Research Article, J Sleep Disor Treat Care Vol: 6 Issue: 4
Cephalometric and Dental Measures as Diagnostic Tools for the Obstructive Sleep Apnea
Scannone A, Tosta M, Suarez A and Otero L*
DDS, Pontificia Universidad Javeriana, Colombia
*Corresponding Author : Liliana Otero M, PhD
Faculty of Dentistry, Pontificia Universidad Javeriana, Cra. 7a No 40-62. Piso 4, Bogota, Colombia
Tel: (57-1)3208320 Ext. 2899
E-mail: lotero@javeriana.edu.co
Received: June 08, 2017 Accepted: June 20, 2017 Published: June 28, 2017
Citation: Scannone A, Tosta M, Suarez A, Otero L (2017) Cephalometric and Dental Measures as Diagnostic Tools for the Obstructive Sleep Apnea. J Sleep Disord: Treat Care 6:4. doi: 10.4172/2325-9639.1000202
Abstract
Background: Obstructive Sleep Apnea (OSA) is a breathing disorder that could be associated with craniofacial and dental phenotype. Objective: To identify features of craniofacial and dental phenotype associated with high suspicion of OSA in adults.
Methods: Lateral X-ray and dental casts were acquired from 126 adults (77 females and 49 males). Sleep Questionnaires were applied to identify high suspicion of OSA. Questionnaires answers for each subject were correlated with cephalometric and dental cast measures.
Results: Suspicion of OSA was observed in 47.6% of the individuals. Bivariate analysis showed that patients with class II malocclusion have more probability to present OSA (OR=2.5; CI: 1.11 - 6.19; p=0.048) while skeletal class I patients having a 60% less chance of presenting suspicion of OSA (OR=0.4; CI: 0.14-1.07; p=0.045).
Conclusions: These findings suggest association between Class II malocclusion and suspicion of OSA. Nevertheless, further research is needed to determine which craniofacial and dental phenotypic features contribute to the development of OSA.
Keywords: Obstructive sleep apnea; Cephalometry; Class II malocclusion
Introduction
Obstructive Sleep Apnea (OSA) is a breathing disorder characterized by the increased resistance of the airways during sleep, leading to episodes of partial (hypopnea) or complete (apnea) collapse of breathing [1,2]. These episodes lead to diminishing of the intrathoracic pressure, blood oxygen desaturation, and sleep fragmentation, resulting in depression, fatigue, irritability and daytime sleepiness [3]. Previous studies have shown that OSA has a bidirectional association among diseases such as arterial hypertension, heart disease, and cerebrovascular events [4], which generate high levels of mortality in the world, reasons for which OSA is considered a major public health problem.
The prevalence of OSA depends on factors such as gender and ethnicity. OSA prevalence in adults varies between 14.7% and 34.2% but it is considered that approximately 82% of women and 93% of men with OSA are still undiagnosed [5,6]. OSA in adults is a multifactorial disorder resulting from the interrelation of factors such as skeletal malformations, collapse of upper airways, age, obesity, gender and genetics [7,8]. The clinical methods that guide to the diagnosis of OSA including sleep questionnaires and skull radiography, but he polysomnography (PSG) or "Sleep Study" is considered the gold standard test. The skull radiography and cephalometric analysis emerge as a complementary tool for the diagnosis of OSA. Cephalometric analysis identifies craniofacial features predisposing to OSA with sensitivity of 93% and a specificity of 21% [9].
Some craniofacial features and upper airways size are predisposing factors for airway collapse during sleep, reasons for which their proper evaluation and diagnosis are essential in preventing the development of sleep disorders. Craniofacial features such as skeletal malocclusions, mandibular retrognathism, mandibular micrognathia, lower position of hyoid bone to mandibular plane and maxilla micrognathism lead to the upper airways diminishing, increasing the risk of developing OSA [10,11]. The size of the upper airways is frequently associated with Class II skeletal patterns including mandibular retrognathism and maxilla micrognathism [12]. Maxilla micrognathia could be transverse and sagittal and it seems that transverse maxillary micrognathia increases the resistance of the upper airway, triggering mixed or oral breathing, but the role of micrognathia in the etiology of OSA has not been clarified yet.
Another important finding related to the OSA pathophysiology and the presence of craniofacial alterations is the hyoid bone position. It seems that the accumulation of fat in the pharyngeal regions produce anterior and inferior position of the hyoid bone, causing a descent of tongue and a consequent reduction of the upper airway. It has been reported that inferior hyoid bone position is observed in patients with OSA [13].
The objective of the present study was to identify craniofacial and dental features associated with high suspicion of Obstructive Sleep Apnea sleep in adults.
Methods
Lateral radiography of skull and dental cast models were taken in 126 individuals between 18 years old (77 women and 49 men). The skeletal analysis by cephalometry in these individuals showed 30 individuals with Class I malocclusion, 62 with Class II malocclusion and 33 with Class III malocclusion. Individuals with history of maxillofacial surgery, syndromes and cleft lip and palate were excluded. This research was approved by ethical committee of Medicine Faculty at Pontificia Universidad Javeriana. All participants signed consent form.
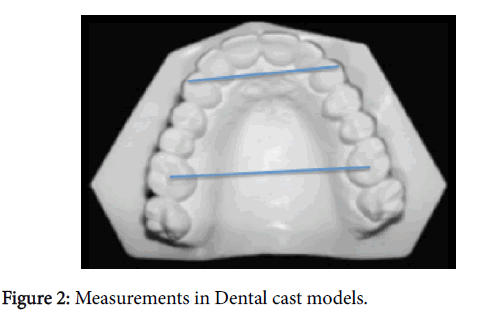
Sleep questionnaires including Berlin, Pittsburgh, Epworth and STOP BANG were applied in each participant. The results of questionnaires were subsequently correlated with the findings obtained in the cephalometric analysis in order to determine the possible relationship between craniofacial features and the high suspicion of OSA. Cephalometric measurements and description were shown in Figure 1. Measurements of dental cast models were taken to identify transverse maxillary micrognathia (Figure 2).
Kappa Statistical Test for concordance between two experts who performed cephalomentric analysis and dental cast measures. Chi square and Fisher Tests were used for the qualitative measures, and TStudent or U-Mann-Whitney Tests for quantitative variables according to the normal variables distribution previously established with the Kolmogorov-Smirnov Test.
For evaluating the relationship of cephalometric features presenting the chance of suspected OSA, a bivariate analysis was performed, where the ORs (Odds Ratios) was calculated with confidence interval of 95% and p<0.05. The statistical software used for the analysis was the STATA version 13.0 for Mac (Table 1).
| Measure | Abbreviation | Definition |
|---|---|---|
| Convexity Angle | Gl-Sn-Pg | Angle formed by the points GI- Sn and Sn-Pg |
| Maxillomandibular Difference | ANB | Difference between the SNA and SNB angles |
| Maxillary Effective length | Co-A (mm) | Distance in mm from the condyle’s extreme posterior upper part to point A |
| Mandibular Effective Length | Co-Gn (mm) | Distance in mm from the condyle’s extreme posterior upper part to point Gn |
| Upper Maxillary Length | ENA-ENP (mm) | Distance in mm from the posterior nasal spine to the anterior nasal spine |
| Maxillary Antero-Posterior Position | A-N (mm) | Distance in mm from a Frankfurt’s perpendicular plane passing through the Nasion point to point A |
| Mandibular Antero-Posterior Position | Pg-N (mm) | Distance in mm from a Frankfurt’s perpendicular plane passing through the Nasion point to point Pg |
| Upper Pharyngeal Space | UFS (mm) | Distance in mm measured from the soft palate and pharyngeal posterior part throughout a line parallel to plane Go-B passing through the soft palate’s most posterior and superior point |
| Inferior Pharyngeal Space | IFS (mm) | Distance in mm from the soft palate and pharyngeal posterior wall throughout the Go-B line |
| Distance from Hyoid Bone to Mandibular Plane | HPM (mm) | Distance in mm from the hyoid bone’s most anterior-superior palate and mandibular plane |
| Distance from Hyoid Bone to C3 | HC3 (mm) | Distance in mm measured from the hyoid bone’s most anterior superior part and the third cervical vertebra’s most anterior inferior point |
Table 1: Cephalometric measurements description.
Results
126 patients were included in the study; 47.6% (n=60) of the sample had suspected OSA; the average age was 26 years old. The gender distribution was similar in both groups, mostly female at a rate of 53.3% (n=32) patients with suspected OSA and 68.2% (n=45) without suspicion of OSA.
The distribution of skeletal and dental measurements and their association with OSA is shown in Table 2.
| Variable | High suspicion OSA n = 66 | Non OSA n = 60 | Total n = 126 | Statistical Test | P Value | |||
|---|---|---|---|---|---|---|---|---|
| Age, average | 25.5 | [20-38] | 28.5 | [21-37] | 26 | [21-37] | Mann-Whitney | 0.409 |
| Gender, n (%) | ||||||||
| Male | 20 | (31.8) | 28 | (46.7) | 49 | (38.9) | Chi2 | 0.088 |
| Female | 45 | (68.2) | 32 | (53.3) | 77 | (61.1) | ||
| Profile, n (%) | ||||||||
| Straight | 28 | (42.4) | 19 | (31.7) | 47 | (37.3) | ||
| Concave | 18 | (27.3) | 18 | (30.0) | 36 | (28.6) | Chi2 | 0.438 |
| Convex | 20 | (30.3) | 23 | (38.3) | 43 | (34.1) | ||
| Skeletal Class, n (%) | ||||||||
| Class I | 20 | (30.3) | 10 | (16.7) | 30 | (23.8) | ||
| Class II | 28 | (42.2) | 35 | (58.3) | 63 | (50.0) | Chi2 | 0.128 |
| Class III | 18 | (27.3) | 15 | (25.0) | 33 | (26.2) | ||
| Effective maxillary length, n (%) | ||||||||
| Average | 9 | (13.6) | 13 | (21.7) | 22 | (17.5) | Chi2 | 0.236 |
| Diminished | 57 | (86.4) | 47 | (78.3) | 104 | (82.5) | ||
| Increased | 0 | (0) | 0 | (0) | 0 | (0) | ||
| Mandibular effective length, n (%) | ||||||||
| Average | 13 | (19.7) | 15 | (25) | 28 | (22.2) | ||
| Diminished | 50 | (75.7) | 44 | (73.3) | 94 | (74.6) | Fisher | 0.638 |
| Increased | 3 | (4.6) | 1 | (1.7) | 4 | (3.2) | ||
| Maxillar length, n (%) | ||||||||
| Average | 27 | (40.9) | 24 | (40) | 51 | (40.5) | ||
| Diminished | 37 | (56.1) | 32 | (53.3) | 69 | (54.8) | Fisher | 0.656 |
| Increased | 2 | (3) | 4 | (6.7) | 6 | (4.7) | ||
| A-N upper maxillary length, n (%) | ||||||||
| Normal | 26 | (39.4) | 18 | (30) | 44 | (34.9) | ||
| Prognathism | 13 | (19.7) | 11 | (18.3) | 24 | (19.1) | Chi2 | 0.446 |
| Retrognathism | 27 | (40.9) | 31 | (51.7) | 58 | (46) | ||
| Pg-N mandibular position, n (%) | ||||||||
| Average | 30 | (45.5) | 31 | (51.7) | 61 | (48.4) | ||
| Prognathism | 14 | (21.2) | 13 | (21.7) | 27 | (21.4) | Chi2 | 0.699 |
| Retrognathism | 22 | (33.3) | 16 | (26.7) | 38 | (31.2) | ||
| Upper pharynx, n (%) | ||||||||
| Average | 43 | (65.1) | 33 | (55) | 76 | (60.3) | Fisher | 0.204 |
| Diminished | 23 | (34.9) | 25 | (41.7) | 48 | (38.1) | ||
| Increased | 0 | (0) | 2 | (3.3) | 2 | (1.6) | ||
| Lower pharynx, n (%) | ||||||||
| Average | 44 | (66.7) | 40 | (66.7) | 84 | (66.7) | Fisher | 0.126 |
| Diminished | 20 | (30.3) | 13 | (21.7) | 33 | (26.2) | ||
| Increased | 2 | (3) | 7 | (11.7) | 9 | (7.1) | ||
| Hyoid PM, n (%) | ||||||||
| Average | 10 | (15.1) | 9 | (15) | 19 | (15.1) | ||
| Diminished | 53 | (80.3) | 51 | (85) | 104 | (82.5) | Fisher | 0.377 |
| Increased | 3 | (4.6) | 0 | (0) | 3 | (2.4) | ||
| Hyoid C3, n (%) | ||||||||
| Average | 26 | (39.4) | 30 | (50) | 56 | (44.4) | ||
| Diminished | 34 | (51.5) | 22 | (36.7) | 56 | (44.4) | Chi2 | 0.239 |
| Increased | 6 | (9.1) | 8 | (13.3) | 14 | (11.1) | ||
Table 2: Cephalometric features of adults with and without suspicion of OSA.
The bivariate analysis showed no statistically significant difference either for the upper maxillary transverse measures (W intercanine and intermolar) (Table 3) nor for the cephalometric measures and their relationship to suspected OSA, except for the skeletal malocclusion (Table 4). Individuals with Class II malocclusion showed 1.5 times more chance of presenting suspicion of OSA compared to individuals with Class I malocclusion, and this relationship was statistically significant (OR:2.5 CI95%: 1.01 - 6.19; p=0.048); on the contrary, the skeletal class I patients have a 60% less chance of presenting suspicion of OSA (OR: 0.4 IC95%: 0.14-1.07 p=0.045).
| Variable | High suspicion OSA n = 66 | suspicion OSA n = 60 | Non n = 126 | OSA | ORR | OR | P n = 66 | CI n = 60 |
|---|---|---|---|---|---|---|---|---|
| N | % | |||||||
| Intercanine width n (%) | ||||||||
| Average | 11 | (16.9) | 11 | (19.3) | 1 | |||
| Diminished | 21 | (32.3) | 12 | (21.0) | 0.57 | 0.317 | (0.19 - 1.71) | |
| Increased | 33 | (50.8) | 34 | (59.7) | 1.03 | 0.952 | (0.39 - 2.69) | |
| Intermolar width, n (%) | ||||||||
| Average | 9 | (15.2) | 6 | (10.9) | 1 | |||
| Diminished | 24 | (40.7) | 19 | (34.5) | 1.18 | 0.778 | (0.35 - 3.92) | |
| Increased | 26 | (44.1) | 30 | (54.6) | 1.73 | 0.354 | (0.54 - 5.51) | |
Table 3: Bivariate analysis between maxillary transverse measurements and its relationship to suspected OSA.
| Variable | Odds Ratio | IC 95% | Valor p |
|---|---|---|---|
| Gender | |||
| Male | 1 | 0.089 | |
| Female | 0.53 | (0.25 - 1.10) | |
| Profile | |||
| Straight | 1 | ||
| Concave | 1.47 | (0.61 - 3.53) | 0.385 |
| Convex | 1.69 | (0.73 - 3.90) | 0.216 |
| Skeletal class | |||
| Class I | 0.4 | (0.14 - 1.07) | 0.045* |
| Class II | 2.5 | (1.01 - 6.19) | 0.048* |
| Class III | 1.6 | (0.59 - 4.63) | 0.328 |
| Maxillary effective length | |||
| Average | 1 | 0.239 - |
|
| Diminished | 0.57 | (0.22 - 1.45) | |
| Increased | - | - | |
| Mandibular effective length | |||
| Average | 1 | ||
| Diminished | 0.76 | (0.32 - 1.77) | 0.530 |
| Increased | 0.28 | (0.02 - 3.12) | 0.307 |
| Maxillary Length | |||
| Average | 1 | ||
| Diminished | 0.97 | (0.47 - 2.01) | 0.941 |
| Increased | 2.25 | (0.37 - 13.39) | 0.373 |
| Upper Maxillary´s position A-N | |||
| Normal | 1 | ||
| Prognathism | 1.22 | (0.44 - 3.33) | 0.695 |
| Retrognathism | 1.65 | (0.75 - 3.66) | 0.211 |
| Mandibular position Pg-N | |||
| Average | 1 | ||
| Prognathism | 0.89 | (0.36 - 2.22) | 0.817 |
| Retrognathism | 0.70 | (0.31 - 1.59) | 0.399 |
| Upper Pharynx | |||
| Average | 1 | 0.347 | |
| Diminished | 1.41 | (0.68 - 2.92) | |
| Increased | - | - | - |
| Pharynx inferior | |||
| Average | 1 | 0.422 | |
| Diminished | 0.71 | (0.31 - 1.62) | |
| Increased | 3.83 | (0.75 - 19.6) | 0.105 |
| Hyoids PM | |||
| Average | 1 | ||
| Diminished | 1.06 | (0.40 - 2.84) | 0.893 |
| Increased | - | - | - |
| Hyoids C3 | |||
| Average | 1 | ||
| Diminished | 0.56 | (0.26 - 1.18) | 0.131 |
| Increased | 1.15 | (0.35 - 3.76) | 0.810 |
Table 4: Bivariate analysis between the cephalometric features and its relationship to suspected OSA.
Discussion
The results of the present study showed that adults with Class II malocclusion showed 1.5 times more chance of presenting suspicion of OSA when compared with individuals with Class I malocclusion, while patients with Class I had 60% less opportunity to present OSA when compared with patients with Class II skeletal patterns. These results have been previously reported by researching that demonstrated a clear reduction in the airways space in individuals with mandibular retrognathism and OSA [7]. A similar correlation has been reported by Ryu et al. [3] through cephalometric and PSG studies who showed that individuals with OSA had posteroinferior position of hyoid bone and mandibular retrognathism. Mandibular retrusion is frequently in individuals with class II malocclusion and the position of mandible in these individuals can obstruct the pharynx during sleep, increasing chances of developing OSA. Likewise, it has been observed that there is a close relationship between the tongue’s position and hyoid bone position. The literature reports that hyoid bone position impacts the tongue position, and therefore the permeability of the hypopharyngeal airway.
These measurements are related with the increase in the distance from hyoid bone to mandibular plane, as well as the increased distance from hyoid bone to anterior-inferior point of the third cervical vertebra (C3) [13]. Individuals with Class II malocclusions tend to have a lower hyoid bone position, but in our investigation anterior and inferior hyoid bone positions were not associated with high suspicion of OSA. Transverse maxillary micrognathia has been associated with OSA, although the results are not consistent [14,15]. For this reason in the present study we evaluated the intercanine and upper intermolar width measurements in dental cast models, but the results did not show association between these measurements with suspicion of OSA. PSG is an effective test to diagnosis OSA, but the origin of airway obstructions that produce OSA cannot be identified by PSG. Lateral cephalometric radiography is a useful tool to evaluate the airway obstructions in these individuals [16-18]. Further investigations are needed to determine craniofacial phenotypic characteristics that contribute to the development of OSA in adults.
References
- Tsai H, Ho C, Lee P, Tan C (2009) Sex differences in anthropometric and cephalometric characteristics in the severity of obstructive sleep apnea syndrome. Am J Orthod Dentofacial Orthop 135: 155-164.
- Seto BH, Gotsopoulos H, Sims MR, Cistulli PA (2002) Maxillary morphology in obstructive sleep apnoea syndrome. Eur J Orthod 23: 703-714.
- Ryu H, Kim C, Cheon S, Bae W, Kim S, et al. (2015) The usefulness of cephalometric measurement as a diagnostic tool for obstructive sleep apnea syndrome: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol 119: 20-31.
- Costa E Sousa RA, dos Santos Gil NA (2013) Craniofacial skeletal architecture and obstructive sleep apnoea syndrome severity. J Craniomaxillofac Surg 41: 740-746.
- Abrishami A, Khajehdehi A, Chung F (2010) A systematic review of screening questionnaires for obstructive sleep apnea. Can J Anaesth 57: 423-438.
- Canto Gde L, Pachêco-Pereira C, Aydinoz S, Major PW, Flores-Mir C (2015) Biomarkers associated with obstructive sleep apnea: A scoping review. Sleep Med Rev10: 28-45.
- Battagel JM, Johal A (2000) A cephalometric comparison of normal weight and obese subjects with obstructive sleep apnoea. Radiography 11: 283-292.
- Denolf P, Vanderveken OM, Marklund M, Braem MJ (2016) The status of cephalometry in the prediction of non-CPAP treatment outcome in obstructive sleep apnea patients: a literature review. Sleep Med Rev 27: 56-73.
- El H, Palomo JM (2013) An airway study of different maxillary and mandibular sagittal positions. Eur J Orthod 35: 262-270.
- Raffaini M, Pisani C (2013) Clinical and cone-beam computed tomography evaluation of the three-dimensional increase in pharyngeal airway space following maxillo-mandibular rotation-advancement for Class II-correction in patients without sleep apnoea (OSA). J Craniomaxillofac Surg 41: 552-557.
- Chi L, Comyn FL, Mitra N, Reilly MP, Wan F, et al. (2011) Identification of craniofacial risk factors for obstructive sleep apnoea using three-dimensional MRI. Eur Respir J 38: 348-358.
- Dobrowolska-Zarzycka M, Dunin-Wilczynska I, Mitura I, Dabala M (2013) Evaluation of upper airways depth among patients with skeletal Class I and III. Folia Morphol (Warsz) 72: 155-160.
- Gungor AY, Turkkahraman H, Yilmaz HH, Yariktas M (2013) Cephalometric comparison of obstructive sleep apnea patients and healthy controls. Eur J Dent 7: 48-54.
- Cistulli PA, Richards GN, Palmisano RG, Unger G, Berthon-Jones M, (1996) Influence of maxillary constriction on nasal resistance and sleep apnea severity in patients with Marfan's syndrome. Chest 110: 1184-1188.
- Johal A, Conaghan C (2004) Maxillary morphology in obstructive sleep apnea: a cephalometric and model study. Angle Orthod 74: 648-656.
- Perri R, Kairaitis K, Cistulli p (2013) Surface cephalometric and anthropometric variables in OSA patients: statistical models for the OSA phenotype. Sleep Breath 18: 39-52.
- Susarla SM, Abramson ZR, Dodson TB, Kaban LB (2010) Cephalometric Measurement of Upper Airway Length Correlates With the Presence and Severity of Obstructive Sleep Apnea. J Oral Maxillofac Surg 68: 2846-2855.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi