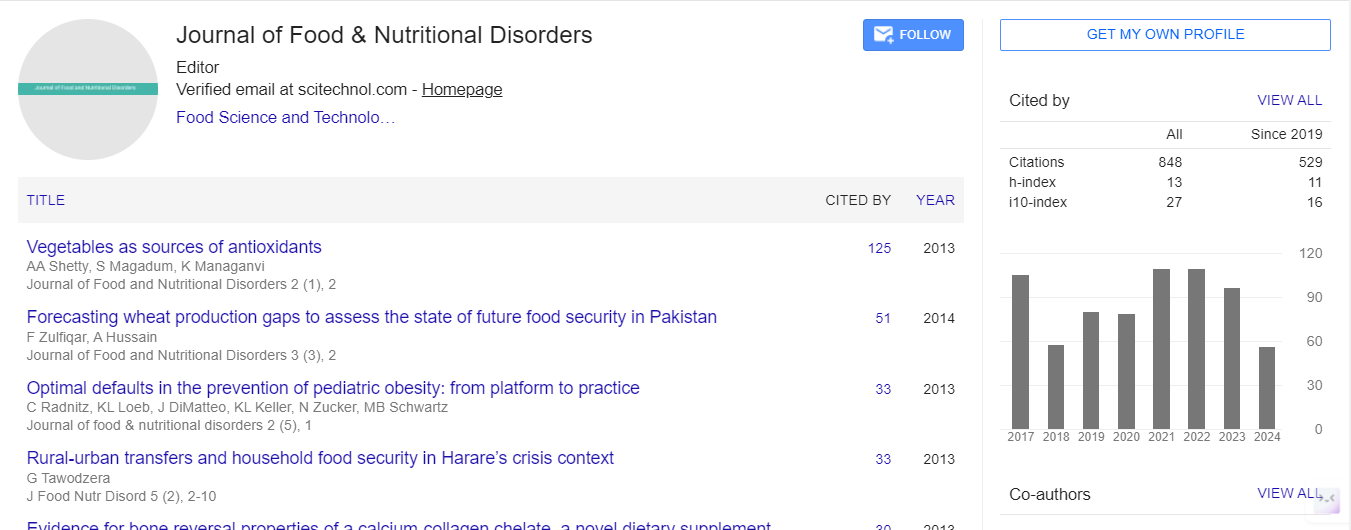
Research Article, J Food Nutr Disor Vol: 7 Issue: 2
Binge Eating Disorder (BED):Nutritional Prevention and Treatment
Julia Maria Melo Granje*
Diet Personnel Course and Nutritional Care, Center of Extension Courses and Post-Graduation Lato Sensu, Estacio de sa University, Brazil
*Corresponding Author : Julia Maria Melo Granje
Diet Personnel Course and Nutritional Care, Center of Extension Courses and Post-Graduation Lato Sensu, Estacio de sa University, Brazil
Tel: (21) 9.8121-3429
E-mail: nutrijuliagranje@yahoo.com.br
Received: March 23, 2018 Accepted: April 12, 2018 Published: April 17, 2018
Citation: Granje (2018) Binge Eating Disorder (BED): Nutritional Prevention and Treatment. J Food Nutr Disor 7:2. doi: 10.4172/2324-9323.1000248
Abstract
The Binge Eating Disorder (BED) is the food disorder with higher prevalence in the world’s population when compared with the classical entities Bulimia and Anorexia Nervosa. In this disorder, the person eats an excessive amount of food, losing control over what and how much is eaten, followed by feelings of guilt, shame, and/or disgust, with no use of compensatory methods. As the prognosis of BED is often found in people
seeking treatment for weight loss, it is important that nutritionists know how to identify and conduct the correct procedures when dealing with this disorder. The objective of this study was to conduct a literature review on the role of nutrition in procedures on the prevention and on the treatment
of BED. Prevention of BED is possible by early identification of behaviors, especially food behaviors, prior to the development of this disorder. The use of screening questionnaires, body image and the research on family history are important ways to identify risk factors for BED. The awareness about diets and encouraging a healthy diet with regular schedules individualized or in groups can help in preventing BED. Binge Eating treatment should be performed by a multidisciplinary team and Nutrition’s professional are responsible for adapting the eating patterns of patients. The use of food diary and guidelines on healthy eating aimed at weight loss or not, showed positive results and should be adopted by nutritionists for the treatment of Binge Eating Disorder.
Keywords: Periodic eating disorder, Eating disorders, Nutrition therapy, Nutrition; Obesity
Introduction
Feeding is linked to both physiological and emotional factors. The act of eating involves not only the sensory properties and nutritional value of foods for the energetic maintenance of the human body, but also involves feelings about what, when, how, when and how, is eaten. Thus, eating is a learned and modifiable behavior that can bring positive or negative changes throughout life [1].
Periodic Eating Disorder (BED) is an eating disorder characterized by the ingestion of too much food in a short time (two hours), accompanied by a lack of control of what and how much one eats, followed by feelings of guilt, shame and/or disgust [2,3]. Unlike Bulimia Nervosa, there are no compensatory methods in BED after the Food Compulsion (ACE) episodes [1].
First described by Stunkard, BED is strongly associated with obese individuals, since obesity can lead to compulsive consumption of food as a compensatory mechanism for their emotional condition, their psychological suffering due to their physical appearance and excessive preoccupation with weight. Binge eating appears to be also partially responsible for failures in the treatment of obesity [3].
However, BED is not exclusively a disorder of the obese, and is also found in several population groups, from children and adolescents [4], to adults of both genders, including eutrophic individuals [3], overweight, obese and pregnant women [5].
As a consequence, individuals with BED may be at increased risk of comorbidities such as obesity, hypertension, depression, as well as other physical and mental disorders [6]. In pregnant women, it may also cause fetal macrosomia and a higher probability of performing cesarean section surgery [5].
In the case of a disorder whose prevalence transcends the classic entities Anorexia Nervosa and Bulimia Nervosa [7], which is found in about 30% of the population seeking treatment for weight loss [8], binge eating episodes should be screened and their risk subgroups identified so that intervention programs and interdisciplinary actions can be created to prevent and treat BED. Because it is a disorder that involves both physical and mental consequences, every approach to these patients must cover these two aspects. With this, interdisciplinary therapies for these individuals are necessary, potentially covering all the factors involved in obesity and the Food Compulsion to reestablish the health conditions of this population [9].
Studies have shown that many prognoses for BED are performed in people seeking treatment for weight loss [8], making it important for the nutrition professional to know how to deal with the disorder, both to identify it in the patients who seek it, to present a behavior according to its treatment, to identify groups at risk and to act in order to prevent the development of the disorder [10].
There are many articles found in the literature aimed at the psychological and pharmacological treatment of BED, but there is a need to explore multidisciplinary prevention and treatment, especially in relation to nutritional behavior. Austin [11] found that 77% of the articles found were written by psychology and psychiatry departments and 5% had some association with public health, confirming the shortage of documents that aim at the nutritional prevention of eating disorders, especially in relation to BED.
Thus, this review aims to establish the relationship of nutrition with the prevention and treatment of Periodic Eating Disorder.
Methods
An electronic search was carried out on the sites of scientific publications: Pubmed, Scielo, Highwire, Lilacs and Periodicals of Capes. Separate or combined words and phrases were used: "Periodic Eating Disorder", "BED", "BED and nutrition", "treatment", "prevention"; and their respective translations into English. We selected articles that present texts pertinent to the objective of this work, whose publications dated from 2004 to 2014.
Literature Review
Definition of periodic eating disorder
Although initially described in 1959, Periodic Compulsive Eating has gained evidence since its publication in Appendix B of the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) in 1994 [12], when it was classified as "Eating Disorder Not specified "as a new diagnostic category that lacks further studies [2]. In this manual, diagnostic criteria for Periodic Eating Disorder were proposed, such as: Recurrent Eating Disorder episodes (ACE), characterized by the ingestion of an excessive amount of food followed by the lack of control; At least three parameters that indicate a loss of control (eating faster than normal, eating until you feel full, eating too much even if you are not hungry, eating yourself out of shame about how much you eat, and feeling ashamed, sad or guilty after the episode of compulsion); Feeling distressed by bouts of binge eating; ECA occurs on an average for 2 days per week for 6 months; And lack of compensatory behaviors for weight loss (such as purging and use of laxatives) and not being associated with the presence of Anorexia Nervosa and Bulimia Nervosa.
TCAP was then approved for inclusion in DSM-5, published in May 2013, as a new eating disorder group, different from the previous publication. The purpose of this modification was to raise awareness about differences between Periodic Eating Disorder and the phenomenon of overeating, most commonly found in the population. Although "Overeating" is a challenge for many people, BHT is a less common, more serious disorder and is associated with more severe physical and psychological problems.
Periodic Eating Disorder is defined as recurrent episodes of ingestion of a large amount of food in a short period of time, accompanied by a sense of loss of control, and followed by feelings of guilt, disgust, and / or shame. Individuals with BED tend to eat more food in up to two hours than people in similar circumstances. In addition, they tend to eat faster than normal and usually eat alone because of the shame of the amount of food consumed. ACE is not followed by compensatory mechanisms of weight control, occurs once on an average in a week for three months and is usually associated with depression and anxiety [9].
Studies have shown that a considerable percentage of obese individuals seeking treatment for weight loss have ECA [9], and BED is often associated with obesity. A fact justified by this population being more affected by psychopathological symptoms such as: low selfesteem, high levels of depression, panic syndrome, personality disorders and anxiety; Disorders positively linked to Eating Disorder. Obese individuals tend to be concerned about shape and body weight, and have a negative body image, having strong stimuli for excessive food intake. Obesity alone poses risks to health and, when accompanied by Eating Disorder, these risks are even greater [13].
Goldschimidt et al. [4] found that not only adults but also overweight children are associated with higher risks of eating disorders, including binge eating, since that type of group will be positively associated with behaviors such as weight and shape of the body, self-imposed restrictive diets and other unhealthy weight management methods.
Although BED is generally related to overweight and obese individuals, people with adequate weight, regardless of age and gender, are also affected by the disorder. Motivational mechanisms seem to be more related to the severity of the symptoms of this Eating Disorder than the weight gain itself [14].
In physiological terms, the hypothalamic-pituitary-adrenal (HHA) axis is of great importance in BED. Stress, among many other motivational factors for compulsive behavior, caused by psychosocial pressures or psychic and / or physical problems, activates the HHA axis, leads to an increase in plasma cortisol. Which leads to an acceleration of the energy metabolism that stimulates food intake, and may contribute to ECA frames [2]?
The abuse of alcohol and psychoactive substances, psychological comorbidities such as depression, anxiety, stress [3], and events [2] appear to be part of the risk factors associated with eating disorders, including BED. In addition to these, dissatisfaction with body image and oscillation of body weight in short periods of time is highlighted. The latter is the consequence of restrictive diets performed with the purpose of rapid weight loss due to dissatisfaction with the body. However, self-imposition and the habit of restrictive diets appear to have a rebound effect, resulting in cycles of loss and weight gain, which leads to health losses, including culminating in compulsive eating behavior [3].
The diagnosis for Periodic Eating Disorder should be performed by qualified medical and psychiatric professionals. Published papers related to BED describes that there are well-defined criteria for the diagnosis of BED. For this, it would be necessary for RCTs to occur at least twice a week over a period of 6 months and to be associated with some characteristics related to loss of control, in addition to the absence of compensatory behaviors [2,3]. These criteria met DSM-IV. With the publication of DSM-5, the frequency of binge eating episodes has been shortened, now being once a week for the past 3 months.
To assist in the diagnosis, questionnaires were created to identify behavior characteristics of BED. The Patient Health Questionnaire (PHQ) is a questionnaire used to identify eating disorders, and composes two blocks of questions whose answers may be "yes" or "no". In the first block, the questions are common for Bulimia Nervosa and BED. Individuals whose responses are positive for all questions in the first block are classified as suspected BED [1]. Another questionnaire used is the Binge Eating Escale (BES), already validated for the Portuguese language as Periodic Feed Compulsion Scale by Freitas et al. [15]. This instrument, although poorly associated with the diagnosis, is of great utility in identifying the severity of binge eating [9,15]. The Questionnaire for Eating and Weight Patterns-Revised (QEWP-R), was validated in the Portuguese version, deals with aspects related to the TCAP according to DSM-IV. It is a questionnaire that evaluates suspicions of Periodic Eating Disorder in spite of not very sensitive to diagnosis. It should be noted that such questionnaires are used as a screening for odisturbia, and the official diagnosis should be made after a clinical interview [16].
Epidemiology of TCAP
Epidemiological data reveals the prevalence of 0.7% to 5% of BED in the general population [1,3,7]. The percentages found for binge eating episodes in adolescent’s ranges from 18.5 to 24% [3] and in the age range of 17-55 years is 13 to 18.1%. In the present study, we found that 20% of cases with a diagnosis of BED in individuals presenting with ACE [3]; Mascarenhas et al. [1] reported 5-30% of obese individuals seeking treatment for obesity and 15-22% in individuals generally seeking treatment for weight loss in Brazil [3]. These data confirms the periodic eating disorder as a more frequent disorder than the classic entities Anorexia and Bulimia Nervosa [7].
In a study carried out with 1209 youngsters from 14 to 19 years old, in Cuiabá, 1.8% of them was included in the diagnosis of BED. The estimated prevalence of binge eating episodes was 24.6%, with the majority observed in females aged 19 years. The study also indicated that the higher the adolescent's weight, the greater the likelihood of developing binge eating episodes. In addition, the use of alcoholic beverages, more than three times a month, and fluctuation of weight in short periods were factors associated with BED [3].
Mascarenhas et al. [1] in a study of 2506 adults in Bahia found a prevalence of 5.02% of BED. The disorder affected a larger number of individuals whose monthly income was below a minimum wage. And, although there was no statistical significance, the Periodic Eating Disorder had a higher prevalence in the female sex.
Although most studies find a higher prevalence of BED in women, men are also affected by this disorder. "The clinical picture and therapeutic response of eating disorders are similar in both sexes, and in males constitute a challenge for diagnosis" [17]. This can be attributed to the lack of epidemiological studies that include males, to the belief that eating disorders are unique in women, or to their low prevalence in men [17]. However, the preoccupation with body image is still a determining factor to place women as a group at greater risk for the development of BED [1].
Along with females, young white people with a more favorable socioeconomic situation are also at the higher prevalence of Eating Disorders [1]. There are more studies that show [3] that individual of black race and lower economic class is diagnosed from eating disorders [1].
In a study of 5191 adults and 1170 black adolescents, in order to identify the prevalence of eating disorders and associated risk factors in this ethnic group, it was shown that the most common eating disorder in this population was the Periodic Eating Disorder, with a prevalence of 5.08 % in adults and 2.44% in adolescents. The study points out that despite the low rates of Anorexia Nervosa and Bulimia Nervosa in this population, numbers for BED were equal to or even higher than those found in studies with white individuals [6].
Patients undergoing bariatric surgery for weight loss may also present binge eating. Brazilian publications point to a prevalence of 16% of compulsive eating disorder in obese patients who undergo this medical procedure. Since it is a restrictive surgery, the amount of food consumed is dramatically reduced, which represents a high risk for compulsive patients, since adapting to this new food condition can be very difficult for them [18].
Chronic non-communicable diseases, such as Type 2 Diabetes Mellitus (IBD), also present significant cases of Papelbaum et al. [19] found in a study that patients with type 2 diabetes have prevalence of BED (Among 70 individuals evaluated, 10% of the individuals were observed with eating disorders). The result presented was attributed to factors related to diabetes. The authors suggested restrictive diets and the preoccupation with the corporal weight, regarding the treatment of the DMII, like a predisposition for the occurrence of episodes of binge eating.
Complications of BED associated with nutrition
Obesity and TCAP: It has already been known that patients with BED have body mass index (BMI) higher than those with Bulimia Nervosa. In addition to this they present a history of restrictive diets more variable than Bulimics [20]. Thus, studies have found that BED is related to obesity, since individuals with periodic binge eating tend to be more obese and have a history of weight fluctuation more pronounced than people outside this standard, in addition to the fact that the increase in adiposity has already been positively associated to the TCAP [20,21].
Despite the already established relationship, authors argue as to their nature. Overweight has already been associated as a cause and / or consequence of Periodic Eating Disorder. Obesity was described as a result of binge eating by Tirico et al. [22], which classified it as a physical impact that contributes negatively to the quality of life of individuals with BED. Taylor et al. [6] suggests that overweight and obesity are classified as symptoms of BED in the diagnostic criteria for African-Americans and Black Caribs. In the study, obesity was positively associated with comorbidity in cases of Periodic Eating Disorder. The high prevalence of overweight and obesity was in 60% of African American adults and 59% of black Caribbean adults. However, Machado et al. [18] points out that, in addition to the causal relationship between the disorder and excess body weight, with ACE being able to cause or facilitate obesity, and the degree of compulsion directly related to the degree of obesity, such as a nutritional condition may be a factor for periodic binge eating disorder. The authors justify that the emotional dynamics of obese individuals could generate the compulsive act. Fact also cited by Goldschimidt et al. [4], who states that overweight in childhood, is a risk factor for the development of eating disorders, such as BED. Thus, obesity seems to be both a cause or facilitator of BED, and a consequence of this disorder.
Obese individuals with Periodic Compulsive Eating have greater difficulties for weight loss; have worse responses and a higher drop-out rate for treatments for weight loss, and greater difficulty in maintaining lost weight [9,21].
Although it is strongly related to obesity, BED is not only a disorder of obese people, but is also found in groups whose body weight range is healthy [15]. Periodic compulsive eating does not seek to treat by individuals with adequate weight, which may be one of the factors that explain the lack of studies with this population group. It adds to the fact that research participants in this disorder usually have a long history of the disease. It is known that, in a large number of researches, the sample of participants is selected from those who seek treatment for BED or Obesity, which could explain why the samples of a large part of the studies tend to be performed with obese. BED cannot be underestimated in people with healthy weight. It is important to study eating disorders in people with BOD and normal body weight to determine appropriate interventions to reduce problematic eating habits and possibly prevents the development of obesity [14].
In a study carried out to compare clinical differences between obese and non-obese patients (with BMI within the appropriate range), it was found that the group with adequate weight used more methods of weight control (healthy and unhealthy)), than the obese group. Among the methods used, some could be part of a healthy life, such as physical exercise, but others could generate more episodes of binge eating, such as chronic performance of restrictive diets. The groups did not differ in frequency and age of onset of binge eating episodes, and distortion of body image. The publications points to the distinct behavior among individuals with BED whose weight is in the healthy range and obese individuals with the same disorder, and suggests that in clinical practice the behaviors in non-obese individuals with BED should be investigated, since this group could be at the risk of becoming obese over time [14].
Metabolic syndrome and BED: As a disorder that is strongly related to obesity and whose eating behavior is based on excessive food intake, alterations in biochemical tests and risks of chronic pathologies such as metabolic syndrome (MS) and cardiovascular diseases (CVD) are widely studied in individuals with TCAP.
Comparing a total of 207 obese individuals diagnosed with BED who did or did not have restrictive diets, Roehrig et al. [23] found an inversely proportional relationship between blood levels of triglycerides, HDL cholesterol and total cholesterol/HDL in subjects with those who had frequent restrictive diets, regardless of the patient's BMI. Therefore, it was suggested that although this eating behavior is associated with episodes of binge eating, weight gain and the "accordion effect" (effect that occurs when there is a weight loss followed by gain of body weight in a relatively short period of time), may be related to lower odds of metabolic abnormalities associated with cardiovascular disease risks than obese patients with BED who did not have restrictive diets frequently. Despite the results, the author emphasizes the need for further studies that may clarify or deepen the theme.
However, other studies point to the increase of metabolic risks, including high blood cholesterol levels [24] and dyslipidemia, in carriers and practitioners of eating-related behaviors [23,25]. Laboratory research reveals that increased feed rate is associated with central adiposity, elevated serum lipids, and hepatic steatosis in men and women. Metabolic abnormalities have been observed in healthy and lean women after ACE, which leads the study to suggest that metabolic dysfunction may be even more pronounced in obese individuals with binge eating who consume excessive calories habitually [26].
Metabolic syndrome (MS), characterized by a set of physiological disorders (central fat deposition, hypertriglyceridemia, hypertension, low levels of HDL cholesterol and high blood glucose linked to insulin resistance), is strongly associated with risk factors for cardiovascular diseases and consequently to a high mortality rate [25]. Because it is widely associated with obesity, it becomes the subject of studies also related to BED.
In 2009, a study comparing clinical outcomes between obese patients with BED, obese patients without BED, and non-obese patients without BED (control group) was presented for a 2.5-year follow-up at the Eating Disorder and Classification Conference in Washington. Individuals with Periodic Compulsive Disorder had the highest risk of developing any (i.e. at least one) component of the metabolic syndrome [26]. This finding was also found by Roehrig et al. [25] in their research with 93 obese individuals who met the criteria for diagnosis of BED. 60.2% of the participants presented SM. The publication indicates that the metabolic syndrome is common in this specific group of patients, and draws attention to the positive association found between MS and the habit of "skipping" meals; behavior that could be routinely targeted to patients by health professionals.
TCAP and diabetes mellitus II: Likewise, the relation between BED and Metabolic Syndrome, whose one of the components refers to insulin resistance, Periodic Compulsive Eating was also associated with Diabetes Mellitus.
In the literature, the prevalence of cases of BED in patients with type II diabetes mellitus (DMII) varies from 10-28.6% [7,27]. lATTERZA et al. [28] found in his study that one in five diabetic patients had some behavior related to eating disorders, with Periodic Eating Disorder being the most frequent disorder observed.
Dietary restriction resulting from treatment for DMII is one of the factors that may explain the predisposition of diabetic patients to the development of BED. Other risk factors are concern about body weight, depression and anxiety, also commonly found in these patients [27]. As a result, periodic dietary impairment in individuals with T2DM may adversely affect not only their weight but also their glycemic control [7], and may increase the risk of complications from type II diabetes [10].
Treatment for BED seems to positively influence the clinical picture of IBD. A study evaluating the effect for the treatment of BED in patients with type II diabetes demonstrated an improvement in glycemic control in patients who decreased the frequency of ACE [10]. Therefore, it is important to identify behaviors linked to Periodic Feeding Compulsion for better clinical management and, consequently, better evolution of the pathology [7].
TCAP and symptoms of gastrointestinal tract: Studies to explore Gastrointestinal Tract symptoms (GIT) in individuals with BED are scarce. A study conducted in Olmsted County, MN, with 4124 residents reporting ACE or presenting BED in order to analyze the gastrointestinal symptoms associated with Food Compulsion. BED was associated with the following symptoms: heartburn, acid regurgitation, dysphagia, bloating and abdominal pain, diarrhea, constipation, and dyskinesia (i.e. anal locking sensation). These associations were independent of BMI or the level of physical activity performed by individuals. The authors point out that although patients with BED have a greater gastric capacity than people without this disorder, which could suggest a protective effect against such symptoms, the reported manifestations may be due to the consumption of an even greater amount of food than the already stretched capacity of the stomach of an individual with BED. The type of food eaten during the compulsive episode may also influence the response of TGI, since individuals with this disorder usually give preference to foods with higher lipid content. The author indicates the need for further studies investigating the topic.
TCAP and bariatric surgery: Bariatric surgery, a medical procedure that reduces part of the stomach and/or intestine or promotes a decrease in gastric capacity, has been a way to reduce obesity and the associated comorbidities. Patients undergoing this operation are led to a restriction in food consumption. The idea of control and restriction of food intake may be a predisposing factor of BED, since b-alteration in eating behavior can trigger episodes of compulsive eating. Likewise, Food Compulsion is also considered as a risk factor in candidates for this surgery, since similar to the disorder developed after the procedure, can lead to postoperative complications and compromised the result of the operation [21]. Many patients who experience food compulsion prior to surgery have symptoms of the disorder reduced after surgery, especially in the first few months. However, the Food Compulsion may resurface, especially after 18 and 24 months postsurgery, as a continuous "pinch", followed by the lack of control over the consumption of hypercaloric foods [28].
To replace excessive and uncontrolled ingestion, patients undergoing bariatric surgery resort to the behavior of eating, in greater quantity, foods that are easier to eat and in short intervals of time. Study shows the highest consumption of sweets and snacks after the operation. Which leads to greater difficulty in weight loss and its maintenance? [21]
The literature also points to the relationship between nutritional deficiencies and psychiatric disorders. Bariatric Surgery is a restrictive procedure, which can lead to vitamin deficiencies and nutrients in patients who undergo this operation. These deficiencies can lead to the genesis of symptoms related to eating and psychic disorders. The deficiency of vitamins B9 and B12, for example, can lead to neurological and depressive symptoms, whereas the deficiency of iron and proteins is related to the appearance of depressive symptoms. Frequently, these deficiencies are underdiagnosed or neglected in patients undergoing bariatric surgeries, which favors the involvement of disorders such as BED [28,29].
Although it is not a factor impeding the operation, it is advisable to perform the identification and treatment of BED before performing bariatric surgery to favor postoperative evolution.
Nutrition Approach in the Periodic Food Completion Disorder
Relationship of nutrition with eating disorder
Knowledge of eating behaviors prior to the development of BED is necessary for the early identification of risk factors linked to the disorder [30]; As well as the awareness of the eating habits adopted after the installation of the disorder are essential for the donation of adequate nutritional conduits to the treatment of BED [30,31].
Restrictive diets: Restrictive diets are followed less by BED patients when compared to reports of patients with Bulimia Nervosa [13]. However, restrictive diets are often linked to dietary Compulsion.
Some studies have been conducted to specify the relationship between binge eating and restrictive diets. Research comparing the onset of binge eating prior to the restrictive diet, and vice versa, indicates that approximately 35-55% of patients had ACE before they started to undergo a dietary restriction regimen [15,32]. Grilo and Masheb [33] found an even more significant difference, with 81% of the sample studied having developed binge eating before dieting. In addition, the onset of BED seems to appear at earlier ages in the group whose compulsion precedes the diet [33].
However, the usual performance of restrictive diets also appears as predisposing to Periodic Eating Disorder. Adolescents on restrictive diets seem to be more likely to develop binge eating and body weight gain over time compared to young people for whom diet is not major concern [33,34].
Additionally, the literature reveals that many patients with BED have a long history of repeated attempts at weight loss through restrictive regimens. The difficulty of controlling food intake leads to binge eating behavior. Individuals with this eating pattern may continue to attempt weight loss through energy restriction, and sometimes acquire unhealthy compensatory behaviors, leading to Bulimia; or they can give up any attempts at weight loss through dieting because of repeated failures, but keeping the episodes of eating compulsively [18,19].
Golan [35] conducted a study with 207 obese individuals diagnosed with BED to explore how the frequency and time spent on dieting was related to behavioral and metabolic functions. The results showed that individuals on diets often started compulsive episodes, diets and obesity earlier, in addition to having more episodes of "concertina effect" than those who did not followed frequent diets. Although it did not present statistically significant differences, it was also noticed that the people who carried out diets usually presented higher levels of concern regarding feeding, dietary restrictions and distortions of body image.
It is added that unhealthy methods for weight loss, such as radical restrictive diets, are positively associated with depression, which in turn is related as a risk factor for BED.
Food consumption in TCAP: Patients with BED usually consume a significantly higher amount of food and calories during ACE than obese individuals without this disorder [19]. Symptoms such as depression and anxiety, often present in individuals with BED, appear to be related to increased energy intake in this public [8], and contribute to a lower weight loss in treatments for obesity, when compared to overweight individuals who do not present such symptoms [9].
Carvalho-Ferreira et al. [9] carried out a study in which objective and subjective factors related to Food Compulsion were observed. The result showed that the variations in anxiety were associated with variations in lipid consumption, which corroborates the idea that anxiety, widely found in individuals with BED, is linked to food consumption. The author points out the importance of multidisciplinary interventions in obese patients with binge eating in order to achieve the desired results.
Not only the amount of food intake, but its quality also differs in patients with BED [21]. In a study carried out with women of African - American and Hispanic/Latino BEDs, the results showed a positive association between fat consumption and the disorder in order to evaluate the relation between fruits, vegetables and fats consumed. The more severe the symptoms of compulsion, the greater the lipid consumption [35].
Increased fat intake was also observed in pregnant women presenting with BED both before and during pregnancy. The highest total energy consumption, of monosaturated and saturated lipids, was found. In addition, the women with BED presented lower intake of fruits and juices and higher intake of sweets and desserts based on milk than pregnant women without the disorder. Such dietary habits, including excess sugar consumed, may lead to excessive weight gain during pregnancy, gestational diabetes and adverse outcomes during childbirth [36,37].
Nutrition assistance in the prevention of BHT
In order to carry out a work of prevention of BHT, it is necessary for health professionals to initially investigate and identify the risk factors and symptoms associated with the disorder [9]. This evaluation should not be performed only for the purpose of diagnosis, but rather to evaluate the presence of behaviors linked to binge eating, in order to enable care management and prevention of the disorder [9,29]
There is concern that clinicians do not question or conduct an assessment routine in young people about the behaviors they use to control body weight, since such habits may be strong indications for the development of eating disorders, including Eating Disorder [33]. Equally important is the clinical evaluation of the weight control behavior adopted by individuals with eutrophic Body Mass Index (BMI), often neglected because BED is a disorder more related to being overweight. Such importance is due to individuals with BED, whose weight is considered healthy, to be at greater risk of becoming obese, since studies point to the weight gain of individuals with binge eating over time [4]. Chronic performance of restrictive diets, habitually skipping meals and fasting are examples of alarming behaviors for the development of BED and should be questioned during the assessment of health professionals [33].
Since it is a medical and mental pathology, BHT cannot be diagnosed by nutritionists, according to Law No. 8234 of September 17, 1991, which regulates the profession in Brazil. However, questionnaires can be used by a nutritionist to evaluate the presence and severity of symptoms related to the disorder [23,31,38,39], development or worsening of Periodic Eating Disorder; In addition, the patient is referred to a qualified professional for the diagnosis [9,23,30].
In this paper, we present a set of questionnaires that have been validated for the Portuguese language [40,41] and many are selfapplied questionnaires. In the present study, Self-administered surveys are easy to administer, economical and effective. They allow the patient to reveal behaviors that they consider shameful, which could be neglected in a face-to-face interview. However, concepts such as Periodic Feed Compulsion itself are difficult to evaluate accurately when using this type of investigation, according to Vitolo et al. [42]. The questionnaires used can identify BED or can provide measure of severity of the disorder and may also be used throughout the treatment for the evaluation of changes [41].
The Questionnaire on Eating and Weight Patterns (QEWP-R) was created with the purpose of providing the diagnosis of BED in clinical cases or populations of adults and adolescents, according to the criteria of the DSM-IV [3,34,41,42]. In addition to the TCAP identifier, this instrument addresses the subclinical Frames of Food Compulsion, related to loss of eating control and methods used for weight loss, and may also be used to differentiate Bulimia Purgative and Non Purgative Bulimine [3,41]. This is a questionnaire containing 27 selfadministered questions [40] or by interviews with trained professionals [41]. which determine ACE indicators, age at onset of RCTs [43], compensatory methods for weight loss, history of diets and body weight, degree of weight and body preoccupation [40,42] and family history of obesity [34]. The QEWP-R was validated in the Portuguese version by Freitas et al. [41]. Despite being modestly sensitive to the diagnosis itself, which should be confirmed later through a clinical interview, and if it proves to be inaccurate in the identification of individuals with absence of BED, QEWP-R has proved to be efficient as a predictive tool. In the present study, it was possible to identify the complications related to food compulsion and to an initial clinical evaluation [40].
A Binge Eating Scale (BES), translated into Portuguese and valid for the Brazilian population as a Periodic Feed Compulsion Scale (ECAP) [39] is a widely used instrument to identify the severity of Periodic Compulsive Eating in obese individuals [41]. It is a self-administered questionnaire containing 16 items that evaluate the behavioral, sentimental and cognitive manifestations involved in binge eating episodes [41]. Each question offers three to four weighted statements that in the end present a score ranging from 0-46, according to the respondent's choices [9]. The scores are then classified according to the severity of the Periodic Eating Disorder (CAP): ≤ 17 points are considered individuals without CAP, 18 to 26 points are considered individuals with moderate CAP, and ≥ 27 points are considered individuals with CAP grave [39]. Despite being not correlating with the criteria for BED presented in the DSM-IV, ECAP proved useful in the identification of individuals without CAP, as well as in the screening of obese individuals with CAP and their respective severity, making possible the adequate use of therapeutic conduits and followup during treatment; And observing the changes in the dietary behavior of patients during treatments for weight loss, at different moments [39].
The Patient Health Questionnaire (PHQ) is a simplified questionnaire designed to replace the Primary Care Evaluation of Mental Disorders (PRIME) in the identification of mental disorders, including BED. Validated by Spitzer et al. [43], it is a self-administered form with blocks of questions based on the criteria established by DSM-III and DSM-IV, referring to various mental disorders [43]. To access possible cases of Eating Disorders, two groups of questions that make up the food block are used. The first group refers to Bulimia and TCAP: "Do you usually feel that you cannot control what you eat and how much you eat?"; "Do you often eat, within a two-hour period, what most people would consider a large amount of food?"; "Has this occurred on average twice a week in the last three months?" The second group is composed of questions related only to Bulimia Nervosa.
It is considered as a suspected BFD that responds to all questions in group I and negatively to all questions in group II. Those who answered "yes" to the first three questions and at least one question from the second group are considered suspected of Bulimia [1,10] The PHQ showed a highly specific and sensitive questionnaire for the identification of Bulimia Nervosa and BED [1,10,43], being ideally administered in clinical practice as in patients who are suspected to be diagnosed with eating disorders, and in patients already in clinical follow-up, applied as part of a routine (eg annual) [43].
In addition to the semi-structured questionnaires validated for use in the diagnosis or identification of BED, other guidelines may be used for the same purpose. The Scottish Intercollegiate Network published in 2010 a guideline on the clinical management of obesity [33]. The publication suggests that health professionals should pay attention to patients with difficulties in weight loss, as these patients may present periodic eating disorders. In order to identify cases with suspected BED, the guideline suggests that a questionnaire with four questions, whose independent translation is found below, should be performed:
1) Are there times during the day when you cannot stop eating, even if you wanted to?
2) Have you ever found yourself eating an unusually large amount of food in a short amount of time?
3) Have you ever felt extremely guilty or depressed after this episode?
4) Have you ever felt more determined to diet or to eat healthier after this food event?
If the answer to all questions is "yes," the patient then suspects BED and should be referred to specialist professionals for the official diagnosis [33].
Body image: Dissatisfaction with body image may be a predictor for the development and maintenance of eating disorders, including BED, and therefore deserves clinical attention [22,44].
Stice et al. [44] conducted a survey of 2856 Brazilian men and women and concluded that in women, the presence of binge eating episodes was significantly correlated with the perception of body weight above the ideal regardless of the BMI they presented [44]. This shows that, because it is often a reflection of psychopathological factors such as low self-esteem, depression and extreme preoccupation with appearance, body dissatisfaction seems to be more related to BED than to excess weight itself [2].
A study carried out with female adolescents showed that dissatisfaction with body image was shown to be a predictive factor for the onset of binge eating [15]. In addition to the psychopathological factors derived from bodily dissatisfaction that could lead to BED as compensation for these feelings, another theory emerges that would explain this relationship. The hypothesis in question refers to the use of restrictive diets based on discontent with body image, since such behavior is often mistakenly seen as an effective form of weight control. However, as previously mentioned, the dietary restriction habit may be the trigger for the initiation of RCTs as a way to compensate for the low caloric intake [45].
To measure the level of dissatisfaction with body image, the Body Shape Questionnaire (BSQ) was created and validated for the Portuguese language by [40]. The questionnaire has 34 selfadministered items, each of which is rated on a scale of 1 to 6, where 1 means "never" and 6 means "always". The final score evaluates the degree of concern and anguish about body image [9]. The aim of the BSQ is to identify changes in body image is crucial for the identification of isolated symptoms of eating disorders since they precede the complete manifestation of the disorders [40].
Therefore, the approach of questions related to body image, including treatment protocols for overweight and obese individuals, can lead into better results and maintenance of the treatment for overweight, as well as predicting possible cases of BED [9].
Family history: A study by Hudson et al. [46] with 300 individuals, half of whom were identified with diagnostic criteria for BED, concluded that first-degree relatives of patients with binge eating were significantly more likely to present a diagnosis of BED than the relatives of the binge-eating group. In addition, parents of individuals with Periodic Compulsive Eating Disorder had higher BMI and higher obesity rates [46].
Another study, carried out by Javaras et al. [47], used data from the study by Hudson et al. [46] and the comparative data of twins, to estimate the degree of heritability of BED. The results showed that the family history had an estimate of 0.57 in the degree of heredity and the degree in the registry of the twins was of 0.39 which shows that the propensity of the development of BED can be controlled [47].
Thus, family history, already widely used by health professionals, can also be an important tool in the identification of risk factors associated with BED, and thus be useful in preventing this disorder. The initial investigation should look at family history first in firstdegree relatives and descendants, and then try to find patterns of behavior pattern in other relatives. Evidence should be sought for eating disorders and other disorders such as alcoholism, substance abuse, and cases of obesity [48].
Nutritional conduct in TCAP prevention: There was concern about Eating Disorder prevention programs actually introducing ideas that would encourage young people to promote dangerous strategies for weight management. However, recent studies have shown such unfounded concern, since such programs have indicated that they are effective in reducing the prevalence of Eating Disorders and in the development of obesity [23].
Data suggest that overweight patients actually wish to talk to health professionals about diets and physical activities. In this way, education about weight control, including information on the negative consequences of eating disorders, can prevent the development of risk behaviors for these disorders. Therefore, a sensible and frank approach to weight and eating issues in clinical practice is suggested [23]. Machado et al. [18] states that it is necessary to educate the patient that restrictive diets can lead to binge eating, and therefore should be directed not to perform random restrictions, such as excluding carbohydrate-rich foods from their diet [18]. In addition, guidance on eating regularly, without "skipping" daily meals (i.e. failing to perform one or more main meals of the day: breakfast, lunch, and dinner) should be encouraged by health professionals, especially nutritionists, for the prognosis and/or treatment of BED. Forced fasting and failure to perform main daily meals regularly increase the risk of other unhealthy weight-loss behaviors that can lead to eating disorders such as SCT (Interconnected Guidance Networks, 2010). In addition, binge eating seems to be also related to meal times. Studies suggest that individuals who ingest higher caloric intake in the morning (i.e., breakfast) show a decrease in total caloric intake during the day. On the other hand, those who consume a greater amount of calories during the night present an increase in the total caloric intake and a greater prevalence in the development of binge eating, which reinforces the idea that the orientation regarding the frequency and schedules of the meals should be stimulated for the prevention of BED [49].
Additionally, studies call attention to patients undergoing bariatric surgeries, which provide a restriction on excess diet, and consequent weight loss. In the present study, the effects of binge eating disorders on the onset of binge eating have been reported in the United States and Canada. Thus, nutritional follow-up is essential for patients who have undergone or will undergo this type of surgery, regardless of the existence or not of binge eating. Health professionals should be alert to the presence of binge eating symptoms following surgery, since patients with preoperative ACE are likely to develop BED within up to two years postoperatively. In addition, nutritional deficiencies, common in these patients, should be monitored supplemented with vitamins and minerals, since the lack of certain nutrients may lead to symptoms related to psychiatric and eating disorders such as BED [29].
In addition to this attention given to the clinical consultations carried out with the intention of preventing BED and eating disorders in general, it is also worth emphasizing the importance of preventive programs aimed at the population in a collaborative way. In their study with adolescents from public and private schools, Zanardi and Rumin [50] propose the implementation of educational actions, aimed at young students and school educators, to raise awareness about eating disorders. Knowledge about the design of eating disorders and the risks brought by the inadequacy of food consumption and its restriction may be preventive factors for the development of eating disorders in this population. The authors suggest the care of health professionals and school units so that health education is taken as constitutive of the educational process [50].
In addition to the guidelines on diet and weight loss control, the treatment for weight loss itself has been shown to be an effective way of preventing BED. Study shows that weight loss leads to a better profile of eating behavior and food intake, supposedly by altering during the weight loss process hormones that regulate these behaviors. Thus, weight loss proved to be efficient not only in avoiding the appearance of BED, but also in reducing symptoms related to Eating Disorder [9].
Nutrition assistance in the treatment of TCAP
Interdisciplinary and the role of nutrition in the treatment of BHT: Given the complexity of eating disorders, a multidisciplinary team, composed of mental health professionals (psychologists and psychiatrists), nutritionists and physicians, is necessary for the initial evaluation, treatment and follow-up of patients affected by these disorders [9,11]. It is important that the professionals from different health areas work in a team, coordinating with each other and conducts a quality treatment of Eating Disorders, including the TCAP [11].
The main objectives of treatment for BED are: to remit psychopathological symptoms related to binge eating (such as depression and anxiety) [51], avoid episodes of hyperphagia and establish healthy eating habits [2].
Many treatment methods have been studied to obtain the best form of therapeutic approach for BED [9], with the best results found in treatments involving psychological interventions and nutrients together [2,9,18]. Carvalho-Ferreira et al. [9], for example, points out that weight loss and the improvement of psychological symptoms seems to be useful for the reduction of Food Compulsion, and suggests that the nutritional therapy for weight loss is related to an improvement in eating behavior and consumption of food itself. Other studies, however, emphasize the need for drug therapy coupled with psychological and nutritional behaviors in order to obtain a positive result in the treatment of BED [2,51].
The nutritional treatment for BED is aimed at improving the patient's eating habits, assisting in the remission of binge eating episodes, improving the patient's relationship with food and his body [18] such as the weight loss aid for those who are overweight and obese [9]. The nutritionist who will deal with Eating Disorders must have knowledge and skills in the areas of psychology and psychiatry, as well as techniques inherent to Cognitive-Behavioral Therapy (CBT), thus facilitating the professional to create a bond with the patient, in an empathic, cooperative and flexible way [18].
Pharmacotherapy: The medicinal treatment for BED has been extensively studied. The classes of drugs with the best efficacy results, regarding the remission of symptoms of binge eating are antidepressants, appetite suppressants and anticonvulsants [2,51].
Depressive episodes are comorbidities notoriously seen in patients with BED, affecting about 51% of this population. Because of this, as well as the fact that Periodic Compulsive Disorder is a disorder with some clinical features similar to Bulimia Nervosa, the class of antidepressant drugs, especially selective serotonin reuptake inhibitors [2], has been studied as a form of treatment for BED) [51]. Desipramine, Fluoxetine, Fluvoxamine, and Venlafaxine are some of the investigated drugs that have shown positive results in the treatment of binge eating [51-53].
For being, BECC, often related to obesity, appetite-inhibiting drugs, or "anti-obesity agents" as described by [2], which act on the central nervous system affecting regions that regulate appetite and satiety, have been considered to be part of the list of drugs which were used in the treatment of Periodic Eating Disorder. D-fenfluramine and sibutramine have been shown to be effective in studies [51-53].
Some anticonvulsants can also act as appetite suppressants, promoting weight loss in some patients, and also act as mood stabilizers [2] and are, therefore, studied in the management of BED [51]. In this area, Topiramate [51-53], and Zonisamide [54] are highlighted.
It is worth noting that despite the positive results in the reduction of symptoms related to BED, pharmacotherapy has shown a short-term efficacy in placebo studies [55,56], being better administered with other types of therapies that address psychological and nutritional aspects [2,57].
Cognitive behavioral therapy: One of the most studied lines for the treatment of BED is Cognitive-Behavioral Therapy (CBT). It is a treatment, usually composed of 12 to 16 sessions, preferably administered by a multidisciplinary team [54]. It focuses on the cognitive aspect of the disorder, i.e. the distorted thoughts generated by BED (e.g., Body image dissatisfaction, low self-esteem, perfectionism); and behavioral aspects related to the inadequacy of eating habits [2]. Thus, CBT aids in the modification of eating habits through behavioral techniques, such as self-monitoring, stimulus control and problemsolving training, helping the patient to develop strategies for coping with difficulties without resorting to inappropriate eating behavior [18,21].
Studies have shown a remission in the frequency of binge eating in obese patients with BED who undergoes group CBT from 76% to 91% [21,57]. Due to its high efficacy, it is considered, therefore, the best treatment established for BED in the present time [55,58]. In a study of 21 obese patients diagnosed with BED, to evaluate the effectiveness of cognitive-behavioral therapy in a group, Duchesne et al. [57] found a reduction of RCTs, depressive symptoms and body dissatisfaction, in addition to a clinically significant weight loss, CBT is conducted and resulted in a significant improvement of symptoms associated with BED [57].
In addition to CBT alone, many studies investigate the results of Cognitive-Behavioral Therapy in conjunction with other treatments such as pharmacological therapies [21], nutritional guidelines [59], or nutritional therapy for loss of weight [55]. The results of these comparisons will be commented on in the next topics of this work.
Drugs x TCC: A large number of psychotherapies and pharmacotherapies have shown significant positive results in reducing binge eating and symptoms arising from BED [60]. Cecchini et al. [60] highlights the positive interaction that may exist between drug therapies and CBT, when performed concomitantly. The author points out that Cognitive-Behavioral Therapy could help patients in adhering to the medication, understanding and coping with the disorder. On the other hand, the drugs could help in the mental concentration, and thus facilitate the adherence of the patients to CBT [60]. However, few studies have found that aimed at comparing pharmacological therapies and CBT in the treatment of BED.
Grilo et al. [61] conducted a study with 102 individuals with BED to compare the efficacy of CBT, Fluoxetine, placebo, and combination therapy as a treatment for Periodic Compulsive Disorder. The results showed that CBT, unlike Fluoxentin, demonstrates greater efficacy in remission of the behavioral and psychological symptoms associated with BED. However, none of the methods used had a significant efficacy in weight loss, although the latter was positively associated with remission of binge eating [61].
In the eminence of leading to weight loss in a treatment for BED, Grilo et al. [62] performed a study with 50 adult patients with periodic eating disorders to evaluate the results obtained in the treatment of the disorder using the drug Orlistat, an appetite suppressant along with CBT, and CBT with placebo. The authors concluded that the therapy using CBT and Orlistat was more effective in patients' weight loss and remission of psychopathological symptoms of post-treatment disorder and follow-up 3 months later. However, the study has limitations, such as the short follow-up time of these patients. Thus, new studies with a greater follow-up for the maintenance analysis of both weight loss and remission of BED were suggested [62].
Despite the few articles found in the last ten years, some studies using drug therapies and CBT have been published previously, but although they have shown positive results regarding the reduction of symptoms related to BED, many reports do not produce significant results for weight loss [57], although this is significantly correlated with the total remission of binge eating [57]. In addition, there is a paucity of data in the literature that assesses follow-up on the maintenance and durability of drug treatments, making it difficult to conclude about its long-term effects on symptoms and weight loss in patients with TCAP [56].
Nutrition guidelines, weight reduction and CBT: Because BED is associated with the possibility of future metabolic complications, since it is a disorder frequently linked to obesity and weight gain, there is a need to ally the treatment of binge eating symptoms with the reduction of body weight [25]. Both treatment and prevention of BED and overweight share the same goals, which include healthy eating habits and behaviors, recognition of internal signs of hunger and satiety, and regular exercise [23].
Some studies have been conducted to evaluate the efficacy of remission of BED symptoms and weight loss using CBT associated with or focused on weight loss treatments [55,59,63].
Grilo et al. [55] conducted a study with 125 obese individuals with BED to evaluate the efficacy of three types of treatment: Cognitive Behavioral Therapy alone (CBT), Behavior Therapy for Weight Loss alone (CPT), and Cognitive-Behavioral Therapy of Behavioral Therapy for Weight Loss (TCC+TCPP). The observations conducted when the improvement of binge eating and BMI were performed after three months: Right after the treatment, with 6 months of follow-up, and with 12 months of follow-up. The highest remission of binge eating behavior shortly after treatment was found in the group undergoing CBT+TCPP. However, at 6 and 12 months of follow-up, this result was higher using CBT alone, although the values presented had no significant differences between treatments. The patients who presented the greatest decrease in BMI soon after treatment and with 6 months of follow up were those submitted to CBT+CPT. After 12 months of follow up there was no significant difference between the treatments. It was also observed that patients with 6 and 12 months of follow-up who achieved remission of binge eating had a higher rate of BMI decrease, which reinforces the idea that binge eating is correlated with weight loss. The authors conclude that although CBT and CPT are effective for the treatment of BED and its follow-up, they fail to produce substantial breasts. Therefore, they support the use of CBT as a treatment for BED, as well as TCPP as an alternative treatment, and emphasize the importance of withdrawal from compulsive episodes for weight loss [55].
Still in the eminence of studying the loss of weight allied to the treatment of BED, Fossati et al. [63] compared the application of CBT alone to the application of CBT with nutritional guidelines and CBT in conjunction with nutritional guidelines and exercise programs. The results showed a significant weight loss, as well as an improvement in the eating disorder, in the groups submitted to the nutritional programs. However, this result was even more expressive in the treatment that’s nutritional and physical education approach was performed [63].
Despite the correlation between body weight loss and remission of ACE, there is concern about the possibility that treatment for weight loss triggers behaviors that lead to the development of eating disorders. This is because weight loss is often achieved through restricted diets, which have previously been shown to be a risk factor for eating disorders [23,57]. However, studies indicate that the association of CBT with treatments for weight loss, including low-energy diets and/or nutritional guidelines, is showing positive results both in body weight reduction and in the reduction of binge eating [57].
A study was performed with participants who were diagnosed with periodic eating disorders, underwent two types of treatments: CBT along with treatment for weight loss, using a low energy density diet; and CBT along with general nutritional guidelines, unrelated to weight loss. Despite the non-statistically significant difference between treatments, there was a significant improvement in remission of binge eating, weight loss, waist circumference, blood pressure and blood cholesterol, as well as an increase in fruit and vegetable consumption and a decrease in fat intake, total calories and energy density in all subjects studied. The best results of weight loss and increased consumption of fruits and vegetables were observed in the group submitted to a low energy density diet. The study demonstrates that low-energy diets, when combined with CBT, may be conducive to the treatment of BED. It also highlights that nutritional strategies can be used in conjunction with CBT and may be successful in the treatment of BOD in obese patients [59].
In addition, studies with young people submitted to weight-loss treatments show positive results regarding adequate eating behavior [64,65], which corroborates with the assumption that treatments for weight loss do not seem to [57]. In the present study, there were no significant differences between the two groups. On the contrary, such programs seem to improve symptoms of eating disorders, such as decreased binge eating, improved body dissatisfaction as well as excessive preoccupation with physical appearance and body weight. However, it should be emphasized that treatments for weight loss in patients with BED should always be accompanied by therapies and professional follow-up that minimize the psychological symptoms of the disorder in order to achieve success in treatment [9].
Nutritional conduct in the treatment for TCAP: The role of the nutritionist in the treatment of Periodic Eating Disorder has as objectives the adequacy of changes in eating behavior, remission of ACE, promotion of healthy eating habits and improvement of the patient's relationship with food [66,67]. Thus, it is the nutritionist's role to conduct nutritional guidelines and dieterotherapies aimed at obtaining and maintaining the healthy weight of the individual with BED, as well as correcting the biological consequences of overweight and obesity, as well as incorporating changes in behavior and the establishment of an adequate dietary standard [66].
Therefore, it is necessary, that the nutrition professional be able to collect accurate information about the patient's food history and establish a collaborative relationship with the patient in order to facilitate the approach of conflicts related to the disorder. Nutritional treatment should be conducted in conjunction with psychotherapeutic treatment, and should address general nutritional guidelines and/or interventions for gradual weight loss, unrelated behavior related to food and body weight, normalization of eating habits and development of strategies to assist the patient in dealing with social situations [67].
The food diary is a tool widely used by nutritionists in the treatment of eating disorders, and can also be used in cases of BED. It is a selfmonitoring instrument in which the patient records the types and quantities of food consumed, the times and places of meals, the presence of RCTs and feelings related to what was ingested, the company during meals, and perception of how much hunger he was feeling before eating and how much satiety he got after that meal [28,41]. The aim of this registry is to make the patient acquire a greater awareness about the various aspects of their disorder and thus acquire a greater control over their eating habits [28], besides providing information to health professionals on which situations will be used as a focus on the interventions [28,41]. However, Vitolo et al. [42] points out the possibility of uncertainty regarding the patients' records, since they could not able to log the data reliably, either because they do not write immediately after meals or because they have an influence on the ECA-related feelings that would mask the actual eating behaviors [42]. To minimize errors in recording data, nutritionists should instruct patients the appropriate reporting form in the food journal. For this, they should use home measures and familiarize individuals with these measures of volumes and portions [9].
Group or individual nutritional guidelines are also behaviors that were adopted by nutritionists in the treatment of BED. Topics such as changing eating habits, food pyramid information, food labels, weight loss diets, healthy food choices, and functional foods can be addressed [9].
Guidance about having regular meals without "skipping" meals (ie failing to perform one or more main meals daily: breakfast, lunch, and dinner) seems to be more a matter of emphasis in the treatment and / or prevention of Periodic Feeding Compulsion [43]. The habit of "skipping" meals has been associated with the development of risk behaviors for BAC [34] and higher rates of metabolic syndrome in obese patients with BED [43]. In addition, the patient should not carry out food restrictions, since these can lead to compulsive episodes [28].
In their study of obese patients with metabolic syndrome, Utter et al. [43] suggests that counseling for regular mealtime meals is a crucial component of Cognitive Behavioral therapy indicated for BED, since patients with this disorder consume at least 3 meals a day appears to weigh less and have fewer bouts of binge eating.
Encouragement to decrease fat consumption has been shown to be effective in the treatment of BED. Wilson et al. [36], after finding a significant relationship between fat consumption and binge eating symptoms in African American and Latina women, suggests that the reduction of fat intake may be a positive factor for the remission of BHT symptoms and may be promising in its treatment.
The multidisciplinary therapy, which includes a nutritional treatment program using dietary diary, group nutritional guidelines and individual nutritional care focused on reducing food consumption and on a balanced diet, was studied by Carvalho-Ferreira et al. [9] in obese patients with BED. A significant improvement in binge eating symptoms and body image dissatisfaction was observed at the end of 6 months. There was also an expressive reduction in the consumption of total calories, lipids, saturated fat, carbohydrates and proteins, as well as an improvement in BMI, waist circumference and thoracic circumference. The results of this work suggest that interdisciplinary therapy is effective both in the physical and mental improvement of symptoms related to Eating Compulsion.
Despite the few written articles on nutritional treatment for BED, studies have shown the positive effect of incorporating nutritional interventions for eating disorders with symptoms common to BED. The incorporation of nutritional conducts, such as the food diary, concomitant with the multidisciplinary treatment, showed improvement or remission in symptoms such as ACE and body perception [28].
Conclusion
Periodic Compulsive Eating Disorder presents both physical and physical complications. Many of these physical complications are directly and indirectly related to the area of nutrition, and its knowledge is essential for the choice of lifestyle to be adopted both in the prevention and treatment of BED.
The nutritional prevention and treatment measures, together with the multidisciplinary treatments, have been effective in cases of binge eating, with the improvement or complete remission of symptoms related to this disorder. However, studies addressing the relationship between nutrition and BED are still scarce, and more work is needed to study the most effective nutritional interventions in cases of Periodic Eating Disorder.
References
- Mascarenhas MTL, Almeida MMGDe, Araujo TMDe, Prisco APK (2011) Eating disorders in the population from 20 to 59 years of Feira de Santana (BA). Cad Saude Colet 19: 179-86.
- Cortez CM, Araujo EA De, Ribeiro MV (2011) Periodic binge eating disorder and obesity. Catarinense MedArch 40.
- Pivetta LA, Gonçalves-Silva RMV (2010) Binge eating and associated factors among teenagers in Cuiabá, Mato Grosso State, Brazil. Cad Saude Publica 26: 337 -346.
- Goldschimidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, Wilfley DE (2008) Disordered Eating Attitudes and Behaviors in Overwheight Youth. Obesity 16: 257-264.
- Ulman TF, Holle AV, Torgersen L, Stoltenberg C, Reichbom-Kennerud T, et al. (2012) Sleep disturbances and binge eating disorder syntoms during and after pregnancy. Sleep 35: 1403-1411.
- Taylor JY, Caldwell CH, Baser RE, Matusko N, Faison N, et al. (2013) Classification and correlates of eating disorders among blacks: Findings from the National Survey of American Life. J Health Care Poor Underserved 24: 289-310.
- Palavras MA, Kaio GH, Mari JJ, Claudino AM (2011) A review of Latin American studies on binge eating disorder. Rev Bras Psiquiatr 33: S81-S108.
- Peterson RE, Latendresse SJ, Bartholome LT, Warren CS, Raymond NC (2012) Binge eating disorder mediates links between symptoms of depression, anxiety and caloric intake in overweight and obese women. J Obes.
- Carvalho-Ferreira JP De, Cipullo MAT, Caranti DA, Maschio DCL, Andrade-Silva SG, et al. (2012) Interdisciplinary lifestyle therapy improves bing eating symtoms and body image dissatisfaction in Brazilian obese adults. Trends Psychiatry Psychother 34: 223-233.
- Olivera GA, Fonseca PN (2006) Binge eating at the reception of health professionals. Psicol Hosp 4.
- Austin SB (2012) A public health approach to eating disorders prevention: It’s time for public health professionals to take a seat at the table. BMC Public Health 12: 854.
- Walsh BT (2011) The importance of eating behavior in eating disorders. Physiol Behav 104: 525-529.
- Bernardi F, Cichelero C, Vitolo MR (2005) Behavior of food restriction and obesity. Rev Nutr 18: 85-93.
- Goldschimidt AB, Le Grange D, Powers P, Crow SJ, Hill LL, et al. (2011) Eating disorder symptomatology in normal-weight vs. Obese individuals with binge eating disorder. Obesity 19: 1515-1518.
- Freitas S, Lopes CS, Coutinho W, Appolinario JC (2001) Translation and adaptation to Portuguese of the Binge-Eating Scale. Rev Bras Psychiatry 23.
- Borges MBF, Morgan CM, Claudino AM, Silveira DX (2005) Validation of the Portuguese version of the Questionnaire on Eating and Weight Patterns: revised (QEWP-R) for the screening of binge eating disorder. Rev Bras Psychiatry 27.
- Di Pietro MC, Lobao BF (2007) Eating disorders in men: Guide to Eating Disorders and Obesity.
- Vaz AR, Conceicao EM, Machado PPP (2009) The cognitive-behavioral approach in the treatment of eating disorders. Ana Psychology 27.
- Papelbaum M, Appolinario JC, Moreira RO, Ellinger VCM, Kupfer R, et al. (2005) Prevalence of eating disorders and psychiatric comorbidity in a clinical sample of type 2 diabetes mellitus patients. Ver Bras Psiquiatr Sao Paulo 27.
- Azevedo AP De, Santo CC, Fonseca DC (2004) Periodic binge eating disorder. J Clin Psy 31: 170-172.
- Duchesne M, Appolinario JC, Range BP, Fandino J, Moya T, et al. (2007) Use of manual-based cognitive-behavioral therapy in a Brazilian sample of obese individuals with periodic eating disorder. Rev Bras Psiquiatr 29: 23-25.
- Tirico PP, Stefano SC, Blay SL (2010) Quality of life and eating disorders: a systematic review. Cad Saude Publica 26: 431-439.
- Roehrig M, Masheb RM, White MA, Grilo CM (2009) Dieting frequency in obese patients with binge eating disorder: Behavioral and metabolic correlates. Obesity 17: 689-697.
- Wadden TA, Foster GD, Letizia KA, Wilk JE (1993) Metabolic, anthropometric and psychological characteristics of obese binge eaters. Int J Eat Disord 14: 17-25.
- Roehrig, M, Masheb RM, White MA, Grilo CM (2008) The Metabolic Syndrome and behavioral correlates in obese patients with binge eating disorder. Obesity 17: 481-486.
- Taylor AE, Hubbard J, Anderson EJ (1999) Impact binge eating on metabolic and lepetin dynamics in normal Young women. J Clin Endocrinol Metab 18: 428-434.
- Wonderlich SA, Gordon KH, Mitchell JE, Crosby RD, Engel SG (2009) The validity and clinical utility of binge eating disorder. Int J Eat Disord 42: 687-705.
- Latterza AR, Dunker KLL, Scagliusi FB, Kemen E (2004) Nutritional treatment of eating disorders. Arch Clin Psych 31: 173-176.
- Gordon PC, Kaio G.H, Sallet PC (2011) Aspects of psychiatric follow-up of obese patients under bariatric treatment: a review. Arch Clin Psych 38.
- Cavalcanti AMTS, Moreno EAC, Frazao IS, Elvia J, Gabrielle J (2011) Risk signs associated with periodic binge eating disorder (BED): A look at the nursing students of the Federal University of Pernambuco-UFPE. Campo Grande-MS.
- Zanatta BM, Souza NPP, Oliveira MRM, Leandro-Merhi VA (2008) Dietary intake of obese people with or without binge eating disorder 51 nutritional monitoring or not. Rev Bras Nutr Clin 23.
- Muschell MP, Mitchell JE, Weller CL (1995) Onset of binge eating, dieting, obesity, and mood disorders among subjects seeking treatment for binge eating disorder. Int J Eat Disord 17: 395-401.
- Grilo CM, Masheb RM (2000) Onset of dieting vs. binge eating in outpatients with binge eating disorder. Int J Obes Relat Metab Disord 24: 404-409.
- Scottish Intercollegiate Guidelines Network (2010) Management of Obesity: A National Clinical Guideline.
- Golan M (2013) The journey from opposition to recovery from eating disorders: multidisciplinary model integrating narrative counseling and motivational interviewing in traditional approaches. J Eat Disord 1: 19.
- Wilson PL, O'connor DP, Bode S, Mama SK, Lee RE, et al. (2012) Relationship of fruit, vegetable and fat consumption to binge eating symptoms in African American and Hispanic or Latina women. Eat Behav Houston 13: 179-182.
- Amorim, AR, Lacerda EMA, Kac G (2007) Use and Interpretation of anthropometric indicators in the evaluation of the nutritional status of pregnant women: Nutr Epidemiol.
- Siega-Riz AM, Haugen M, Meltzer HM, Holle AV, Hamer R, et al. (2009) Nutrient and food group intakes of women with and without Bulimia Nervosa and Binge eating disorder during pregnancy. Am J Clin Nutr 87: 1346-1355.
- Souza NPP, Oliveira MRM, Motta DG (2005) Occurrence of periodic eating disorders in obese patients. 8th National Congress of Sban, Brazil.
- Di Pietro M, Silveira DX (2009) Internal validity, dimensionality and performance of the Body Shape Questionnaire scale in a population of Brazilian university students. Rev Bras Psychiatrist 31.
- Freitas S, Gorenstein C, Appolinario JC (2002) Assessment instruments for eating disorders. Rev Bras Psiquiatr 24.
- Vitolo MR, Bortolini GA, Horta RL (2006) Prevalence of binge eating in female university students in different fields of knowledge. Rev Psychiatry 28: 20-26.
- Spitzer RL, Kroenke K, Williams JB (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorder. Patient Health Questionnaire. JAMA 282: 1737-1744.
- Stice E, Presnell K, Spangler D (2002) Risk factors for binge eating onset in adolescent girls: a 2-year prospective investigation. Health Psychol 21: 131-138.
- Hudson JI, Lalonde JK, Berry JM, Pindyck LJ, Bulik CM, et al. (2006) Binge-eating disorder as a distinct familial phenotype in obese individuals. Arch Gen Psychiatry 63: 313-319.
- Javaras KN, Reichborn-Kjennerud T, Bulik CM, Pope HG, Hudson JI (2008) Familiality and heritability of binge eating disorder: Results of a case-control family study and a twin study. Int J Eat Disord 41: 174-179.
- Yager J, Powers PS (2010) Evaluation and determination of the initial approaches for the treatment of patients with eating disorders: Clinical Manual of Eating Disorders. Sao Paulo: Artmed Editora 51-81.
- Bernardi F, Harb ABC, Levandovski RM, Hidalgo MPL (2009) Eating disorders and circadian food pattern: a review. Rev Psychiatrist 31:170-176.
- Zanardi CM, Rumin CR (2009) Eating disorders and adolescence: evaluation among public and private school students. Omnia Saude 6: 01-12.
- Salzano FT, Cordas TA (2004) Pharmacological treatment of eating disorders. Rev Psychiatry Clin 31.
- Appolinario JC (2004) Periodic eating disorder: an emerging clinical entity that responds to pharmacological treatment. Rev Bras Psychiatry 26.
- Appolinario JC, McElroy SL (2004) Pharmacological approaches in the treatment of binge eating disorder. Curr Drug Targets 5: 301-307.
- Segal A (2012) Behavioral strategies in the treatment of obese with binge eating. ABESO 57.
- Grilo CM, Masheb RM, Wilson GT, Gueorguieva R, White MA (2012) Cognitive-Behavioral Therapy, Behavioral Weight Loss, and Sequential Treatment for Obese Patients with Binge Eating Disorder: A Randomized Controlled Trial. J Consult Clin Psychol 79: 675-685.
- Reas DL, Grilo CM (2008) Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity 16: 2024-2038.
- Duchesne MD, Appolinario JC, Range BP, Freitas S, Papelbaum M, et al. (2007) The use of a manual-driven group cognitive behavior therapy in a Brazilian sample of obese individuals with binge-eating disorder. Rev Bras Psychiatry 29: 80-92.
- Wilson GT, Wilfley DE, Bryson SW (2007) Psychological treatments of Binge Eating Disorder. Arch Gen Psychiatry 67: 94-101.
- Masheb RM, Grilo CM, Rolls BJ (2011) A randomized controlled trial for obesity and binge eating disorder: Low-energy-density dietary counseling and cognitive behavioral therapy. Behav Res Ther 49: 821-829.
- Cecchini FF, Bertini E, Martins MB, Rodrigues FML, Monson CA (2010) Cognitive-behavioral therapy as a co-intervention in the treatment of periodic eating disorder in obesity. Neurosciences 6.
- Grilo CM, Masheb RM, Salant SL (2005) Cognitive Behavioral Therapy Guided Self-Help and Orlistat for the treatment of binge eating disorder: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry 57: 1193-1201.
- Grilo CM, Masheb RM, Wilson GT (2005) Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: a randomized double-blind placebo-controlled comparison. Biol Psychiatry 57: 301-309.
- Fossati M, Amati F, Painot D, Haenni C, Golay A, et al. (2004) Cognitive-behavioral therapy with simultaneous nutritional and physical activity in obese patients with binge eating disorder. Eat Weight Disord 9: 134-138.
- Braet C, Tanghe A, Decaluwe V, Moens E, Rosseel Y (2004) Inpatient treatment for children with obesity: weight loss, psychological well-being, and eating behavior. J Pediatr Psychol 29: 519-529.
- Butryn ML, Wadden TA (2005) Treatment of overweight in children and adolescents: does dieting increase the risk of eating disorders? Int J Eat Disord 37: 285-293.
- Pisciolaro F, Azevedo AP (2010) Periodic Compulsory Eating Disorder: Nutrition in psychiatry. Porto Alegre: Artmed 167-179.
- Scherer AA, Ferrari F, Machado MAG, Renzetti F (2011) Ambutal: An interdisciplinary experience performed in the scope of eating disorders and obesity treatments in the greater Florianopolis, SC. Ceres 6: 163-174.
- Timerman F, Scagliusi FB, Cordas TA (2010) Follow-up of the evolution of body image disorders in patients with bulimia nervosa, throughout the multiprofessional treatment. Rev Psychiatry Clin 37.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi