan A, Keany S, Eleftheriadou O (2014) Mechanism-based inhibition of HsaD: a CC bond hydrolase essential for survival of Mycobacterium tuberculosis in macrophage. FEMS Microbiol Lett 350: 42-47.
- Yams KC, D’Angelo I, Kalscheuer R (2009) Studies of a ring-cleaving dioxygenase illuminate the role of cholesterol metabolism in the pathogenesis of Mycobacterium tuberculosis. PLoS Path 5: e1000344.
- Shivangi, Meena LS (2018) A novel approach in treatment of tuberculosis by targeting drugs to infected macrophages using biodegradable nanoparticles. Appl Biochem Biotechnol 185: 815-821.
- Areej A (2017) Cholesterol metabolism: a potential therapeutic target in Mycobacteria. Br J Pharmacol 174: 2194-2208.
- Kaley M, Rachael A, Brian C (2018) Cholesterol and fatty acids grease the wheels of Mycobacterium tuberculosis pathogenesis. Pathogen Dis 1: 76.
- Gabriela EV, Susana FV, Clara I (2017) Virulence factors and pathogenicity of Mycobacterium.
- Bisht D, Meena LS (2016) A part of intracellular life of Mycobacterium. Mycobact Dis 6: 220.
- VanderVen BC, Fahey RJ, Lee Y (2015) Novel inhibitors of cholesterol degradation in Mycobacterium tuberculosis reveal how the bacterium’s metabolism is constrained by the intracellular environment. PLoS Pathogens 11: e1004679.
- Crowe AM, Stogios PJ, Casabon E (2015) Structural and functional characterization of a ketosteroid transcriptional regulator of Mycobacterium tuberculosis. J Biol Chem 290: 872-882.
- Barrientos AE, Merino I, Casabon J (2015) Functional analyses of three acyl-CoA synthetases involved in bile acid degradation in Pseudomonas putida DOC21. Environ Microbiol 17: 47-63.
- Kendall SL, Withers M, Soffair CN (2007) A highly conserved transcriptional repressor controls a large regulon involved in lipid degradation in Mycobacterium smegmatis and Mycobacterium tuberculosis. Mol Microbiol 65: 684-699.
- Larrouy MG (2015) Cholesterol acquisition by Mycobacterium tuberculosis. Virulence 6: 412-413.
- Russell DG, Vander BC, Lee W (2010) Mycobacterium tuberculosis wears what it eats. Cell Host Microbe 8: 68-76.
- Vander GR, Yam K, Heuser T (2007) A gene cluster encoding cholesterol catabolism in a soil actinomycete provides insight into Mycobacterium tuberculosis survival in macrophages. Proc Natl Acad Sci 104: 1947-1952.
- Pandey R, Zahoor A, Sharma S (2003) Nanoparticle encapsulated antitubercular drugs as a potential oral drug delivery system against murine tuberculosis. Tuberculosis 83: 373-378.
- Pandey R (2004) Subcutaneous nanoparticle-based antitubercular chemotherapy in an experimental model. J Antimicrob Chemother 54: 266.
- Sung JC (2009) Dry powder nitroimidazopyran antibiotic PA-824 aerosol for inhalation. Antimicrob Agents Chemother 53: 1338.
- Verma H, Shivangi, Meena LS (2018)Delivery of antituberculosis drugs to Mycobacterium tuberculosis H37Rv infected macrophages via polylactide-co-glycolide (PLGA) nanoparticles.Int J Mol Biol Open Access 3: 235-238.
- Meena, LS (2019) Interactions of mesoporous silica and Zno nanoparticles with Escherichia coli. Adv Biotech Microbio 12.
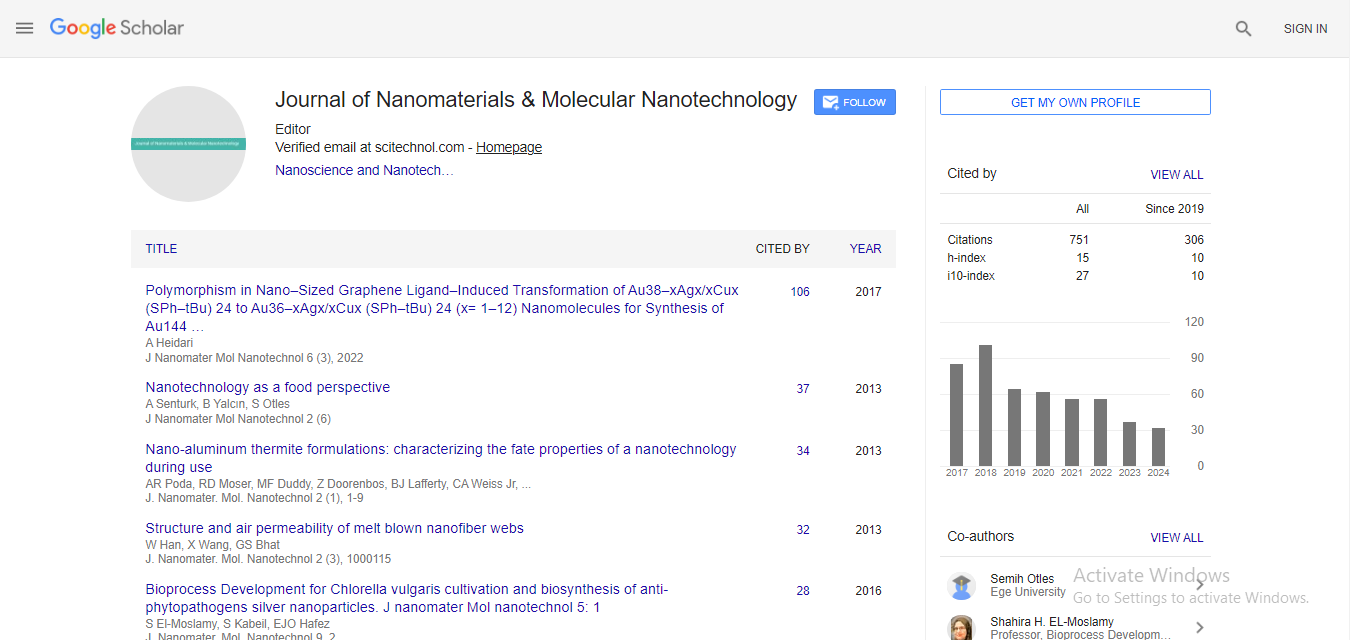
- Meena J, Singh M, Sahare PD (2014) Interaction of nanoparticles in biological systems and their role in therapeutical treatment of tuberculosis and cancer. J Lumin 1: 7-22.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi