Case Report, J Neurosci Clin Res Vol: 8 Issue: 1
Case of Opsoclonus Myoclonus Ataxia Syndrome with Benign Ovarian Teratoma
Nilesh Chaudhary1* , Anil Venkatachalam1 and Anita Soni2
1Department of Neurology, Dr L H Hiranandani Hospital, Powai, Mumbai, India;
2Department of Obstetrics and Gynaecology, Dr L H Hiranandini Hospital, Powai, Mumbai, India;
*Corresponding Author: Nilesh Chaudhary
Department of Neurology, Dr L
H Hiranandani Hospital, Powai, Mumbai, India;
E-mail: nilmint@gmail.com
Received date: 27 January, 2023, Manuscript No. JNSCR-23-88059;
Editor assigned date: 30 January, 2023, PreQC No. JNSCR-23-88059(PQ);
Reviewed date: 13 February, 2023, QC No. JNSCR-23-88059;
Revised date: 21 April, 2023, Manuscript No. JNSCR-23-88059 (R);
Published date: 28 April, 2023, DOI: 10.4172/JNSCR.1000152
Citation: Chaudhary N, Venkatachalam A, Soni A (2023) Case of Opsoclonus Myoclonus Ataxia Syndrome with Benign Ovarian Teratoma. J Neurosci Clin Res 8:2.
Keywords: Opsoclonus myoclonus ataxia syndrome; Ovarian teratoma; NMDA antibody; Oscillopsia
Introduction
Opsoclonus myoclonus ataxia syndrome is rare aetiology can be infectious, para-infectious, idiopathic, or paraneoplastic. The clinical manifestations of Opsoclonus-Myoclonus Syndrome ataxia (OMS) also named “dancing eyes dancing feet” syndrome due to its unique clinical features [1].
Opsoclonus Myoclonus Syndrome ataxia (OMS) is a rare condition of unknown etiology that manifest with opsoclonus, myoclonic jerks, behavioural disturbances, and ataxia. The leading hypothesis for the cause of OMS is an autoimmune, inflammatory reaction targeting central nervous system tissues, triggered by either a paraneoplastic or an infectious antigen [2-5].
Mechanism for opsoclonus myoclonus ataxia syndrome is disinhibition of oculomotor neurons in caudal fastigial nucleus of cerebellum due to purkinje cell dysfunction and disinhibited burst neurons. Normal saccadic eye movements controlled by burst neurons. Disinhibited burst neurons leads to opsoclonus [6].
In children, the most common age is 1 to 3 years. In adults, the age of presentation can vary widely depending on the etiology, with reports ranging from adolescence to the eighth decade of life [7].
Age of onset in paediatric age group is 1-3 years, but in adult its variable from age of 10 years to 80 years depending on underlying etiology [8]. The ratio of male to female is 3:6, which showing significant female predominance. All cases need prompt paraneoplastic work up especially for ovarian teratoma. If detected early and treated it carries good prognosis main treatment is surgical excision and immunosuppressive therapy. NMDA antibodies may not be detected in all cases [9].
Opsoclonus myoclonus ataxia syndrome due to ovarian teratoma is rare, before 2005 there were only 8 cases reported by Dalmau, et al.
Case Presentation
26 years old nulliparous female presented to outpatient department with progressive imbalance during walking since last 1 week with episodic jerky movements of trunk and upper and lower limbs since last 5 days [10]. Along with imbalance and truncal and appendicular jerky movements from last 2 days she was having episodic irregular jerky eye ball movements causing her oscillopsia is an illusion of an unstable vision, made up of the perception of to-and-fro movement of the environment [11].
No history of fever, headache or seizure in past, no history of weight loss, steatorrhea [12]. On examination, her vitals were normal, on cranial nerve examination opsoclonus was present. Irregular jerky movements including face and upper and lower limbs and trunk suggestive of cortical myoclonus. She was also having appendicular and truncal ataxia [13].
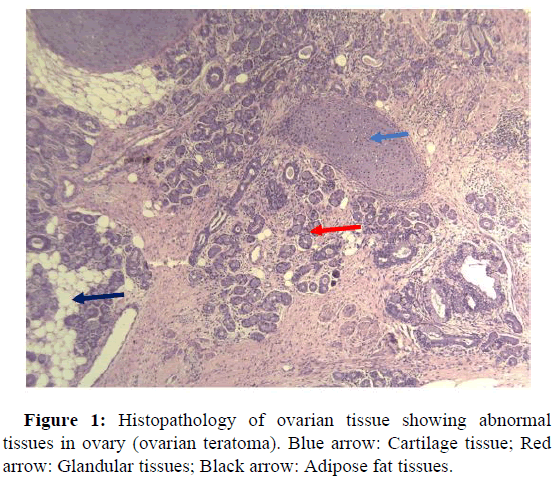
Her MRI brain with contrast was normal, CSF study was normal. Her initial serum NMDA and VGKC antibodies were negative she was started on intravenous immunoglobulins as her symptoms were progressing rapidly [14]. Her whole-body pet scan was suggestive of right ovarian teratoma so urgent gynecological opinion was taken a laparoscopic excision of teratoma is done. Histopathology was suggestive of mature benign teratoma (Figure 1).
She was kept on oral prednisolone 1 mg/kg and started tapering after 3 months, after tapering oral prednisolone she developed again ataxia and opsoclonus which was less severe but was progressive despite of increasing dose of prednisolone. Her opsoclonus was treated with gabapentin [15]. We have done repeat whole-body pet to rule out any residual teratoma which was negative her repeat autoimmune and paraneoplastic panel was showing NMDA antibody positive. She is started on rituximab 1 gm 2 weekly regimen for 2 dosages she has shown significant improvement and we are monitoring her CD 20 regularly [16].
Her CD20 was zero for 3 months, and below normal biological reference for 6 months. She has not received further immunosuppressant or rituximab as primary cause (ovarian teratoma) was tackled with surgical excision. She was followed closely for next 2 years without signs of recurrence. At end of 2 years, she was conceived successfully [17].
Results and Discussion
Opsoclonus Myoclonus Syndrome (OMS) is characterized by the combination of opsoclonus and arrhythmic action myoclonus that predominantly involves trunk and limbs usually associated with axial ataxia and dysarthria [18].
Opsoclonus Myoclonus Syndrome ataxia (OMS) disorder found in paediatric and adult patients. Etiology is either idiopathic (I-OMS) or Paraneoplastic (P-OMS).
Diagnostic criteria for Opsoclonus-Myoclonus Syndrome ataxia (OMS) were defined as requiring three of the four following features;
• Opsoclonus,
• Myoclonus or ataxia,
• Behavioural change or sleep disturbance, and
• Neuroblastoma.
But opsoclonus and myoclonus were two persistent clinical features in both paediatric and adult age groups, other features were variable.
The relapse of OMS was defined as worsening of OMS symptoms lasting for at least 72 h after a period of stability or improvement for at least 30 days, or the escalation of immunotherapy [19].
In age less than 40 years common causes are idiopathic, para infectious and ovarian teratoma and if age more than 40 years paraneoplastic is more likely small cell carcinoma most common followed by carcinoma breast and gynecological cancers.
In the paediatric population, OMS is associated with an underlying diagnosis of neuroblastoma in approximately half of cases [20].
Opsoclonus Myoclonus Syndrome ataxia (OMS) in adults which is not paraneoplastic etiology (idiopathic) mainly due to para and postinfectious particularly with viral infections like influenza, varicella, cytomegalovirus, human herpes virus 6, human immunodeficiency virus, and hepatitis C and dengue virus.
Also, association of Mycoplasma pneumoniae and Salmonella, Streptococcus with Opsoclonus-Myoclonus Syndrome ataxia is described (OMS). All patient presenting with opsoclonus, myoclonus, ataxia syndrome, should get evaluated for occult cancer irrespective of age. Paraneoplastic antibodies detection doesn’t make major difference in management than tumour evaluation except RI antibodies.
Ovarian teratomas are the most common type germ cell tumour in adults. Mature ovarian teratomas are benign; they associated paraneoplastic syndromes, like anti-N-Methyl-D-Aspartate Receptor (NMDAR) encephalitis. Opsoclonus-ataxia syndrome in adults is due to both mature and immature teratomas.
Ovarian teratomas mostly commonly associated with anti NMDAR encephalitis paraneoplastic syndrome due to antibodies against teratoma associated NMDA receptor antibodies which has potential to cross blood brain barrier. Treatment principle is intravenous pulse steroids, plasmapheresis, or intravenous immunoglobulin in I-OMS.
The treatment of ovarian teratoma associated encephalitis opsoclonus myoclonus syndrome is consisting of aggressive immunotherapy, tumour resection, and control of ataxia and opsoclonus symptomatically. First-line immunotherapy includes intravenous corticosteroids, intravenous immunoglobulins, and plasma exchange. Second-line immunotherapy involves, intravenous rituximab, and mycophenolate mofetil, cyclophosphamide.
Review of literature confirmed that early tumour resection with immunotherapy significantly improves clinical outcomes and prevents further neurological deterioration. Tumour resection should be considered in all ovarian teratoma associated paraneoplastic syndrome even when patient is systemically unstable and progressive severe neurological symptoms.
Isolated immunotherapy may become ineffective over the course unless antigen source from ovarian teratoma is surgically removed.
Conclusion
Opsoclonus Myoclonus Syndrome ataxia (OMS) syndrome is a rare entity that may be secondary to a paraneoplastic, infectious, or idiopathic process. All young females with opsoclonus myoclonus ataxia syndrome, should thoroughly evaluated for underlying ovarian teratoma. NMDAR antibodies may be negative initially in ovarian teratoma associated, Serial check may show positive antibodies in serum. Aggressive immunotherapy with surgical resection of ovarian teratoma is main treatment principle which minimizes morbidity and will have better outcomes.
References
- Wong AM, Musallam S, Tomlinson RD, Shannon P, Sharpe JA (2001) Opsoclonus in three dimensions: Oculographic, neuropathologic and modelling correlates. J Neurol Sci 189:71-81.
[Crossref] [Google Scholar] [PubMed]
- Rucker JC, Ying SH, Moore W, Optican LM, Buttner-Ennever J, et al. (2011) Do brainstem omnipause neurons terminate saccades? Ann N Y Acad Sci 1233:48-57.
[Crossref] [Google Scholar] [PubMed]
- Mitchell WG, Wooten AA, O'Neil SH, Rodriguez JG, Cruz RE, et al. (2015) Effect of increased immunosuppression on developmental outcome of Opsoclonus Myoclonus Syndrome (OMS). J Child Neurol 30:976-982.
[Crossref] [Google Scholar] [PubMed]
- Pranzatelli MR (2017) Clinical immunologic features of 389 children with opsoclonus-myoclonus syndrome: A cross-sectional study. Front Neurol 8:468.
[Crossref] [Google Scholar] [PubMed]
- KlaasJP, Ahlskog JE, Pittock SJ, Matsumoto JY, Aksamit AJ, et al. (2012) Adult-onset opsoclonus-myoclonus syndrome. Arch Neurol 69:1598-1607.
[Crossref] [Google Scholar] [PubMed]
- Dalmau J (2007) Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 61:25-36.
[Crossref] [Google Scholar] [PubMed]
- Armangue T, Sabater L, Torres-Vega E, Martinez-Hernandez E, Arino H, et al. (2016) Clinical and immunological features of opsoclonus-myoclonus syndrome in the era of neuronal cell surface antibodies. JAMA Neurol 73:417-424.
[Crossref] [Google Scholar] [PubMed]
- Caviness JN (1995) The movement disorder of adult opsoclonus. Mov Disord 10:22-27.
[Crossref] [Google Scholar] [PubMed]
- Pranzatelli MR (1996) The immunopharmacology of the opsoclonus-myoclonus syndrome. Clin Neuropharmacol 19:1-47.
[Crossref] [Google Scholar] [PubMed]
- Yaguchi H, Tsuji T, Yabe I, Hirayama E, Nomura T, et al. (2020) Incidence of anti-NMDAR encephalitis in patients undergoing resection of ovarian teratoma in a single institution. J Neurol Sci 409:116608.
[Crossref] [Google Scholar] [PubMed]
- Sheridan A, Kapur K, Pinard F, Dietrich Alber F, Camposano S, et al. (2020) IQ predictors in pediatric opsoclonus myoclonus syndrome: A large international cohort study. Dev Med Child Neurol 62:1444-1449.
[Crossref] [Google Scholar] [PubMed]
- Shamssili S, Grefkens J, de Leeuw B, van den Bent M, Hooijkaas H, et al. (2003) Paraneoplastic cerebellar degeneration associated with antineuronal antibodies: Analysis of 50 patients. Brain 126:1409-1418.
[Crossref] [Google Scholar] [PubMed]
- ArmangueT, Titulaer MJ, Sabater L, Pardo‐Moreno J, Gresa‐Arribas N, et al. (2014) A novel treatment-responsive encephalitis with frequent opsoclonus and teratoma. Ann Neurol 75:435-444.
[Crossref] [Google Scholar] [PubMed]
- Gorman MP (2010) Update on diagnosis, treatment, and prognosis in opsoclonus-myoclonus-ataxia syndrome. Curr Opin Pediatr 22:745-750.
[Crossref] [Google Scholar] [PubMed]
- Hasegawa S, Matsushige T, Kajimoto M, Inoue H, Momonaka H, et al. (2015) A nationwide survey of opsoclonus-myoclonus syndrome in Japanese children. Brain Dev 37:656-660.
[Crossref] [Google Scholar] [PubMed]
- BatallerL, Graus F, Saiz A, Vilchez JJ (2001) Opsoclonus-myoclonus study group. Clinical outcome in adult onset idiopathic or paraneoplastic opsoclonus-myoclonus. Brain 124:437-443.
[Crossref] [Google Scholar] [PubMed]
- Kanno K, Kin S, Hirose M, Suzuki S, Watanabe T, et al. (2015) Opsoclonus-ataxia syndrome associated with ovarian mature teratoma. J Obstet Gynaecol Res 41:1149-1153.
[Crossref] [Google Scholar] [PubMed]
- Lou E, Hensley ML, Lassman AB, Aghajanian C (2010) Paraneoplastic opsoclonus-myoclonus syndrome secondary to immature ovarian teratoma. Gynecol Oncol 117:382-384.
[Crossref] [Google Scholar] [PubMed]
- Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, et al. (2008) Anti-NMDA-receptor encephalitis: Case series and analysis of the effects of antibodies. Lancet Neurol 7:1091-1098.
[Crossref] [Google Scholar] [PubMed]
- Smith JH, Dhamija R, Moseley BD, Sandroni P, Lucchinetti CF, et al. (2011) N-methyl-D-aspartate receptor autoimmune encephalitis presenting with opsoclonus myoclonus: Treatment response to plasmapheresis. ArchNeurol 68:1069-1072.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi