Research Article, Dent Health Curr Res Vol: 9 Issue: 4
Association between Periodontal Disease, Aterosclerosis and Thickness of the Intimate-Medium Carotid Layer
Renata Gabriela Oliveira Cavalcanti, Ingrid Carla Guedes da Silva Lima, Laura de Fatima Souto Maior*, Luiz Alcino Monteiro Gueiros, Jair Carneiro Leao and Alessandra Albuquerque Tavares Carvalho
Department of Odontology, Federal University of Pernambuco, Recife, Brazil
- *Corresponding Author:
- Laura de Fatima Souto Maior
Department of Odontology,
Federal University of Pernambuco,
Recife,
Brazil;
E-mail: alessandra.atcarvalho@gmail.com
Received date: 14 May, 2020, Manuscript No. dhcr-23-10820;
Editor assigned date: 19 May, 2020, PreQC No. dhcr-23-10820 (PQ);
Reviewed date: 02 June, 2020, QC No. dhcr-23-10820;
Revised date: 04 August, 2023, Manuscript No. dhcr-23-10820 (R);
Published date: 01 September, 2023, DOI: 10.4172/2470-0886.1000166
Citation: Cavalcanti RGO, da Silva Lima ICG, de Fatima SLM, Gueiros LAM, Leao JC, et al. (2023) Association between Periodontal Disease, Aterosclerosis and Thickness of the Intimate-Medium Carotid Layer. Dent Health Curr Res 9:4.
Abstract
Background: Coronary heart disease has a major impact on global health, the potential morbidity and mortality and as periodontal diseases have a high prevalence in the present day. In addition, the two conditions share common risk factors, such as smoking, diabetes mellitus and age. The purpose of this study is to evaluate the association between periodontal disease, atherosclerosis and carotid intima-media thickness of the carotid artery.
Methods and findings: A cross-sectional observational study with a sample of patients from the emergency hospital university of Pernambuco (PROCAPE) was conducted anamnesis and periodontal evaluation through the plaque index, bleeding index, probing depth, gingival recession. The thickness of the intima-media thickness of the carotid artery (cIMT) was obtained by ultrasound. The sample consisted of 92 patients aged 19-82 years. The prevalence of periodontal disease index was 74.2% and 11.8% of gingivitis. In the bivariate analysis showed a statistically significant correlation between periodontal disease and the presence of atheromatous plaque, but this relationship was not maintained in the multivariate analysis. The presence of atheromatous plaques was higher in patients with moderate to severe periodontal disease.
Conclusion: There was a statistically significant correlation between the presence of periodontal disease and the presence of atheromatous plaques, as well as increased carotid intima-media thickness. However, this association was not verified in multivariate analyzes.
Keywords: Periodontal disease, Atherosclerosis, Gingivitis, Carotid intima-media thickness, Atheromatous plaque
Introduction
Periodontitis is a multifactorial disease characterized by the loss of supporting tissues of the teeth making possible the loss of teeth as well as allowing the entry of bacteria and their subprocesses into the bloodstream, which activate the host's immune and inflammatory response. Research involving the systemic implications of periodontitis has grown exponentially [1]. Epidemiological studies relate periodontal disease to several systemic pathologies, among them cardiovascular disease. One of the main causes of cardiovascular disease is atherosclerosis, which is defined as the progressive accumulation of lipids, macrophages, calcium, fibrotic tissue and other components in the coronary artery wall.
The suggested mechanism of the relationship between periodontitis and coronary disease consists in the release of inflammatory bacteria, endotoxins and cytokines into the bloodstream, which are derived from periodontal disease. Such agents may cause increased carotid intima-media thickness, atheromatous plaque formation and thromboembolytic events. Vascular and endothelial changes were seen in patients with periodontitis [2]. In fact, there are reports that oral bacteria and their by-products can spread in the bloodstream and can settle in the vascular wall. Atherosclerotic plaques were detected in DNA, RNA and antigens of a variety of bacterial buccal species. It is noteworthy that studies indicate that the association between periodontitis and atherosclerosis independent of other risk factors. There is evidence that periodontitis may contribute to endothelial dysfunction, a marker that is a substitute for atherosclerosis, since studies have associated low values for flow-mediated dilatation of the brachial artery, probably due to thickening of the carotid intima-media layer.
Cardiovascular disease is one of the leading causes of mortality in the world, accounting for 16.7 million deaths annually [3]. Nevertheless, periodontitis is considered a public health problem, given its high prevalence and its indication as a risk factor for cardiovascular disease by the European society of cardiology and The American heart association. Better understanding of the relationship between periodontitis and cardiovascular disease may necessitate the integration of periodontal treatment and maintenance into the public health system in order to prevent and treat cardiovascular disease. In addition, it can help provide a complete and personalized preventative medical approach. Therefore, the purpose of this study is to analyze the association between periodontal diseases, atherosclerosis and the thickness of the carotid artery intima-media layer and to correlate it with other common risk factors [4].
Materials and Methods
Type of study and sample
This is a cross-sectional observational study with a sample composed of 92 patients over 18 years of age attended at the university of Pernambuco emergency room (PROCAPE).
Interview and periodontal exam
Anamnesis and completion of a form with information on gender, age, medical history, smoking, oral hygiene habits and Body Mass Index (BMI) were performed. The intrabuccal physical examination was performed by a single dental surgeon previously calibrated and included assessment of oral and periodontal hygiene through plaque index, bleeding index, depth of probing, gingival recession, presence of furca lesion and dental mobility. The periodontal probe used was the UNC-15 (Hu-Friedy, Chicago) hand probe that was introduced parallel to the tooth, measuring six points (mesiovestibular, mediovestibular, distobuccal, mesiolingual, mediolingual, distolingual) in each tooth [5]. Recent data were obtained through previously requested examinations of cardiac risk markers and inflammatory markers.
Carotid ultrasound
In order to measure the thickness of the intima-media layer of the carotid artery, ultrasonography was performed by a PROCAPE cardiologist with the patient in the supine position and the ultrasound beam perpendicular to the structures to be visualized, in an environment with reduced and quiet luminosity [6]. The common carotid artery was evaluated for the thickness of its walls and for the presence or absence of atheromatous plaque and the maximum thickness was recorded.
Statistical analysis
The data were analyzed by the IBM SPSS 20 program, using descriptive statistical techniques and univariate, bivariate and multivariate inferential statistics techniques. In the univariate analysis the normality of the data was verified through the Kolmogorov- Smirnov and Shapiro-Wilk tests; in the bivariate, the correlation between the presence of atheromatous plaques and carotid intimamedia thickness versus periodontal disease was verified using the chisquare test and the Kruskal Wallis test, together with a multiple comparison of the mean of the orders [7]. Multivariate analysis was performed through logistic regression. The level of significance was 5%.
Results
In summary, PROCAPE patients in the study period presented the periodontal parameters as presented in Table 1, with averages for probing depth and insertion loss of 3.2 and 4.3 millimeters, respectively, platelet and bleeding rates were 40% and 27.2%, respectively.
| Periodontal parameter | Minimum | Maximum | Average | Deviation standard |
|---|---|---|---|---|
| Probing depth (mm) | 1.7 | 6.0 | 3.2 | 0.8 |
| Attachment loss (mm) | 2.4 | 8.8 | 4.3 | 1.3 |
| Plaque index (%) | 0.0 | 100.0 | 40.0 | 21.3 |
| Bleeding index (%) | 0.0 | 60.9 | 27.2 | 17.5 |
Table 1: Descriptive statistics of the periodontal parameters of patients assisted in the Pernambuco university cardiology emergency room-PROCAPE.
With the aid of Table 2, it can be verified that the prevalence of periodontal disease in PROCAPE patients was 74.2%. Gingivitis presented a prevalence of 11.8%. Among periodontal diseases, moderate chronic periodontitis was the most frequent, occurring in 38.8% of the patients in the sample. As to the extent of periodontal disease, it prevailed of the generalized type.
| Periodontal condition | Presence and extent of periodontal disease | Total % (n) | ||
|---|---|---|---|---|
| No periodontal disease % (n) | With periodontal disease | |||
| Localized % (n) | Generalized % (n) | |||
| Periodontal health | 14.0 (13) | 14.0 (13) | ||
| Gingivitis | 11.8 (11) | 11.8 (11) | ||
| Mild periodontitis | 3.2 (3) | 5.4 (5) | 8.6 (8) | |
| Moderate periodontitis | 6.5 (6) | 32.3 (30) | 38.8 (36) | |
| Severe periodontitis | 2.2 (2) | 24.7 (23) | 26.9 (25) | |
| Total | 25.8 (24) | 74.2 (69) | 100 (93) | |
Table 2: Distribution of frequencies of periodontal status of patients from the PROCAPE in the presence or absence of periodontal disease and scope thereof.
The correlation between periodontal disease and the presence of atherosclerotic plaque in the common carotid artery in the studied group is initially displayed through a bivariate analysis, summarized in Table 3. In this table, it appears that the presence of atherosclerotic plaque was more frequent in patients with moderate periodontal disease (88.9%) and severe periodontal disease (92%) than in patients without or with mild periodontal disease periodontal disease (68.8%), this being a significant difference at a level of 5%.
| Periodontal status | Atherosclerotic plaque presence | p value* | |
|---|---|---|---|
| No (%) n | Yes (%)n | ||
| No periodontal disease or mild periodontal disease | 31.2% (10) | 68.8% (22) | |
| Moderate periodontal disease | 11.1% (4) | 88.9% (32) | 0.04 |
| Severe periodontal disease | 8.0% (2) | 92.0% (23) | |
Note: *X2 test
Table 3: Frequency of atheroma in common carotid artery in patients assisted in PROCAPE according to his periodontal status.
However, in multivariate analysis, using logistic regression, periodontal disease showed no significant association with the presence of atheromatous plaque in the carotid artery. This occurred even with different statistical models and methods to make up to it and even varying the way of categorizing and treating periodontal disease quantitative variables in its original form or categorized mode. Illustrating this situation, Table 4 shows the summary data of a logistic regression model that includes variable periodontal disease along with other variables to estimate their effects on the probability of the presence of atherosclerotic plaques in carotid artery [8].
There is on the model in the table, the variables that had a significant effect on the level of 5%, on the probability of the presence of atheromatous plaques were only diabetes and thickness of each inner or middle carotid.
The other variables mentioned (except periodontal disease) in the model are those that were associated with the presence of atheromatous plaque in significant level (p<0.05) or close to it (p<0.20), the various models tested [9]. The model is the one best suited when it keeps the variable periodontal disease.
| Variables | p Value | OR* | CI 95% OR** |
|---|---|---|---|
| Diabetes | |||
| Without diabetes | 0.02 | 12.5 | 1.4-115.9 |
| Com diabetes | |||
| Thickness of the intima/media carotid | |||
| >1 mm | 0.04 | 9.6 | 1.0-92.3 |
| Up to 1 mm | |||
| Smoking habit | |||
| Never smoked | 0.23 | 2.9 | 0.5-16.6 |
| Smoker or ex-smoker | |||
| Total cholesterol ratio | |||
| Up to 200 mg / Dl | 0.28 | 2. | 0.5-15.0 |
| > 200mg/dL | |||
| Gingival bleeding index | |||
| Up to 25% | 0.18 | 3.8 | 0.5-27.9 |
| > 25% | |||
| Periodontal disease-PD | |||
| Without PD or with mild PD | 0.95 | ||
| Moderate PD | 0.77 | 1.3 | 0.2 – 8.8 |
| Severe PD | 0.88 | 1.2 | 0.1 – 13.9 |
Note: *Odds Ratio, with the first category of each variable as the reference. **95% confidence interval for the odds ratio
Table 4: Data summaries of logistic regression of the presence of atheromatous plaque in the common carotid in patients assisted in PROCAPE based on diabetes, thickness of the intima or media carotid, smoking, total cholesterol rate, gingival bleeding index and periodontal disease.
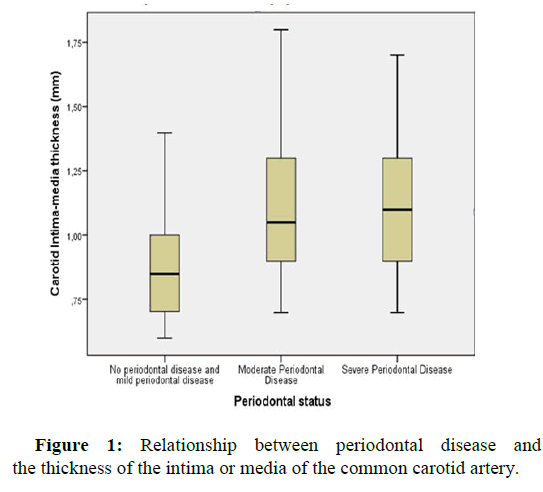
Regarding the relationship between periodontal disease and the thickness of the intima or media of the common carotid artery, a significant difference was identified in thicknesses of these layers among PROCAPE patients with various periodontal conditions (p=0.002 by the Kruskal Wallis test). According to multiple comparison of average orders, periodontal disease patients with no or mild disease presented reduced thickness (0.90 mm) than those with moderate periodontal disease (1.09 mm, p=0.002) and severe periodontal disease (1.11 mm; p=0.002). But the difference between these thicknesses patients with moderate to severe periodontal disease was not significant (p=0.76). Figure 1 illustrates these comparisons and differences [10].
In multivariate analysis, however, periodontal disease had no significant effect on the probability of occurrence of intima thickness or average carotid larger than 1 mm, even in different models and logistic regression methods. Table 5 presents a summary of the best adjusted model when it keeps the variable periodontal disease [11]. It appears that the most significant variable of this model (and also other tested) was C-reactive protein of interest. Also in this model the presence of atheroma, total cholesterol level and probing depth showed significant effect on the probability of occurrence of intima thickness or average carotid larger than 1 mm.
Note that the probing depth only showed a significant level of 5% when the reactive protein C rate was treated in a categorized way and at the 1% level when it itself was also categorized [12]. This, on the one hand, illustrates the non-linear relationships between variables (which justified the multivariate logistic regression-type, with the thickness of the intima or ormedia also treated in a categorized way) On the other hand, it points to a parameter associated with periodontal thickness of the intima or media of the carotid artery, regardless of the level of periodontal disease is not. Specifically, it is observed in Table 5, that a patient of the population studied in the survey of depth average that is greater than 3 mm is 11 times more likely to have a thickness of the intima or media of higher carotid than 1 mm.
| Variables | p Value | OR* | IC 95% OR** |
|---|---|---|---|
|
|
|||
| Without plaque | 0.04 | 11.7 | 1.1 -139.5 |
| With plaque | |||
| C-reactive protein rate | |||
| Up to 1 mg/dL | 0 |
14.3 | 1.9-105.0 |
| > 1 mg/dL | |||
|
|
|||
| 0.04 | 3.1 | 1.1- 9.1 | |
| Up to 200 mg/dL | |||
| >200 mg/dL | |||
|
|
|||
| 0.01 | 11.3 | 1.9-65.0 | |
| Up to 3 mm | |||
| >3 mm | |||
| Without PD or with mild PD | 0.30 | ||
| Moderate PD | 0.27 | 0.3 | 0.5-2.3 |
| Severe PD | 0.12 | 0.2 | 0.3-1.6 |
Note: * Odds Ratio, with the first category of each variable as the reference. ** 95% confidence interval for the odds ratio
Table 5: Summary data of logistic regression of the thickness of the intima or media of common carotid artery (up to 1 mm vs. >1 mm) in patients assisted in PROCAPE due to the presence of atheroma, c-reactive protein rate, total cholesterol rate, probing depth and periodontal disease.
Discussion
Periodontal disease is a public health problem and is highly prevalent today. In this study, there was a high prevalence of gingivitis and periodontitis among the subjects, which is in agreement with similar studies. 74.2% of the patients evaluated had periodontitis and 11.8% had gingivitis. The gingival bleeding index was 27.2%. Regarding the severity of periodontitis, the results corroborate with data from other studies in which there is a higher prevalence of moderate and severe periodontitis among the study population.
Several studies have shown the association between periodontitis and atherosclerotic cardiovascular diseases. The scientific literature states that the correlation between periodontal disease and atherosclerotic cardiovascular disease occurs independently of the presence of confounding risk factors. In this study, a statistically significant difference (p=0.04) was observed in relation to the association between periodontal disease and the presence of atheromatous plaques, with the presence of atheroma plaques being more frequent in moderate and severe periodontitis compared to individuals with periodontal health and mild degree of periodontal disease. However, after multivariate analysis, there was no significant association between periodontal disease and the presence of atheroma plaques in the carotid artery. Differently from the results of a study, which underwent a follow-up of three years, verifying that the progression atherosclerosis has a parallel relationship with the periodontal condition, both microbiologically and clinically. A study conducted in 2016 analyzed 86 patients and found a significant positive correlation between the variables: Depth of probing, gingival recession, clinical level of insertion and bleeding at the probing. The means of periodontal parameters in patients with obstructed arteries were significantly higher than those without coronary artery obstruction.
The association between these two diseases was confirmed by several studies, however it is worth mentioning that these studies present significant methodological variability. A meta-analysis analyzed 15 observational studies, which included a total of 17,330 patients, demonstrating that the presence of periodontal disease was associated with carotid atherosclerosis (OR: 1.27; 95% CI: 1.14-1.41) authors found substantial statistical heterogeneity (12=78.90%, p<0.0001), this fact may be related to the fact that these studies were carried out in different ethnicities. A large case-control study found that the risk of a first myocardial infarction was significantly higher in patients with periodontal disease, even after adjusting for confounding factors. These results reinforce the possibility of an independent relationship between periodontal disease and myocardial infarction. In a cross-sectional analysis of a large cohort study conducted in the Netherlands, it was found that 60,174 of the participants showed an independent association of periodontitis with atherosclerotic cardiovascular diseases.
Some articles address the link between periodontitis and endothelial dysfunction. The results demonstrate that periodontitis is associated with impaired endothelial function and that periodontal treatment may improve cardiovascular condition. The relationship between periodontitis and atherosclerosis has been described by two mechanisms: Caused directly by the periodontal pathogens or indirectly by bacterial components or inflammatory mediators. A third mechanism that would also support this connection is the relationship between periodontitis and lipid profile. Periodontal inflammation may adversely affect serum lipid control and also contribute to an increased risk of cardiovascular disease. In addition, lipid dysregulation would also increase susceptibility to periodontitis, as dyslipidemia is associated with a state of systemic inflammation. This suggests a possible bidirectional relationship between dyslipidemia and periodontitis.
Faced with these facts, one of the interests of cardiology is to find a surrogate marker for subclinical atherosclerosis. Ultrasonographic measurement of carotid artery intima-media thickness has been suggested as an alternative diagnostic feature. It is a very widespread method because it is non-invasive, low cost and without associated risks. The carotid ultrasound is able to visualize the first alterations of the walls of the arteries, monitoring arterial changes and their association with risk factors. This fact justifies the use of this test in the methodology of the present study, which verified that the carotid artery intimal layer in patients with moderate or severe periodontal disease presented thicker, statistically significant (p=0.002), in relation to patients with periodontal health or with mild periodontal disease. Dietrich in a systematic review, found that there is a significantly higher incidence of atherosclerotic cardiovascular disease in individuals with more severe periodontal disease when compared with individuals without periodontal disease or the mild degree of this pathology. The multivariate analysis of this study showed that the periodontal diagnosis did not present significant effects on the probability of occurrence of carotid intima-media thickness greater than 1 mm. The depth of the probing showed a significant effect (p=0.01) in relation to the thickness of the intima intimal layer greater than 1 mm. Probe depths greater than 3 mm increased 11.3 times the occurrence of an intima-media thickness greater than 1mm.
Unlike most studies, the non-correlation between periodontal disease and the presence of atheroma or increased carotid thickness after multivariate analyzes may be due to the age range of the study patients. A total of 92 patients participated, of which 38 (41.3%) were 60 years of age or older. And all age-stratified studies report stronger associations in younger individuals compared to older individuals. In fact, most studies failed to demonstrate an association between PD and cardiovascular disease incidence in older adults (>60-65 years). Unexpected or unanalyzed confounders may have occurred, genetic factors not yet known for susceptibility to cardiovascular disease. It is necessary to carry out longitudinal studies to obtain a deeper knowledge about these proposed hypotheses and mechanisms of action, as well as a causal relationship between these two diseases. Well-designed interventional studies are also needed to prove the effect of periodontal treatment on variables related to cardiovascular disease. The identification of these mechanisms will also enable new therapeutic alternatives that can have effects and be of potential use in both diseases [13].
Conclusion
There was a statistically significant correlation between the presence of periodontal disease and the presence of atheromatous plaques, as well as increased carotid intima-media thickness. However, this association was not verified in multivariate analyzes. There are several reasons that may justify the differences between the results of our study and previous studies. Among them, the diversity of methods used for both the diagnosis and measurement of periodontal disease and the resources to measure the thickness of the middle intima layer.
Conflict of Interest
All authors declare that there is no conflict of interest.
Funding
All the investment to carry out the research was being of all the responsibilities of the researchers.
References
- Tonetti MS, van Dyke TE (2013) Periodontitis and atherosclerotic cardiovascular disease: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J Clin Periodontol 84: S24-S29.
[Crossref] [Google Scholar] [PubMed]
- Monsarrat P, Blaizot A, Kemoun P, Ravaud P, Nabet C, et al. (2016) Clinical research activity in periodontal medicine: A systematic mapping of trial registers. J Clin Periodontol 43: 390-400.
[Crossref] [Google Scholar] [PubMed]
- Slocum C, Kramer C, Genco CA (2016) Immune dysregulation mediated by the oral microbiome: Potential link to chronic inflammation and atherosclerosis. J Intern Med 1: 114-128.
[Crossref] [Google Scholar] [PubMed]
- Gurav AN (2014) The association of periodontitis and metabolic syndrome. J Den Res 11: 1
[Google Scholar] [PubMed]
- Berlin‐Broner Y, Febbraio M, Levin L (2017) Association between apical periodontitis and cardiovascular diseases: A systematic review of the literature. Int Endod J 50: 847-859.
[Crossref] [Google Scholar] [PubMed]
- Mesa F, Magan-Fernandez A, Castellino G, Chianetta R, Nibali L, et al. (2019) Periodontitis and mechanisms of cardiometabolic risk: Novel insights and future perspectives. Biochim Biophys Acta Mol Basis DiS 1865: 476-484.
[Crossref] [Google Scholar] [PubMed]
- Sen S, Chung M, Duda V, Giamberardino L, Hinderliter A, et al. (2017) Periodontal disease associated with aortic arch atheroma in patients with stroke or transient ischemic attack. J Stroke Cerebrovasc Dis 26: 2137-2144.
[Crossref] [Google Scholar] [PubMed]
- Ziebolz D, Jahn C, Pegel J, Semper-Pinnecke E, Mausberg RF,et al. (2018) Periodontal bacteria DNA findings in human cardiac tissue-Is there a link of periodontitis to heart valve disease? Int J Cardiol 251: 74-79.
[Crossref] [Google Scholar] [PubMed]
- Desvarieux M, Demmer RT, Jacobs Jr DR, Papapanou PN, Sacco RL, et al. (2013) Changes in clinical and microbiological periodontal profiles relate to progression of carotid intima‐media thickness: The oral infections and vascular disease epidemiology study. J Am Heart Assoc 2: e000254.
[Crossref] [Google Scholar] [PubMed]
- Yu H, Qi LT, Liu LS, Wang XY (2014) Association of carotid Intima-media thickness and atherosclerotic plaque with periodontal status. J Dent Res 93: 744-751.
[Crossref] [Google Scholar] [PubMed]
- Dietrich T, Sharma P, Walter C, Weston P, Beck J (2013) The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J Periodontol 84: S70-S84.
[Crossref] [Google Scholar] [PubMed]
- Ketabi M, Meybodi FR, Asgari MR (2016) The association between periodontal disease parameters and severity of atherosclerosis. Dent Res J 13: 250.
[Crossref] [Google Scholar] [PubMed]
- Zeng XT, Leng WD, Lam YY, Yan BP, Wei XM, et al. (2016) Periodontal disease and carotid atherosclerosis: A meta-analysis of 17,330 participants. Int J Cardiol 203: 1044-1045.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi